Primary hyperparathyroidism: Difference between revisions
No edit summary |
m (Robot: Changing Category:Disease state to Category:Disease) |
||
| Line 87: | Line 87: | ||
{{Endocrine pathology}} | {{Endocrine pathology}} | ||
{{SIB}} | {{SIB}} | ||
[[sv:Primär hyperparatyreos]] | [[sv:Primär hyperparatyreos]] | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[Category:Endocrinology]] | |||
[[Category:Disease]] | |||
[[Category:Mature chapter]] | |||
Revision as of 22:31, 9 December 2011
For patient information click here
| Primary hyperparathyroidism | |
 | |
|---|---|
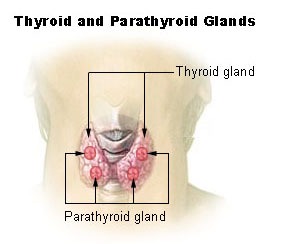
| Thyroid and parathyroid. | |
| ICD-10 | E21.0 |
| ICD-9 | 252.01 |
| DiseasesDB | 6283 |
| MeSH | D049950 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Phone:617-632-7753
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Primary hyperparathyroidism causes hypercalcemia (elevated blood calcium levels) through the excessive secretion of parathyroid hormone (PTH), usually by an adenoma (benign tumors) of the parathyroid glands. Its incidence is approximately 42 per 100,000 people. It is almost exactly three times as common in women as men.
Signs and Symptoms
The signs and symptoms of primary hyperparathyroidism are those of hypercalcemia. They are classically summarized by the mnemonic "stones, bones, abdominal groans and psychic moans".
- "Stones" refers to kidney stones, nephrocalcinosis, and diabetes insipidus (polyuria and polydipsia). These can ultimately lead to renal failure.
- "Bones" refers to bone-related complications. The classic bone disease in hyperparathyroidism is osteitis fibrosa cystica, which results in pain and sometimes pathological fractures. Other bone diseases associated with hyperparathyroidism are osteoporosis, osteomalacia, and arthritis.
- "Abdominal groans" refers to gastrointestinal symptoms of constipation, indigestion, nausea and vomiting. Hypercalcemia can lead to peptic ulcers and acute pancreatitis.
- "Psychic moans" refers to effects on the central nervous system. Symptoms include lethargy, fatigue, depression, memory loss, psychosis, ataxia, delirium, and coma.
- Left ventricular hypertrophy.[1]
Other signs include proximal muscle weakness, itching, and band keratopathy of the eyes.
Diagnosis
The diagnosis of primary hyperparathyroidism is made by blood tests. Serum calcium levels are elevated.
The serum chloride phosphate ratio is 33 or more in most patients with primary hyperparathyroidism. [2][3][4] However, thiazide medications have been reported to causes ratios above 33.[5]
Urinary cAMP is occasionally measured; this is generally elevated.
Parathyroid hormone activity
Intact PTH levels are also elevated.
Causes
The most common cause of primary hyperparathyroidism is a sporadic, single parathyroid adenoma resulting from a clonal mutation (~97%). Less common are hyperplasia of all parathyroid glands (~2.5%), parathyroid carcinoma (malignant tumor), and adenomas in more than one gland (together ~0.5%). Primary hyperparathyroidism is also a feature of several familial endocrine disorders: Multiple endocrine neoplasia type 1 and type 2A (MEN type 1 and MEN type 2A), and familial hyperparathyroidism.
In all cases, the disease is idiopathic, but is thought to involve inactivation of tumor suppression genes.
Complications
The classic bone disease in hyperparathyroidism is osteitis fibrosa cystica, which results in pain and sometimes pathological fractures. Other bone diseases associated with hyperparathyroidism are osteoporosis, osteomalacia, and arthritis.
Treatment
Treatment is usually surgical removal of the gland(s) containing adenomas.
