Progeria physical examination: Difference between revisions
Jump to navigation
Jump to search
(Created page with "__NOTOC__ {{Xyz}} {{CMG}}; {{AE}} ==Overview== Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usua...") |
|||
| (29 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Progeria}} | ||
{{CMG}}; {{AE}} | {{CMG}}; {{AE}} {{VKG}} | ||
==Overview== | ==Overview== | ||
Common physical examination findings of [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) include skin changes, hair changes, eye problems and [[musculoskeletal]] abnormalities. | |||
==Physical Examination== | ==Physical Examination== | ||
===Appearance of the Patient=== | ===Appearance of the Patient=== | ||
*Patients with [ | *Patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) usually appear normal at birth.<ref name="pmid21251803">{{cite journal| author=Doubaj Y, Lamzouri A, Elalaoui SC, Laarabi FZ, Sefiani A| title=[Three cases of Hutchinson-Gilford progeria syndrome]. | journal=Arch Pediatr | year= 2011 | volume= 18 | issue= 2 | pages= 156-9 | pmid=21251803 | doi=10.1016/j.arcped.2010.11.014 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.Ffcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21251803 }}</ref> | ||
*Onset of symptoms usally occurs around 6-12 months in patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]). | |||
===Vital Signs=== | ===Vital Signs=== | ||
*High | *High [[blood pressure]] with normal [[pulse pressure]].<ref name="pmid182563943">{{cite journal| author=Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB et al.| title=Phenotype and course of Hutchinson-Gilford progeria syndrome. | journal=N Engl J Med | year= 2008 | volume= 358 | issue= 6 | pages= 592-604 | pmid=18256394 | doi=10.1056/NEJMoa0706898 | pmc=2940940 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18256394 }}</ref> | ||
===Skin=== | ===Skin=== | ||
< | * Skin examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) shows the following:<ref name="pmid20301300">{{cite journal| author=Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K et al.| title=GeneReviews® | journal= | year= 1993 | volume= | issue= | pages= | pmid=20301300 | doi= | pmc= | url= }}</ref><ref name="pmid9606327">{{cite journal| author=Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF et al.| title=Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology. | journal=Arch Dermatol | year= 1998 | volume= 134 | issue= 5 | pages= 577-9 | pmid=9606327 | doi=10.1001/archderm.134.5.577 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9606327 }}</ref><ref name="pmid18256394">{{cite journal| author=Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB et al.| title=Phenotype and course of Hutchinson-Gilford progeria syndrome. | journal=N Engl J Med | year= 2008 | volume= 358 | issue= 6 | pages= 592-604 | pmid=18256394 | doi=10.1056/NEJMoa0706898 | pmc=2940940 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18256394 }}</ref> | ||
** Skin atrophy | |||
** Skin dryness | |||
**Focal sclerotic and areas of laxity and outpouching of the skin | |||
**Rigid and tense skin with erosions | |||
**Intermittent hyperpigmentation along with hypopigmentation on the skin | |||
**Patients have indurated, shiny, inelastic skin | |||
**Aged-appearing skin due to the following: | |||
***Loss of subcutaneous fat(most commonly on the hands and feet) | |||
===HEENT=== | |||
* Abnormalities of the hair may include | |||
**Hair loss | |||
**Baldness | |||
=== | *progressive eyelashes loss | ||
* Facial features are very characteristic in patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) which include:<ref name="pmid96063272">{{cite journal| author=Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF et al.| title=Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology. | journal=Arch Dermatol | year= 1998 | volume= 134 | issue= 5 | pages= 577-9 | pmid=9606327 | doi=10.1001/archderm.134.5.577 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9606327 }}</ref><ref name="pmid22460337">{{cite journal| author=Ullrich NJ, Silvera VM, Campbell SE, Gordon LB| title=Craniofacial abnormalities in Hutchinson-Gilford progeria syndrome. | journal=AJNR Am J Neuroradiol | year= 2012 | volume= 33 | issue= 8 | pages= 1512-8 | pmid=22460337 | doi=10.3174/ajnr.A3088 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22460337 }}</ref><ref name="pmid22011502">{{cite journal| author=Chandravanshi SL, Rawat AK, Dwivedi PC, Choudhary P| title=Ocular manifestations in the Hutchinson-Gilford progeria syndrome. | journal=Indian J Ophthalmol | year= 2011 | volume= 59 | issue= 6 | pages= 509-12 | pmid=22011502 | doi=10.4103/0301-4738.86327 | pmc=3214428 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22011502 }}</ref> | |||
