|
|
| (40 intermediate revisions by 7 users not shown) |
| Line 1: |
Line 1: |
| {{Infobox_Disease | | | __NOTOC__ |
| Name = Pheochromocytoma |
| | {{Infobox_Disease |
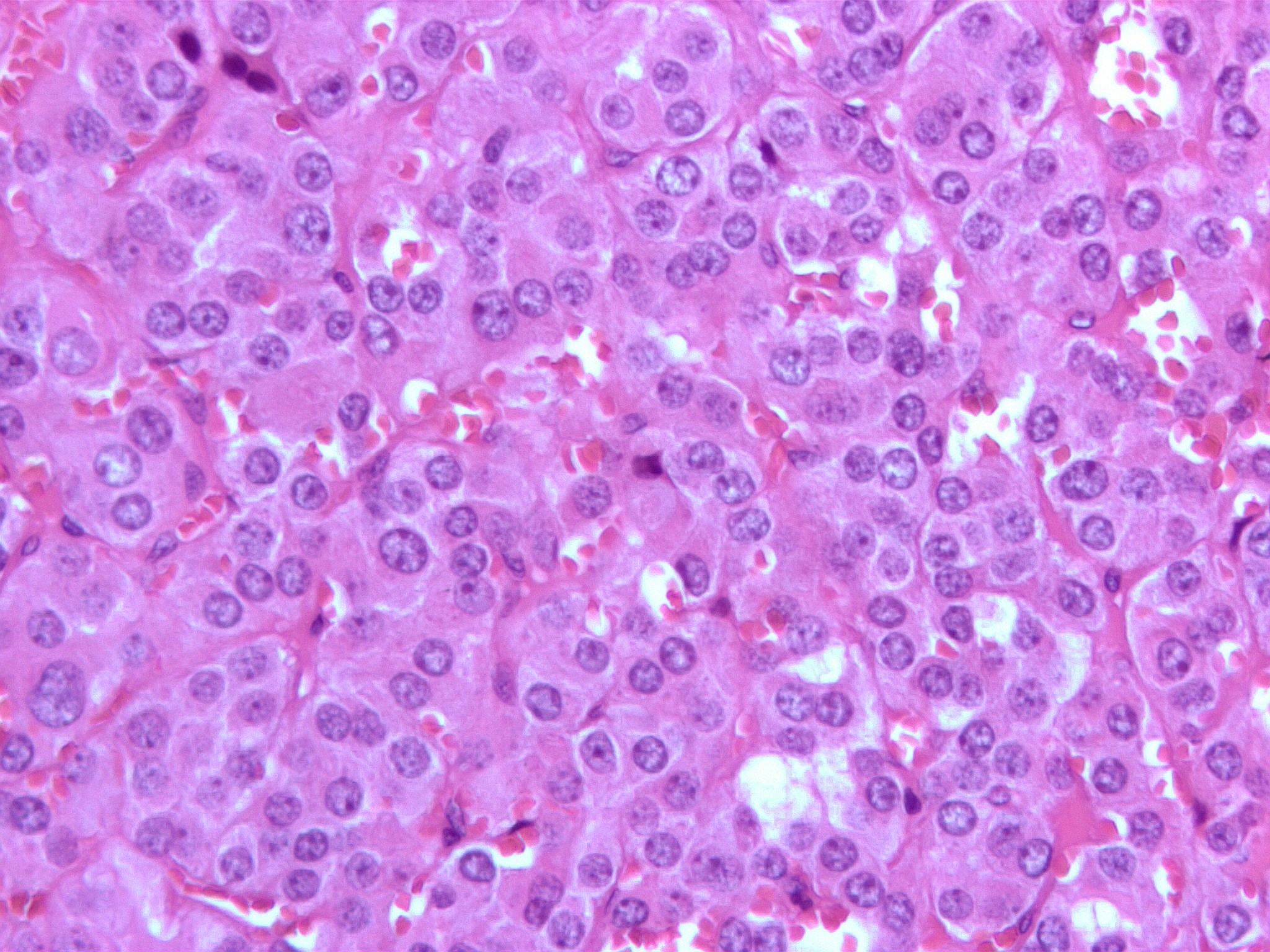
| Image = Pheochromocytoma high mag.jpg |
| | | Name = {{PAGENAME}} |
| Caption = Micrograph of a pheochromocytoma. |
| | | Image = Head.jpg |
| DiseasesDB = 9912 |
| | | Caption = Gross pathology of pheochromocytoma, source: wikipedia.org |
| ICD10 = {{ICD10|C|74|1|c|73}} |
| |
| ICD9 = {{ICD9|255.6}} |
| |
| ICDO = {{ICDO|8700|0}} |
| |
| OMIM = 171300 |
| |
| MedlinePlus = 000340|
| |
| eMedicineSubj = med |
| |
| eMedicineTopic = 1816 |
| |
| eMedicine_mult = {{eMedicine2|radio|552}} {{eMedicine2|ped|1788}} |
| |
| MeshID = D010673 |
| |
| }} | | }} |
| {{SI}} | | {{Pheochromocytoma}} |
| {{CMG}} | | {{CMG}}; {{AE}} {{AAM}} {{MAD}} |
|
| |
|
| {{editor help}} | | {{SK}} Phaeochromocytoma; Pheochromocytoma; Chromaffin paraganglioma; Chromaffin tumor; Chromaffinoma |
|
| |
|
| ==Overview==
| | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
|
| A '''pheochromocytoma''' ('''phaeochromocytoma''' outside of the US) is a [[neuroendocrine tumor]] of the [[Adrenal medulla|medulla]] of the [[adrenal gland]]s (originating in the [[chromaffin cell]]s) or extra-adrenal chromaffin tissue which failed to involute after birth,<ref>{{cite book |author=Boulpaep, Emile L.; Boron, Walter F. |title=Medical physiology: a cellular and molecular approach |publisher=Saunders |location=Philadelphia |year=2003 |pages=1065 |isbn=0-7216-3256-4 |oclc= |doi=}}</ref> which secretes excessive amounts of [[catecholamine]]s, usually [[epinephrine]] and [[norepinephrine]].
