Pleomorphic adenoma
Template:DiseaseDisorder infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-In-Chief: Cafer Zorkun M.D., PhD.
Overview
Clinical Presentation
The tumour is usually solitary and presents as a slow growing, painless, firm single nodular mass. Isolated nodules are generally outgrowths of the main nodule rather than a multinodular presentation. It is usually mobile unless found in the palate and can cause atrophy of the mandibular ramus when located in the parotid gland. When found in the parotid tail, it may present as an eversion of the ear lobe. Though it is a benign tumour, pleomorphic adenomas have the capacity to grow to large proportions.
Diagnosis
The diagnosis of salivary gland tumors utilize both histopathological sampling and radiographic studies. Histopathological sampling procedures include fine needle aspiration (FNA) and core needle biopsy (bigger needle comparing to FNA). Both of these procedures can be done in an outpatient setting. Diagnostic imaging techniques for salivary gland tumors include ultrasound, computer tomography (CT) and magnetic resonance imaging (MRI). Fine needle aspiration biopsy (FNA), operated in experienced hands, can determine whether the tumor is malignant in nature with sensitivity around 90%[1][2]. FNA can also distinguish primary salivary tumor from metastatic disease. Core needle biopsy can also be done in outpatient setting. It is more invasive but is more accurate compared to FNA with diagnostic accuracy greater than 97%[3]. Furthermore, core needle biopsy allows more accurate histological typing of the tumor. In terms of imaging studies, ultrasound can determine and characterize superficial parotid tumors. Certain types of salivary gland tumors have certain sonographic characteristics on ultrasound[4]. Ultrasound is also frequently used to guide FNA or core needle biopsy. CT allows direct, bilateral visualization of the salivary gland tumor and provides information about overall dimension and tissue invasion. CT is excellent for demonstrating bony invasion. MRI provides superior soft tissue delineation such as perineural invasion when compared to CT only[5].
Diagnostic Findings
- At US, pleomorphic adenomas are hypoechoic, well-defined, lobulated tumors with posterior acoustic enhancement and may contain calcifications.
- On CT, pleomorphic adenomas are typically smooth, well-marginated tumors. The attenuation values of the mass are usually homogeneous and higher than that of the surrounding gland. Tumor enhancement is variable and can result in a missed diagnosis if delayed images are not acquired (Pleomorphic adenomas are poorly enhancing in the early phase of contrast enhancement, though the amount of enhancement increases over time).
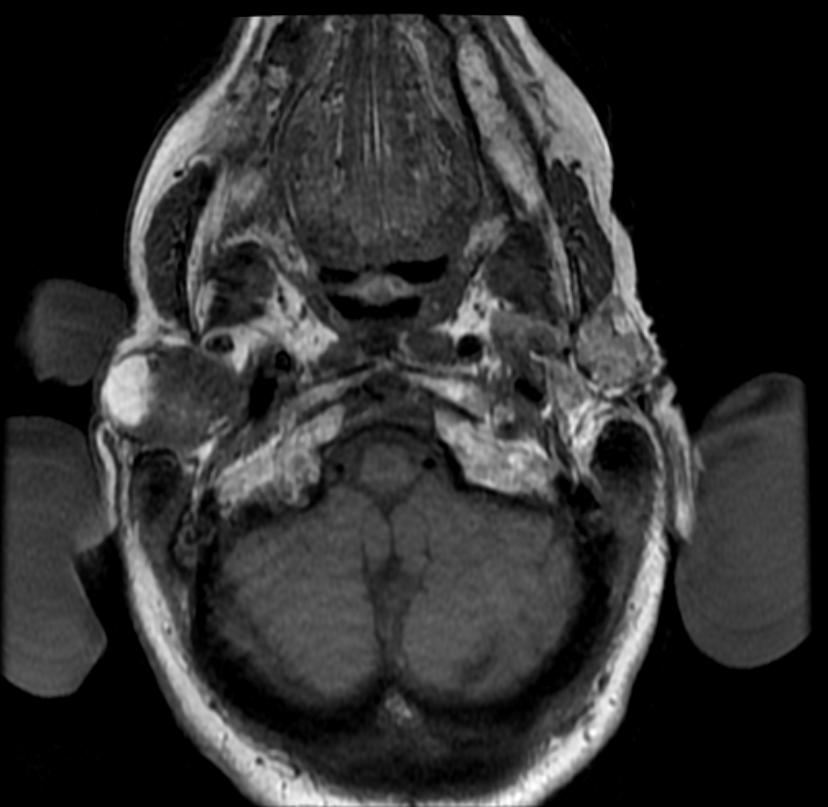
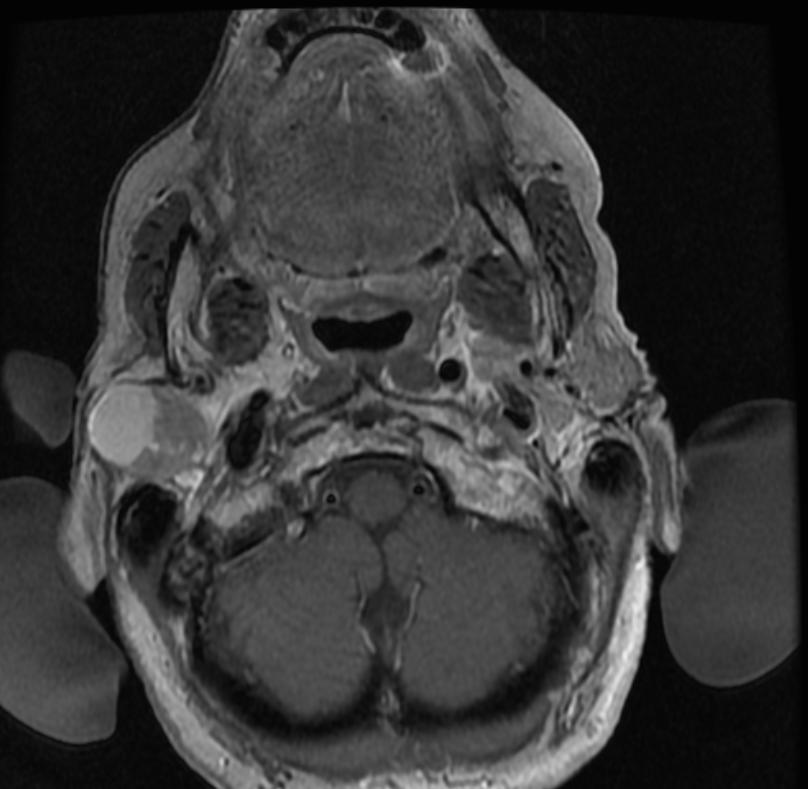
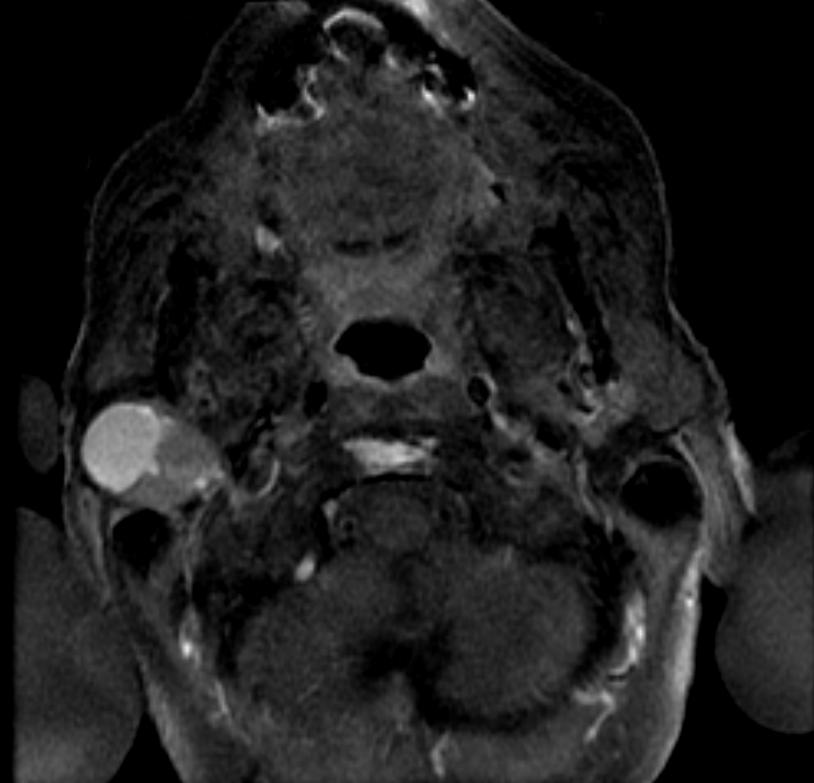