**Circumoral cyanosis with Thin lips | |||
**Mouth in O position | |||
* | **Prominent scalp veins | ||
* | **Prominent eyes | ||
* | **Fixed facial expressions | ||
* | **Beaked nose | ||
* | **pseudo hydrocephalus | ||
* | **Micrognathia(undersized jaw) | ||
* | **Retrognathia(abnormal posterior positioning of the maxilla or mandible) | ||
* | **Protruding ears with absent lobes | ||
* | **Frontal and parietal bossing | ||
* | **Large anterior fontanel | ||
* | |||
* | |||
* | |||
* | |||
* | |||
* Possible exposure keratopathy | |||
* Nocturnal lagophthalmos can be noticed in some patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) | |||
*Blepharophimosis<ref name="pmid96063273">{{cite journal| author=Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF et al.| title=Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology. | journal=Arch Dermatol | year= 1998 | volume= 134 | issue= 5 | pages= 577-9 | pmid=9606327 | doi=10.1001/archderm.134.5.577 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9606327 }}</ref> | |||
*Eruption of secondary incisors lingually and palatally in the mandible and maxillary area is noticed in patients with HGPS<ref name="pmid17908770">{{cite journal| author=Gordon LB, McCarten KM, Giobbie-Hurder A, Machan JT, Campbell SE, Berns SD et al.| title=Disease progression in Hutchinson-Gilford progeria syndrome: impact on growth and development. | journal=Pediatrics | year= 2007 | volume= 120 | issue= 4 | pages= 824-33 | pmid=17908770 | doi=10.1542/peds.2007-1357 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17908770 }}</ref> | |||
*Dental crowding and dental caries | |||
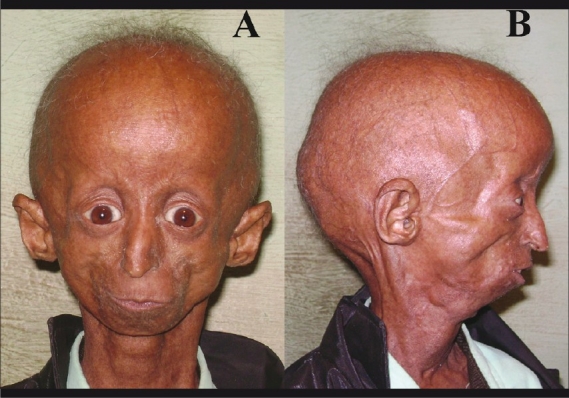
[[File:Hutchinson-Gilford progeria.jpg|thumb|Hutchinson-Gilford progeria male patient (A) showing disproportionately small face in comparison to the head, micrognathia, prominent eyes, both upper eyelids’ retraction, beaked nose, thin lips. (B) Prominent scalp veins, alopecia with grey and sparse hairs, and protruding ears with absent earlobe. Case courtesy by Dr. Shivcharan Lal Chandravanshi et al.<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214428/|title=Ocular manifestations in the Hutchinson-Gilford progeria syndrome|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]]<br /> | |||
[[File:Dental crowding and dental caries.jpg|alt=Dental crowding and dental caries|center|thumb|A) Upper jaw dental crowding and dental caries (B) Lower jaw dental crowding and dental caries. Case courtesy by Shivcharan L Chandravanshi<ref>{{Cite web|url=https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3214428/|title=Ocular manifestations in the Hutchinson-Gilford progeria syndrome|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref>]] | |||
<br /> | |||
===Neck=== | ===Neck=== | ||
* Neck examination of patients with | * Neck examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Lungs=== | ===Lungs=== | ||
* Pulmonary examination of patients with | * Pulmonary examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Heart=== | ===Heart=== | ||
* Cardiovascular examination of patients with | * Cardiovascular examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually shows dextrocardia. | ||
===Abdomen=== | ===Abdomen=== | ||
* Abdominal examination of patients with [ | * Abdominal examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Back=== | ===Back=== | ||
* Back examination of patients with [ | * Back examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Genitourinary=== | ===Genitourinary=== | ||
* Genitourinary examination of patients with [ | * Genitourinary examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Neuromuscular=== | ===Neuromuscular=== | ||
