Primary biliary cirrhosis: Difference between revisions
| Line 35: | Line 35: | ||
A liver biopsy is necessary to determine the stage of disease. | A liver biopsy is necessary to determine the stage of disease. | ||
===Other Diagnostic studies=== | ===Other Diagnostic studies=== | ||
Abdominal [[medical ultrasonography|ultrasound]] or a [[CT scan]] is usually performed to rule out blockage to the bile ducts. Previously most suspected sufferers underwent a [[liver biopsy]], and - if uncertainty remained - [[endoscopic retrograde cholangiopancreatography]] (ERCP, an [[endoscopy|endoscopic]] investigation of the [[bile duct]]). | Abdominal [[medical ultrasonography|ultrasound]] or a [[CT scan]] is usually performed to rule out blockage to the bile ducts. Previously most suspected sufferers underwent a [[liver biopsy]], and - if uncertainty remained - [[endoscopic retrograde cholangiopancreatography]] (ERCP, an [[endoscopy|endoscopic]] investigation of the [[bile duct]]). | ||
Revision as of 19:42, 16 April 2013
For patient information page on this topic, click here.
|
Primary Biliary Cirrhosis Microchapters |
|
Differentiating Primary Biliary Cirrhosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Primary biliary cirrhosis On the Web |
|
American Roentgen Ray Society Images of Primary biliary cirrhosis |
|
Risk calculators and risk factors for Primary biliary cirrhosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] Prashanth Saddala M.B.B.S
Synonyms and keywords: Chronic non-suppurative destructive cholangitis, PBC
Causes
Diagnosis
History and Symptoms
The following symptoms may be present in PBC:
- Fatigue
- Pruritus (itchy skin)
- Jaundice (yellowing of the eyes and skin), due to increased bilirubin in the blood.
- Association with an extrahepatic autoimmune disorder such as Rheumatoid Arthritis or Sjögren syndrome (up to 80% incidence).
Physical Examination
On physical examination, the following may be present
- Xanthelasmata (focal collections of cholesterol in the skin, especially around the eyes)
- Complications of cirrhosis and portal hypertension:
- Esophageal varices
- Fluid retention in the abdomen (ascites)
- Hepatic encephalopathy, up to coma, in extreme cases.
Laboratory tests
To diagnose PBC, distinctions should be established from other conditions with similar symptoms, such as autoimmune hepatitis or primary sclerosing cholangitis (PSC).
Diagnostic blood tests include:
- Deranged liver function tests (high alkaline phosphatase, elevated AST, ALT)
- Presence of certain antibodies: antimitochondrial antibody antinuclear antibodies like Anti-glycoprotein-210 antibodies, Anti-centromere antibodies, anti-sp100. (the M2-IgG antimitochondrial antibody is the most specific test)
Liver Biopsy
Primary biliary cirrhosis is characterized by interlobular bile duct destruction. Histopathologic findings of primary biliary cirrhosis include:[1]
- Inflammation of the bile ducts, characterized by intraepithelial lymphocytes, and
- Periductal epithelioid granulomata.
A liver biopsy is necessary to determine the stage of disease.
Other Diagnostic studies
Abdominal ultrasound or a CT scan is usually performed to rule out blockage to the bile ducts. Previously most suspected sufferers underwent a liver biopsy, and - if uncertainty remained - endoscopic retrograde cholangiopancreatography (ERCP, an endoscopic investigation of the bile duct).
Now most patients are diagnosed without invasive investigation since the combination of anti-mitochondrial antibodies (see below) and typical (cholestatic) liver function tests are considered diagnostic. However, a liver biopsy is necessary to determine the stage of disease.