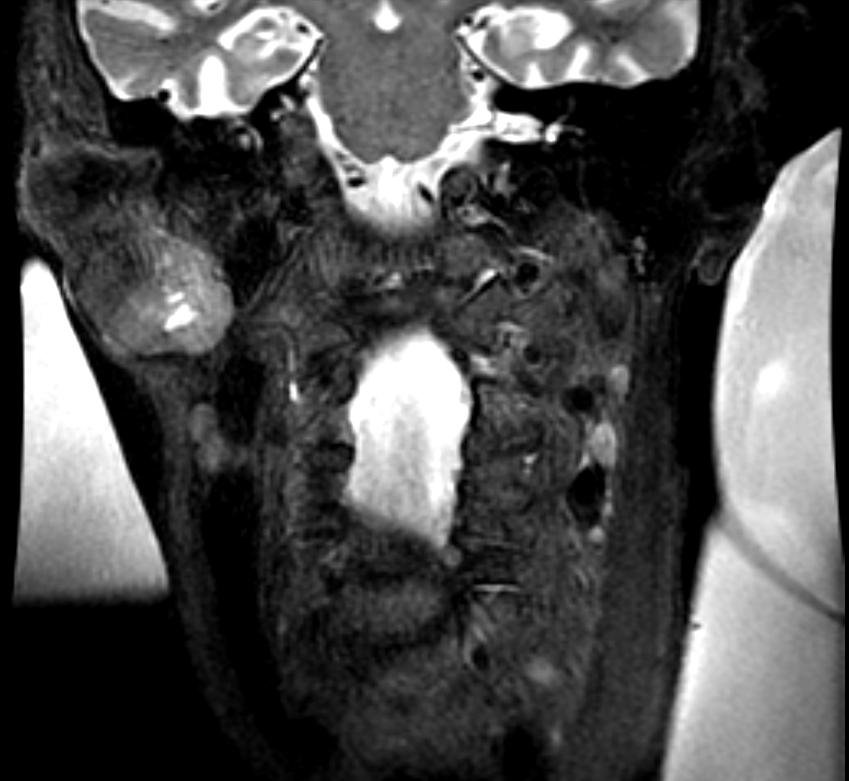
- On MRI, pleomorphic adenomas are usually well-circumscribed, homogeneous masses with low intensity on T1-weighted images and high intensity on T2-weighted images. They commonly have a rim of decreased signal intensity on T2-weighted images. After gadolinium enhancement, the tumors are homogeneously enhancing unless they are large (unlike CT, MRI has no role in delayed imaging).
-
MRI: A right parotid pleomorphic adenoma
-
MRI: A right parotid pleomorphic adenoma
-
MRI: A right parotid pleomorphic adenoma
-
MRI: A right parotid pleomorphic adenoma
-
MRI: A right parotid pleomorphic adenoma
-
PET: A right parotid pleomorphic adenoma
Histology
Histologically, it is highly variable in appearance, even within individual tumours. It is characterized by an admixture of epithelial and myoepithelial elements in a variable background stroma that may be mucoid, myxoid, cartilaginous or hyaline. Epithelial elements may be arranged in duct-like structures, sheets, clumps and/or interlacing strands and consist of polygonal, spindle or stellate-shaped cells (hence pleomorphism). Areas of squamous metaplasia and epithelial pearls may be present. The tumour is usually enveloped by a fibrous capsule of varying thickness and often incomplete. The tumour often extends through these discontinuities but is not a sign of malignant transformation as it does not invade surrounding tissues.