* Neuromuscular examination of patients with [ | * Neuromuscular examination of patients with [[Hutchinson-Gilford progeria syndrome]] ([[HGPS]]) is usually normal. | ||
===Extremities=== | ===Extremities=== | ||
* | * Musculoskeletal abnormalities which include:<ref name="pmid182563942">Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB et al. (2008) [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&retmode=ref&cmd=prlinks&id=18256394 Phenotype and course of Hutchinson-Gilford progeria syndrome.] ''N Engl J Med'' 358 (6):592-604. [http://dx.doi.org/10.1056/NEJMoa0706898 DOI:10.1056/NEJMoa0706898] PMID: [https://pubmed.gov/18256394 18256394]</ref><ref name="pmid96063274">{{cite journal| author=Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF et al.| title=Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology. | journal=Arch Dermatol | year= 1998 | volume= 134 | issue= 5 | pages= 577-9 | pmid=9606327 | doi=10.1001/archderm.134.5.577 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9606327 }}</ref><ref name="pmid179087702">{{cite journal| author=Gordon LB, McCarten KM, Giobbie-Hurder A, Machan JT, Campbell SE, Berns SD et al.| title=Disease progression in Hutchinson-Gilford progeria syndrome: impact on growth and development. | journal=Pediatrics | year= 2007 | volume= 120 | issue= 4 | pages= 824-33 | pmid=17908770 | doi=10.1542/peds.2007-1357 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17908770 }}</ref> | ||
**Thin limbs with prominent joints | |||
* | **Coxa valga | ||
* | **Measured reductions in joint range of motion | ||
* | **Osteoarthritis | ||
* | **Joint contractures | ||
* | **Pyriform (pear-shaped) thorax | ||
**Bilateral hip dislocations | |||
**Avascular necrosis of the femoral head | |||
==References== | ==References== | ||
Latest revision as of 14:00, 12 August 2019
|
Progeria Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Progeria physical examination On the Web |
|
American Roentgen Ray Society Images of Progeria physical examination |
|
Risk calculators and risk factors for Progeria physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vamsikrishna Gunnam M.B.B.S [2]
Overview
Common physical examination findings of Hutchinson-Gilford progeria syndrome (HGPS) include skin changes, hair changes, eye problems and musculoskeletal abnormalities.
Physical Examination
Appearance of the Patient
- Patients with Hutchinson-Gilford progeria syndrome (HGPS) usually appear normal at birth.[1]
- Onset of symptoms usally occurs around 6-12 months in patients with Hutchinson-Gilford progeria syndrome (HGPS).
Vital Signs
- High blood pressure with normal pulse pressure.[2]
Skin
- Skin examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) shows the following:[3][4][5]
- Skin atrophy
- Skin dryness
- Focal sclerotic and areas of laxity and outpouching of the skin
- Rigid and tense skin with erosions
- Intermittent hyperpigmentation along with hypopigmentation on the skin
- Patients have indurated, shiny, inelastic skin
- Aged-appearing skin due to the following:
- Loss of subcutaneous fat(most commonly on the hands and feet)
HEENT
- Abnormalities of the hair may include
- Hair loss
- Baldness
- progressive eyelashes loss
- Facial features are very characteristic in patients with Hutchinson-Gilford progeria syndrome (HGPS) which include:[6][7][8]
- Circumoral cyanosis with Thin lips
- Mouth in O position
- Prominent scalp veins
- Prominent eyes
- Fixed facial expressions
- Beaked nose
- pseudo hydrocephalus
- Micrognathia(undersized jaw)
- Retrognathia(abnormal posterior positioning of the maxilla or mandible)
- Protruding ears with absent lobes
- Frontal and parietal bossing
- Large anterior fontanel
- Possible exposure keratopathy
- Nocturnal lagophthalmos can be noticed in some patients with Hutchinson-Gilford progeria syndrome (HGPS)
- Blepharophimosis[9]
- Eruption of secondary incisors lingually and palatally in the mandible and maxillary area is noticed in patients with HGPS[10]
- Dental crowding and dental caries

Neck
- Neck examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Lungs
- Pulmonary examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Heart
- Cardiovascular examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually shows dextrocardia.