| |
| Extra-adrenal [[paragangliomas]] (often described as extra-adrenal pheochromocytomas) are closely related, though less common, tumors that originate in the [[ganglion|ganglia]] of the [[sympathetic nervous system]] and are named based upon the primary anatomical site of origin.
| |
|
| |
|
| Traditionally it is known as the "10% tumor":
| | {{Infobox_Disease | |
| * bilateral disease is present in approximately 10% of patients
| | Name = Pheochromocytoma | |
| * approximately 10% of tumours are malignant
| | Image = Pheochromocytoma high mag.jpg | |
| * approximately 10% are located in chromaffin tissue outside of the adrenal gland
| | Caption = Micrograph of a pheochromocytoma | |
| * Approximately 10% arise in childhood
| | }} |
| * Approximately 10% are familial
| |
| * Approximately 10% recur after being resected
| |
| * Approximately 10% patients do not have [[hypertension]] (Campbell's Urology)
| |
| | |
| ===Differential diagnosis===
| |
| | |
| The [[differential diagnosis]] of pheochromocytoma includes:
| |
| *[[Anxiety disorder]]s
| |
| *[[Carcinoid tumor]]
| |
| *[[Paraganglioma]]s
| |
| *[[Essential hypertension]]
| |
| *[[Hyperthyroidism]]
| |
| *[[Insulinoma]]
| |
| *[[Paroxysmal supraventricular tachycardia]]
| |
| *[[Renovascular hypertension]]
| |
| | |
| ==Inheritance and Genetic Syndromes==
| |
| | |
| Up to 25% of pheochromocytomas may be [[familial]]. Mutations of the genes ''[[VHL]]'', ''RET'', ''NF1'', ''[[SDHB]]'' and ''[[SDHD]]'' are all known to cause familial pheochromocytoma/extra-adrenal paraganglioma.