Medications
Medications include estrogen replacement therapy in postmenopausal women and bisphosphonates. Bisphosphonates may improve bone turnover.[6]
Surgery
A consensus statement in 2002 recommended the following indications for surgery[7]:
- Serum calcium (above upper limit of normal): 1.0 mg/dl
- 24-h urinary calcium >400 mg
- Creatinine clearance reduced by 30% compared with age-matched subjects.
- Bone mineral density t-score <-2.5 at any site
- Age <50
More recently, three randomized controlled trials have studied the role of surgery in patients with asymptomatic hyperparathyroidism. The largest study reported that surgery showed increase in bone mass, but no improvement in quality of life after one to two years among patients with[8]:
- Untreated, asymptomatic primary hyperparathyroidism
- Serum calcium between 2.60 - 2.85 mmol/liter (10.4 - 11.4 mg/dl)
- Age between 50 and 80 yr
- No medications interfering with Ca metabolism
- No hyperparathyroid bone disease
- No previous operation in the neck
- Creatinine level < 130 µmol/liter (<1.47 mg/dl)
Two other trials reported improvements in bone density and some improvement in quality of life with surgery.[9][10]
Future therapies
Future developments such as calcimemetic agents (e.g. cinacalcet) which activate the parathyroid calcium-sensing receptor may offer a good alternative to surgery.
See also
References
- ↑ Stefenelli T, Abela C, Frank H; et al. (1997). "Cardiac abnormalities in patients with primary hyperparathyroidism: implications for follow-up". J. Clin. Endocrinol. Metab. 82 (1): 106–12. PMID 8989242.
- ↑ Reeves CD, Palmer F, Bacchus H, Longerbeam JK (1975). "Differential diagnosis of hypercalcemia by the chloride/phosphate ratio". Am. J. Surg. 130 (2): 166–71. PMID 1155729.
This study found a ratio above 33 to have a sensitivity of 94% and a specificity of 96%.
- ↑ Palmer FJ, Nelson JC, Bacchus H (1974). "The chloride-phosphate ratio in hypercalcemia". Ann. Intern. Med. 80 (2): 200–4. PMID 4405880.
- ↑ Broulík PD, Pacovský V (1979). "The chloride phosphate ratio as the screening test for primary hyperparathyroidism". Horm. Metab. Res. 11 (10): 577–9. PMID 521012.
This study found a ratio above 33 to have a sensitivity of 95% and a specificity of 100%.
- ↑ Lawler FH, Janssen HP (1983). "Chloride:phosphate ratio with hypercalcemia secondary to thiazide administration". The Journal of family practice. 16 (1): 153–4. PMID 6848626.
- ↑ Khan AA, Bilezikian JP, Kung AW; et al. (2004). "Alendronate in primary hyperparathyroidism: a double-blind, randomized, placebo-controlled trial". J. Clin. Endocrinol. Metab. 89 (7): 3319–25. doi:10.1210/jc.2003-030908. PMID 15240609.
- ↑ Bilezikian JP, Potts JT, Fuleihan Gel-H; et al. (2002). "Summary statement from a workshop on asymptomatic primary hyperparathyroidism: a perspective for the 21st century". J. Clin. Endocrinol. Metab. 87 (12): 5353–61. PMID 12466320.
- ↑ Bollerslev J, Jansson S, Mollerup CL; et al. (2007). "Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial". J. Clin. Endocrinol. Metab. 92 (5): 1687–92. doi:10.1210/jc.2006-1836. PMID 17284629.
- ↑ Ambrogini E, Cetani F, Cianferotti L; et al. (2007). "Surgery or surveillance for mild asymptomatic primary hyperparathyroidism: a prospective, randomized clinical trial". J. Clin. Endocrinol. Metab. 92 (8): 3114–21. doi:10.1210/jc.2007-0219. PMID 17535997.
- ↑ Rao DS, Phillips ER, Divine GW, Talpos GB (2004). "Randomized controlled clinical trial of surgery versus no surgery in patients with mild asymptomatic primary hyperparathyroidism". J. Clin. Endocrinol. Metab. 89 (11): 5415–22. doi:10.1210/jc.2004-0028. PMID 15531491.