Abdomen
- Abdominal examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Back
- Back examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Genitourinary
- Genitourinary examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Neuromuscular
- Neuromuscular examination of patients with Hutchinson-Gilford progeria syndrome (HGPS) is usually normal.
Extremities
- Musculoskeletal abnormalities which include:[13][14][15]
- Thin limbs with prominent joints
- Coxa valga
- Measured reductions in joint range of motion
- Osteoarthritis
- Joint contractures
- Pyriform (pear-shaped) thorax
- Bilateral hip dislocations
- Avascular necrosis of the femoral head
References
- ↑ Doubaj Y, Lamzouri A, Elalaoui SC, Laarabi FZ, Sefiani A (2011). "[Three cases of Hutchinson-Gilford progeria syndrome]". Arch Pediatr. 18 (2): 156–9. doi:10.1016/j.arcped.2010.11.014. PMID 21251803.
- ↑ Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB; et al. (2008). "Phenotype and course of Hutchinson-Gilford progeria syndrome". N Engl J Med. 358 (6): 592–604. doi:10.1056/NEJMoa0706898. PMC 2940940. PMID 18256394.
- ↑ Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K; et al. (1993). "GeneReviews®". PMID 20301300.
- ↑ Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF; et al. (1998). "Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology". Arch Dermatol. 134 (5): 577–9. doi:10.1001/archderm.134.5.577. PMID 9606327.
- ↑ Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB; et al. (2008). "Phenotype and course of Hutchinson-Gilford progeria syndrome". N Engl J Med. 358 (6): 592–604. doi:10.1056/NEJMoa0706898. PMC 2940940. PMID 18256394.
- ↑ Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF; et al. (1998). "Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology". Arch Dermatol. 134 (5): 577–9. doi:10.1001/archderm.134.5.577. PMID 9606327.
- ↑ Ullrich NJ, Silvera VM, Campbell SE, Gordon LB (2012). "Craniofacial abnormalities in Hutchinson-Gilford progeria syndrome". AJNR Am J Neuroradiol. 33 (8): 1512–8. doi:10.3174/ajnr.A3088. PMID 22460337.
- ↑ Chandravanshi SL, Rawat AK, Dwivedi PC, Choudhary P (2011). "Ocular manifestations in the Hutchinson-Gilford progeria syndrome". Indian J Ophthalmol. 59 (6): 509–12. doi:10.4103/0301-4738.86327. PMC 3214428. PMID 22011502.
- ↑ Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF; et al. (1998). "Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology". Arch Dermatol. 134 (5): 577–9. doi:10.1001/archderm.134.5.577. PMID 9606327.
- ↑ Gordon LB, McCarten KM, Giobbie-Hurder A, Machan JT, Campbell SE, Berns SD; et al. (2007). "Disease progression in Hutchinson-Gilford progeria syndrome: impact on growth and development". Pediatrics. 120 (4): 824–33. doi:10.1542/peds.2007-1357. PMID 17908770.
- ↑ "Ocular manifestations in the Hutchinson-Gilford progeria syndrome".
- ↑ "Ocular manifestations in the Hutchinson-Gilford progeria syndrome".
- ↑ Merideth MA, Gordon LB, Clauss S, Sachdev V, Smith AC, Perry MB et al. (2008) Phenotype and course of Hutchinson-Gilford progeria syndrome. N Engl J Med 358 (6):592-604. DOI:10.1056/NEJMoa0706898 PMID: 18256394
- ↑ Smitt JH, van Asperen CJ, Niessen CM, Beemer FA, van Essen AJ, Hulsmans RF; et al. (1998). "Restrictive dermopathy. Report of 12 cases. Dutch Task Force on Genodermatology". Arch Dermatol. 134 (5): 577–9. doi:10.1001/archderm.134.5.577. PMID 9606327.
- ↑ Gordon LB, McCarten KM, Giobbie-Hurder A, Machan JT, Campbell SE, Berns SD; et al. (2007). "Disease progression in Hutchinson-Gilford progeria syndrome: impact on growth and development". Pediatrics. 120 (4): 824–33. doi:10.1542/peds.2007-1357. PMID 17908770.