| |
|
| |
|
| Pheochromocytoma is a [[tumor]] of the [[multiple endocrine neoplasia]] syndrome, type IIA (also known as MEN IIA) and type IIB MEN IIB. The other component [[neoplasms]] of that syndrome include [[parathyroid]] [[adenomas]], and [[medullary thyroid cancer]]. [[Mutations]] in the [[autosomal]] RET [[proto-oncogene]] drives these malignancies
| | ==[[Pheochromocytoma overview|Overview]]== |
| <ref>{{OMIM|171400|MULTIPLE ENDOCRINE NEOPLASIA, TYPE IIA; MEN2A}}</ref>.
| |
|
| |
|
| Common [[mutations]] in the RET oncogene may also account for [[medullary sponge kidney]] as well. <ref name="pmid11096158">{{cite journal |author=Diouf B, Ka EH, Calender A, Giraud S, Diop TM |title=Association of medullary sponge kidney disease and multiple endocrine neoplasia type IIA due to RET gene mutation: is there a causal relationship? |journal=Nephrol. Dial. Transplant. |volume=15 |issue=12 |pages=2062–3 |year=2000 |pmid=11096158|doi=10.1093/ndt/15.12.2062}}</ref>
| | ==[[Pheochromocytoma historical perspective|Historical Perspective]]== |
|
| |
|
| Pheochromocytoma linked to MEN II can be caused by RET oncogene mutations. Both syndromes are characterized by pheochromocytoma as well as [[thyroid cancer]] (thyroid medullary carcinoma). MEN IIA also presents with hyperparathyroidism, while MEN IIB also presents with mucosal neuroma. It is now postulated that Lincoln suffered from MEN IIB, rather than [[Marfan's syndrome]] as previously thought, though this is uncertain.
| | ==[[Pheochromocytoma classification|Classification]]== |
|
| |
|
| ==Features== | | ==[[Pheochromocytoma pathophysiology|Pathophysiology]]== |
|
| |
|
| The [[signs]] and [[symptoms]] of a pheochromocytoma are those of [[sympathetic nervous system]] [[hyperactivity]], including:
| | ==[[Pheochromocytoma causes|Causes]]== |
|
| |
|
| *[[Elevated heart rate]]
| | ==[[Pheochromocytoma differential diagnosis|Differentiating Pheochromocytoma from other Diseases]]== |
| *[[Elevated blood pressure]], including paroxysmal (sporadic, episodic) high blood pressure, which sometimes can be more difficult to detect; another clue to the presence of pheochromocytoma is [[orthostatic hypotension]] (a fall in [[systolic blood pressure]] greater than 20 [[mmHg]] or a fall in [[diastolic blood pressure]] greater than 10 [[mmHg]] on making the patient stand)
| |
| *[[Palpitations]]
| |
| *[[Anxiety]] often resembling that of a [[panic attack]]
| |
| *[[Diaphoresis]]
| |
| *[[Headaches]]
| |
| *[[Pallor]]
| |
| *[[Weight loss]]
| |
| *Localized [[amyloid]] deposits found microscopically
| |
| *Elevated blood glucose level (due primarily to catecholamine stimulation of [[lipolysis]] (breakdown of stored fat) leading to high levels of [[free fatty acids]] and the subsequent inhibition of glucose uptake by muscle cells. Further, stimulation of beta-adrenergic receptors leads to glycogenolysis and gluconeogenesis and thus elevation of blood glucose levels).
| |
|
| |
|
| A pheochromocytoma can also cause resistant [[arterial hypertension]]. A pheochromocytoma can be fatal if it causes [[malignant hypertension]], or severely [[high blood pressure]]. This hypertension is not well controlled with standard blood pressure medications.
| | ==[[Pheochromocytoma epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| Not all patients experience all of the signs and symptoms listed. The most common presentation is headache, excessive sweating, and increased heart rate, with the attack subsiding in less than one hour.
| | ==[[Pheochromocytoma risk factors|Risk Factors]]== |
|
| |
|
| Tumors may grow very large, but most are smaller than 10 cm.
