Peutz-Jeghers syndrome: Difference between revisions
No edit summary |
|||
| Line 13: | Line 13: | ||
MeshID = D010580 | | MeshID = D010580 | | ||
}} | }} | ||
{{ | {{Peutz-Jeghers syndrome}} | ||
'''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' | ||
Revision as of 23:57, 20 January 2012
| Peutz-Jeghers syndrome | |
 | |
|---|---|
| ICD-10 | Q85.8 |
| ICD-9 | 759.6 |
| OMIM | 175200 |
| DiseasesDB | 9905 |
| MeSH | D010580 |
|
Peutz-Jeghers syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Peutz-Jeghers syndrome On the Web |
|
American Roentgen Ray Society Images of Peutz-Jeghers syndrome |
|
Risk calculators and risk factors for Peutz-Jeghers syndrome |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Diagnosis
Causes of Peutz-Jeghers syndrome
History & Symptoms
Natural history, Complications, and Prognosis
Screening
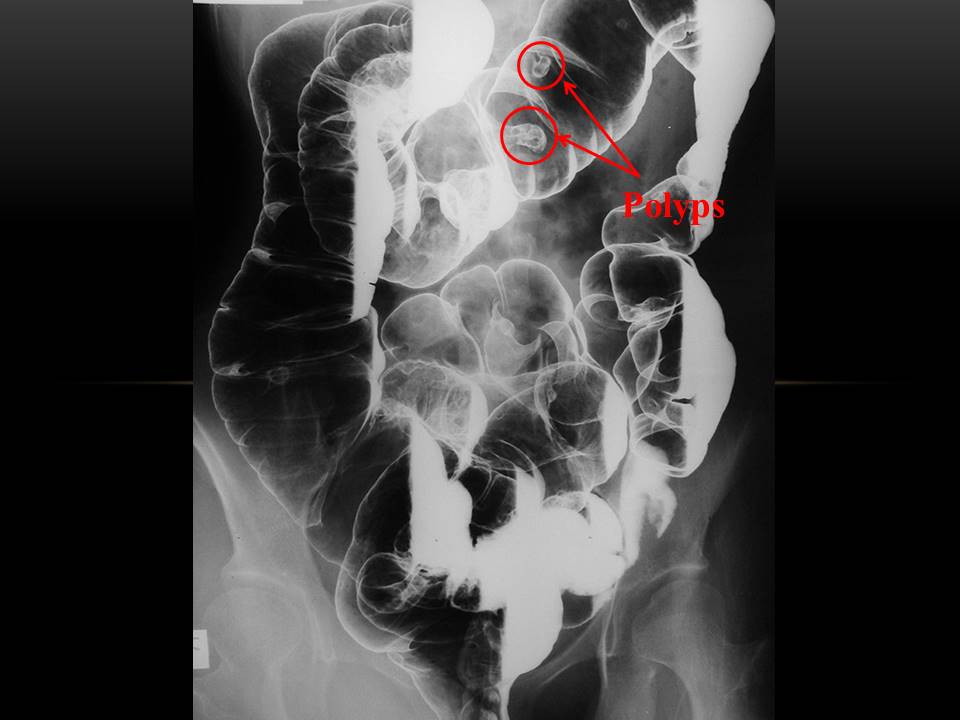
Screening includes upper GI endoscopy, enteroclysis, and colonoscopy to check for the locations of the hamartomas. To check for cancerous lesions, endoscopic ultrasound, testicular ultrasound and imaging studies of the liver and the pancreas are indicated because of the risk of pancreatic cancer as well as gallbladder polyps and cancer. These imaging studies may include ultrasonography as well as CT with pancreatic details or magnetic resonance cholangiopancreatography (MRCP).
In addition, an annual physical examination that includes evaluation of the breasts, abdomen, pelvis, and testes should be done by a physician. An annual complete blood count to check for anemia should be done. If bleeding is found, removal of hemorrhagic or large polyps (>5 mm) by endoscopic polypectomy should be performed.
Some suggestions for surveillance for cancer include the following: Small intestine with small bowel radiography every 2 years, Esophagogastroduodenoscopy and colonoscopy every 2 years, Ultrasound of the pancreas yearly, Ultrasound of the pelvis (women) and testes (men) yearly, Mammography (women) at ages 25, 30, 35, and 38 years, then every 2 years until age 50 years, then annually, and Papanicolaou (Pap) test every year
Follow-up care should be supervised by a gastroenterologist familiar with Peutz-Jeghers syndrome. Genetic consultation and counseling as well as urological and gynecological consultations are required in the management of these patients.
References
Template:Digestive system neoplasia
de:Peutz-Jeghers-Syndrom
it:Sindrome di Peutz-Jeghers
nl:Syndroom van Peutz-Jeghers