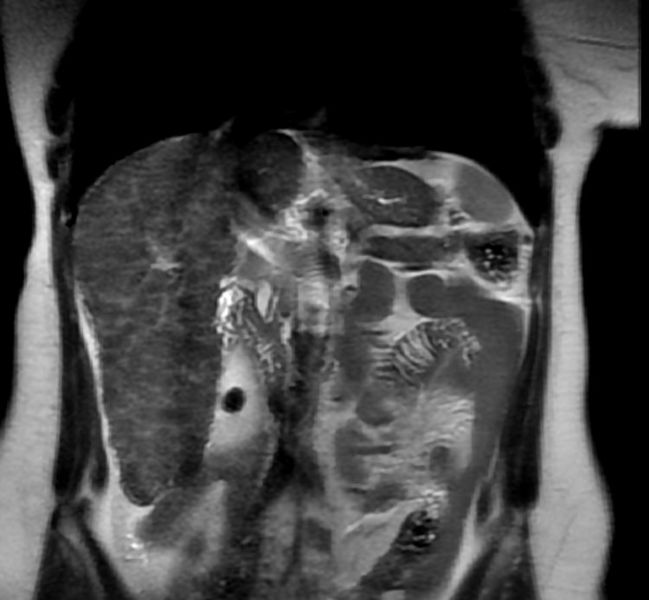
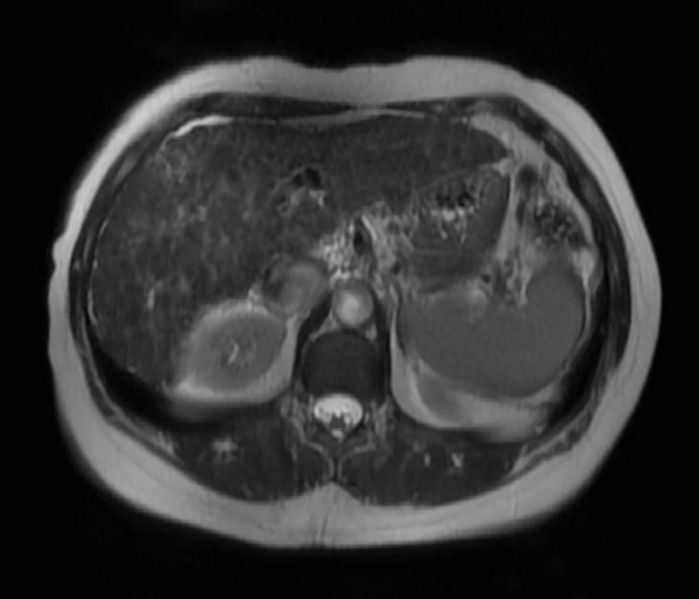
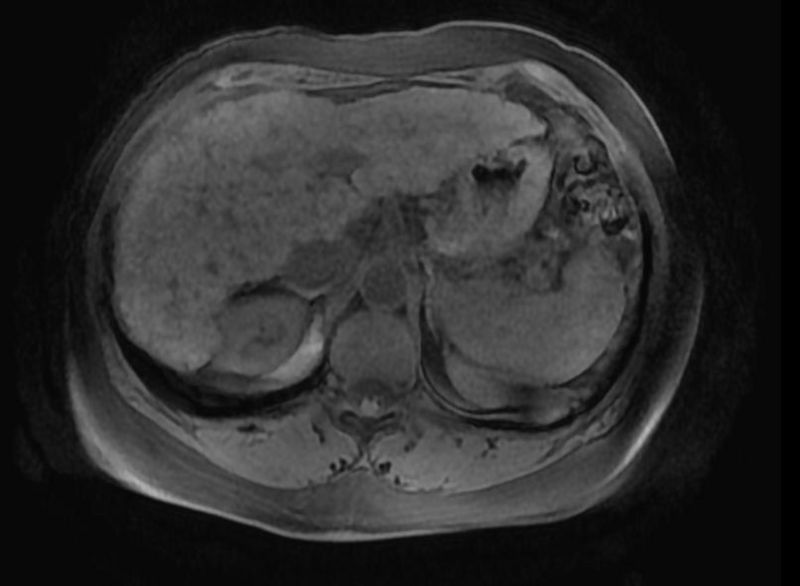
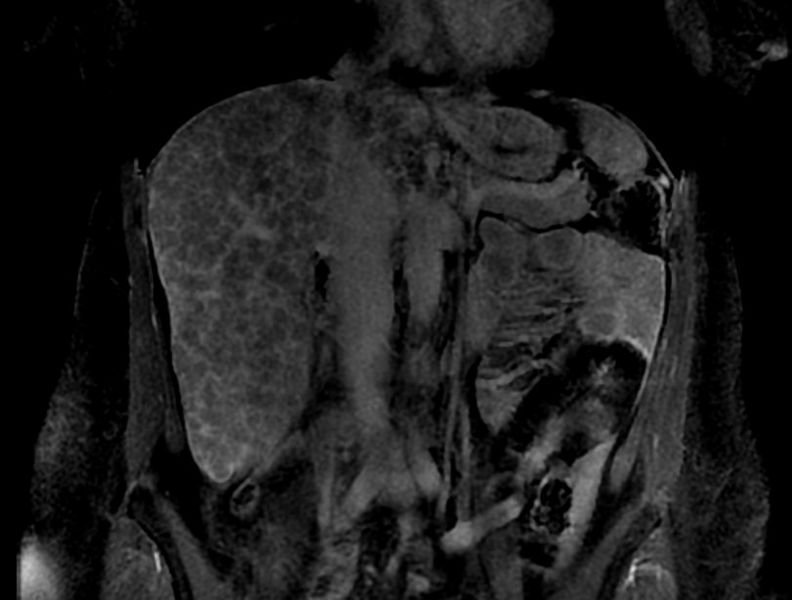
MR images of a patient with primary biliary cirrhosis
-
T2
-
T2Image:
-
T1 preImage:
-
T1 postImage:
-
T1 postImage:
-
T1 postImage:
-
T1 post
Therapy
There is no known cure, but medication may slow the progression so that a normal lifespan and quality of life may be attainable for many patients. Specific treatment for fatigue, which may be debilitating in some patients, is limited and currently undergoing trials.
- Ursodeoxycholic acid (Ursodiol) is the most frequently used treatment. This helps reduce the cholestasis and improves blood test results (liver function tests). It has a minimal effect on symptoms and whether it improves prognosis is controversial.
- To relieve itching caused by bile acids in circulation, which would normally be removed by the liver, cholestyramine (a bile acid sequestrant) may be prescribed to absorb bile acids in the gut and be eliminated, rather than re-enter the blood stream. Alternative agents include naltrexone and rifampicin.
- To relieve fatigue associated with primary biliary cirrhosis, current studies indicate that Provigil (modafinil) may be effective without damaging the liver.[2] Though off-patent, the limiting factor in the use of modafinil in the U.S. is cost. The manufacturer, Cephalon, has made agreements with manufacturers of generic modafinil to provide payments in exchange for delaying their sale of modafinil.[3] The FTC has filed suit against Cephalon alleging anti-competitive behavior.[4]
- Patients with PBC have poor lipid-dependent absorption of Vitamins A, D, E, K.[5] Appropriate supplementation is recommended when bilirubin is elevated[6]. Multivitamins (esp. Vitamin D) and calcium are also recommended.
- Patients with PBC are at elevated risk of developing osteoporosis[7] and esophageal varices[8] as compared to the general population and others with liver disease. Screening and treatment of these complications is an important part of the management of PBC.
- As in all liver diseases, alcoholic beverages are contraindicated.
As in all liver diseases, excessive consumption of alcohol is contraindicated.