| | ==[[Pheochromocytoma screening|Screening]]== |
|
| |
|
| ==Tumor Location== | | ==[[Pheochromocytoma natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| In adults, 90% tumors are located unilaterally and are solitary, and 10% are located outside the adrenal gland. In children 50% are adrenal, while 25% are bilateral and 25% are extraadrenal. The common extradrenal locations are the abdomen, thorax and urinary bladder.
| |
|
| |
|
| ==Diagnosis== | | ==Diagnosis== |
| [[Image:Adrenal pheochromocytoma (3) histopathology.jpg|thumb|left|150px|Histopathology of adrenal pheochromocytoma. Adrenectomy specimen. ]] | | [[Pheochromocytoma history and symptoms|History and Symptoms]] | [[Pheochromocytoma physical examination|Physical Examination]] | [[Pheochromocytoma laboratory findings|Laboratory Findings]] | [[Pheochromocytoma electrocardiogram|Electrocardiogram]] | [[Pheochromocytoma x ray|X Ray]] | [[Pheochromocytoma CT|CT]] | [[Pheochromocytoma MRI|MRI]] | [[Pheochromocytoma echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Pheochromocytoma other imaging findings|Other Imaging Findings]] | [[Pheochromocytoma other diagnostic studies|Other Diagnostic Studies]] |
| [[Image:Adrenaline.svg|thumb|150px|left|[[Epinephrine]]]] | |
| [[Image:Norepinephrine.png|thumb|100px|left|[[Norepinephrine]]]] | |
| The diagnosis can be established by measuring [[catecholamine]]s and [[metanephrine]]s in plasma or through a 24-hour urine collection. Care should be taken to rule out other causes of adrenergic (adrenalin-like) excess like hypoglycemia, stress, exercise, and drugs affecting the catecholamines like [[stimulant]]s, [[methyldopa]], [[dopamine]] [[agonist]]s, or ganglion blocking [[antihypertensive]]s. Various foodstuffs (e.g. vanilla ice cream) can also affect the levels of urinary [[metanephrine]] and VMA ([[vanillyl mandelic acid]]). Imaging by [[computed tomography]] or a [[Spin-spin relaxation time|T2]] weighted [[magnetic resonance imaging|MRI]] of the [[head]], [[neck]], and [[chest]], and [[abdomen]] can help localize the tumor. Tumors can also be located using [[Iodine-131]] meta-iodobenzylguanidine (I131 MIBG) imaging.
| |
| | |
| One diagnostic test used in the past for a pheochromocytoma is to administer [[clonidine]], a centrally-acting alpha-2 agonist used to treat high blood pressure. Clonidine mimics catecholamines in the brain, causing it to reduce the activity of the sympathetic nerves controlling the adrenal medulla. A healthy adrenal medulla will respond to the [[Clonidine#Clonidine suppression test|Clonidine suppression test]] by reducing catecholamine production; the lack of a response is evidence of pheochromocytoma.
| |
| | |
| Another test is for the clinician to press gently on the [[adrenal gland]]. A pheochromocytoma will often release a burst of catecholamines, with the associated signs and symptoms quickly following. This method is not recommended because of possible complications arising from a potentially massive release of catecholamines.
| |
| | |
| Pheochromocytomas occur most often during young-adult to mid-adult life. Less than 10% of pheochromocytomas are [[malignant]] (cancerous), bilateral or pediatric.
| |
| | |
| These tumors can form a pattern with other endocrine gland cancers which is labeled [[multiple endocrine neoplasia]] (MEN). Pheochromocytoma may occur in patients with MEN 2 and MEN 3. [[VHL]] (Von Hippel Lindau) patients may also develop these tumors.
| |
| | |
| Patients experiencing symptoms associated with pheochromocytoma should be aware that it is rare. However, it often goes undiagnosed until autopsy; therefore patients might wisely choose to take steps to provide a physician with important clues, such as recording whether blood pressure changes significantly during episodes of apparent anxiety.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Surgical [[resection]] of the tumor is the treatment of first choice. Given the complexity of [[perioperative]] management, and the potential for catastrophic intra and postoperative complications, such surgery should be performed only at centers experienced in the area. In addition to the surgical expertise that such centers can provide, they will also have the necessary endocrine and anesthesia resources as well. It may also be nescessary to carry out adrenalectomy, a complete surgical removal of the affected adrenal gland(s).