Treatment
Overall, the mainstay of the treatment for salivary gland tumor is surgical resection. Needle biopsy is highly recommended prior to surgery to confirm the diagnosis. More detailed surgical technique and the support for additional adjuvant radiotherapy depends on whether the tumor is malignant or benign. Generally, benign tumors of the parotid gland are treated with superficial or total parotidectomy with the latter being the more commonly practiced due to high incidence of recurrence[6]. The facial nerve should be preserved whenever possible. The benign tumors of the submandibular gland is treated by simple excision with preservation of mandibular branch of the trigeminal nerve, the hypoglossal nerve, and the lingual nerve[7]. Similarly, other benign tumors of minor salivary glands are treated similarly. Malignant salivary tumors usually require wide local resection of the primary tumor. However, if complete resection cannot be achieved, adjuvant radiotherapy should be added to improve local control[8][9]. This surgical treatment has many sequellae such as cranial nerve damage, Frey's syndrome , cosmetic problems, etc.
References
- ↑ Cohen EG, Patel SG, Lin O; et al. (2004). "Fine-needle aspiration biopsy of salivary gland lesions in a selected patient population". Arch Otolaryngol Head Neck Surg. 130 (6): 773–8. doi:10.1001/archotol.130.6.773. PMID 15210562. Unknown parameter
|month=ignored (help) - ↑ Batsakis JG, Sneige N, el-Naggar AK (1992). "Fine-needle aspiration of salivary glands: its utility and tissue effects". Ann Otol Rhinol Laryngol. 101 (2 Pt 1): 185–8. PMID 1739267. Unknown parameter
|month=ignored (help) - ↑ Wan YL, Chan SC, Chen YL; et al. (2004). "Ultrasonography-guided core-needle biopsy of parotid gland masses". AJNR Am J Neuroradiol. 25 (9): 1608–12. PMID 15502149. Unknown parameter
|month=ignored (help) - ↑ Białek EJ, Jakubowski W, Karpińska G (2003). "Role of ultrasonography in diagnosis and differentiation of pleomorphic adenomas: work in progress". Arch Otolaryngol Head Neck Surg. 129 (9): 929–33. doi:10.1001/archotol.129.9.929. PMID 12975263. Unknown parameter
|month=ignored (help) - ↑ Koyuncu M, Seşen T, Akan H; et al. (2003). "Comparison of computed tomography and magnetic resonance imaging in the diagnosis of parotid tumors". Otolaryngol Head Neck Surg. 129 (6): 726–32. doi:10.1016/j.otohns.2003.07.009. PMID 14663442. Unknown parameter
|month=ignored (help) - ↑ Stennert E, Guntinas-Lichius O, Klussmann JP, Arnold G (2001). "Histopathology of pleomorphic adenoma in the parotid gland: a prospective unselected series of 100 cases". Laryngoscope. 111 (12): 2195–200. doi:10.1097/00005537-200112000-00024. PMID 11802025. Unknown parameter
|month=ignored (help) - ↑ Leonetti JP, Marzo SJ, Petruzzelli GJ, Herr B (2005). "Recurrent pleomorphic adenoma of the parotid gland". Otolaryngol Head Neck Surg. 133 (3): 319–22. doi:10.1016/j.otohns.2005.04.008. PMID 16143173. Unknown parameter
|month=ignored (help) - ↑ Ganly I, Patel SG, Coleman M, Ghossein R, Carlson D, Shah JP (2006). "Malignant minor salivary gland tumors of the larynx". Arch Otolaryngol Head Neck Surg. 132 (7): 767–70. doi:10.1001/archotol.132.7.767. PMID 16847187. Unknown parameter
|month=ignored (help) - ↑ Terhaard CH, Lubsen H, Rasch CR; et al. (2005). "The role of radiotherapy in the treatment of malignant salivary gland tumors". Int J Radiat Oncol Biol Phys. 61 (1): 103–11. doi:10.1016/j.ijrobp.2004.03.018. PMID 15629600. Unknown parameter
|month=ignored (help)
See also
- Warthin's tumor - monomorphic adenoma
External links