In advanced cases, a liver transplant, if successful, results in a favorable prognosis. After liver transplant, the recurrence rate may be as high as 18% at 5 years, and up to 30% at 10 years. There is no consensus on risk factors for recurrence of the disease [9]
Obeticholic acid is in phase III clinical trials for PBC.[10]
References
- ↑ Nakanuma Y, Tsuneyama K, Sasaki M, Harada K (2000). "Destruction of bile ducts in primary biliary cirrhosis". Baillieres Best Pract Res Clin Gastroenterol. 14 (4): 549–70. doi:10.1053/bega.2000.0103. PMID 10976014. Unknown parameter
|month=ignored (help) - ↑ Modafinil#Primary_biliary_cirrhosis
Ian Gan S, de Jongh M, Kaplan MM (2009). "Modafinil in the treatment of debilitating fatigue in primary biliary cirrhosis: a clinical experience". Dig. Dis. Sci. 54 (10): 2242–6. doi:10.1007/s10620-008-0613-3. PMID 19082890. Unknown parameter|month=ignored (help)
Kumagi T, Heathcote EJ (2008). "Primary biliary cirrhosis". Orphanet J Rare Dis. 3: 1. doi:10.1186/1750-1172-3-1. PMC 2266722. PMID 18215315.Ref 157 viz:
Jones DE, Newton JL (2007). "An open study of modafinil for the treatment of daytime somnolence and fatigue in primary biliary cirrhosis". Aliment. Pharmacol. Ther. 25 (4): 471–6. doi:10.1111/j.1365-2036.2006.03223.x. PMID 17270003. Unknown parameter|month=ignored (help) - ↑ Modafinil#Patent_protection_and_antitrust_litigation
Carrier MA (2011). "Provigil: A Case Study of Anticompetitive Behavior" (PDF). Hastings Science & Technology Law Journal. 3 (2): 441–452. - ↑ http://www.ftc.gov/os/caselist/0610182/080213complaint.pdf
- ↑ Bruce R. Bacon; John G. O'Grady (2006). Comprehensive clinical hepatology. Elsevier Health Sciences. pp. 283–. ISBN 978-0-323-03675-7. Retrieved 29 June 2010.
- ↑ Lindor, KD (2009 Jul). "Primary biliary cirrhosis". Hepatology (Baltimore, Md.). 50 (1): 291–308. doi:10.1002/hep.22906. PMID 19554543. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Collier, Jane (2002). "Guidelines on the management of osteoporosis associated with chronic liver disease". Gut. 50: i1–i9. PMC 1867644. PMID 11788576.
|access-date=requires|url=(help) - ↑ Ali, AH (2011 Aug). "Varices in early histological stage primary biliary cirrhosis". Journal of Clinical Gastroenterology. 45 (7): e66–71. doi:10.1097/MCG.0b013e3181f18c4e. PMID 20856137. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Medical care of the Liver Trasplant Patient, 3rd Edition published 2006, editied by Paul G. Killenberg, page 429
- ↑ http://www.genengnews.com/gen-news-highlights/dainippon-sumitomo-pays-intercept-15m-for-phase-iii-liver-disease-drug/81244901/
Sources
Medical
- Online Mendelian Inheritance in Man (OMIM) 109720
- M. Eric Gershwin, John M. Vierling, Michael P. Manns, eds. Liver Immunology. Philadelphia, Pa.: Hanley and Belfus, 2003. ISBN 1-56053-499-0. (State of the art; technical.)
- Marshall M. Kaplan, and M. Eric Gershwin, "Primary Biliary Cirrhosis", New Engl. J. of Medicine, 353:1261-1273 September 22, 2005 Number 12 . Review article
- Carlo Selmi, Ross L. Coppel, and M. Eric Gershwin, "Primary Biliary Cirrhosis", in Noel R. Rose, Ian R. Mackey, eds, The Autoimmune Diseases, 4th edition, Academic Press, 2006
General
- Sanjiv Chopra. The Liver Book: A Comprehensive Guide to Diagnosis, Treatment, and Recovery, Atria, 2002, ISBN 0-7434-0585-4
- Melissa Palmer. Dr. Melissa Palmer's Guide to Hepatitis and Liver Disease: What You Need to Know, Avery Publishing Group; Revised edition May 24, 2004, ISBN 1-58333-188-3. her webpage.
- Howard J. Worman. The Liver Disorders Sourcebook, McGraw-Hill, 1999, ISBN 0-7373-0090-6.
See also
External Links
- PBCers.org - patients' organisation
- PBC Foundation UK