| | [[Pheochromocytoma medical therapy|Medical Therapy]] | [[Pheochromocytoma surgery|Surgery]] | [[Pheochromocytoma primary prevention|Primary Prevention]] | [[Pheochromocytoma secondary prevention|Secondary Prevention]] | [[Pheochromocytoma cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Pheochromocytoma future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| Either surgical option requires prior treatment with both the non-specific alpha adrenoceptor blocker [[Phenoxybenzamine]] to counteract hypertension and the beta-1 adrenoceptor antagonist [[Atenolol]] to reduce cardiac output. Given before surgery, these can also block the effect of a sudden release of adrenaline during tumour removal, which would otherwise endanger the anaethetised patient.
| | ==Case Studies== |
| | | [[Pheochromocytoma case study one|Case #1]] |
| ==Historical== | |
| In 1886, Fränkel made the first description of a patient with pheochromocytoma, however the term was first coined by Pick, a pathologist, in 1912. In 1926, Roux (in Switzerland) and Mayo (in U.S.A.) were the first surgeons to remove pheochromocytomas.<br />
| |
| Jaroszewski DE, Tessier DJ, Schlinkert RT, et al. Laparoscopic adrenalectomy for pheochromocytoma. Mayo Clin Proc. 2003; 78: 1501-1504.
| |
| | |
| ==Additional images==
| |
| | |
| <gallery>
| |
| Image:Adrenal pheochromocytoma (1) histopathology.jpg|[[Micrograph]] of pheochromocytoma.
| |
| Image:Adrenal pheochromocytoma (2) histopathology.jpg|Micrograph of pheochromocytoma.
| |
| Image:Adrenal pheochromocytoma (3) histopathology.jpg|Micrograph of pheochromocytoma.
| |
| Image:Bilateral pheo MEN2.jpg|Bilateral pheochromocytoma in [[Multiple_endocrine_neoplasia_type_2|MEN2]]. Gross image.
| |
| Image:Pheochromocytoma.jpg|Pheochromocytoma. CT abdomen.
| |
| Image:Pheochromocytoma2.jpg|Pheochromocytoma. CT abdomen.
| |
| </gallery>
| |
|
| |
|
| ==References== | | ==References== |
| {{Reflist|2}} | | {{reflist|2}} |
|
| |
|
| ==External links==
| |
| * [http://clinicaltrials.gov/show/NCT00458952 Pheochromocytoma clinical trial currently recruiting patients]
| |
| * {{MedlinePlusOverview|pheochromocytoma}}
| |
| * [http://www.cancer.gov/cancertopics/pdq/treatment/pheochromocytoma/healthprofessional overview] from [[National Cancer Institute]]
| |
| * [http://www.pressor.org/members.html Pheochromocytoma Research Support Organization at pressor.org]
| |
| * [http://pub1.ezboard.com/bpheochromocytomasupportboard Pheochromocytoma Support Worldwide at pub1.ezboard.com]
| |
| * [http://www.pheochromocytoma.org/sys-tmpl/door/ pheochromocytoma.org]
| |
| {{Epithelial neoplasms}}
| |
| {{SIB}}
| |
| [[Category:Endocrinology]] | | [[Category:Endocrinology]] |
| [[Category:Oncology]]
| |
| [[de:Phäochromozytom]]
| |
| [[es:Feocromocitoma]]
| |
| [[fr:Phéochromocytome]]
| |
| [[it:Feocromocitoma]]
| |
| [[he:פאוכרומוציטומה]]
| |
| [[nl:Feochromocytoom]]
| |
| [[ja:褐色細胞腫]]
| |
| [[pl:Guz chromochłonny nadnerczy]]
| |
| [[sv:Feokromocytom]]
| |
|
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WS}} |
| {{WikiDoc Sources}} | | {{WH}} |