Parathyroid adenoma: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
'''For patient information, click [[Insert page name here (patient information)|Insert page name here]]''' | '''For patient information, click [[Insert page name here (patient information)|Insert page name here]]''' | ||
{{CMG}}; {{AE}} {{Ammu}} | |||
{{CMG}} | ==Overview== | ||
A parathyroid adenoma is a [[adenoma|benign tumor]] of the [[parathyroid gland]]. Parathyroid adenoma can be associated with overexpression of the [[cyclin D1]] gene. Hyperparathyroidism is confirmed by blood tests such as calcium and parathormone levels. A specific test for parathyroid adenoma is [[sestamibi parathyroid scintigraphy]], the sestamibi scan. [[Surgery]] is the only cure for parathyroid adenomas. | |||
{{ | |||
== Overview == | |||
== Pathophysiology== | == Pathophysiology== | ||
* A parathyroid adenoma is a [[adenoma|benign tumor]] of the [[parathyroid gland]]. It generally causes [[hyperparathyroidism]]; there are very few reports of parathyroid adenomas that were not associated with hyperparathyroidism.<ref name=sekine>{{cite journal |author=Sekine O, Hozumi Y, Takemoto N, Kiyozaki H, Yamada S, Konishi F |title=Parathyroid adenoma without hyperparathyroidism |journal=Japanese Journal of Clinical Oncology |volume=34 |issue=3 |pages=155–8 |date=March 2004 |pmid=15078912 |doi=10.1093/jjco/hyh028}}</ref> | * A parathyroid adenoma is a [[adenoma|benign tumor]] of the [[parathyroid gland]]. It generally causes [[hyperparathyroidism]]; there are very few reports of parathyroid adenomas that were not associated with hyperparathyroidism.<ref name=sekine>{{cite journal |author=Sekine O, Hozumi Y, Takemoto N, Kiyozaki H, Yamada S, Konishi F |title=Parathyroid adenoma without hyperparathyroidism |journal=Japanese Journal of Clinical Oncology |volume=34 |issue=3 |pages=155–8 |date=March 2004 |pmid=15078912 |doi=10.1093/jjco/hyh028}}</ref> | ||
* A human being usually has four parathyroid glands located on the back surface of the [[thyroid]] in the neck. The parathyroids secrete [[parathyroid hormone]] (PTH), which increases the concentration of [[calcium]] in the blood by inducing the [[bone]]s to release calcium into the blood and the [[kidney]]s to reabsorb it from the urine into the blood. When a parathyroid adenoma causes hyperparathyroidism, more parathyroid hormone is secreted, causing the calcium concentration of the blood to rise, resulting in [[Hypercalcaemia|hypercalcemia]].<ref name=fel>{{cite journal |author=Felsenfeld AJ, Rodríguez M, Aguilera-Tejero E |title=Dynamics of parathyroid hormone secretion in health and secondary hyperparathyroidism |journal=Clinical Journal of the American Society of Nephrology |volume=2 |issue=6 |pages=1283–305 |date=November 2007 |pmid=17942777 |doi=10.2215/CJN.01520407}}</ref> | * A human being usually has four parathyroid glands located on the back surface of the [[thyroid]] in the neck. The parathyroids secrete [[parathyroid hormone]] (PTH), which increases the concentration of [[calcium]] in the blood by inducing the [[bone]]s to release calcium into the blood and the [[kidney]]s to reabsorb it from the urine into the blood. When a parathyroid adenoma causes hyperparathyroidism, more parathyroid hormone is secreted, causing the calcium concentration of the blood to rise, resulting in [[Hypercalcaemia|hypercalcemia]].<ref name=fel>{{cite journal |author=Felsenfeld AJ, Rodríguez M, Aguilera-Tejero E |title=Dynamics of parathyroid hormone secretion in health and secondary hyperparathyroidism |journal=Clinical Journal of the American Society of Nephrology |volume=2 |issue=6 |pages=1283–305 |date=November 2007 |pmid=17942777 |doi=10.2215/CJN.01520407}}</ref> | ||
=== Genetics === | === Genetics === | ||
* Parathyroid adenoma can be associated with overexpression of the [[cyclin D1]] gene.<ref>{{cite journal |author=Hsi ED, Zukerberg LR, Yang WI, Arnold A |title=Cyclin D1/PRAD1 expression in parathyroid adenomas: an immunohistochemical study |journal=The Journal of Clinical Endocrinology and Metabolism |volume=81 |issue=5 |pages=1736–9 |date=May 1996 |pmid=8626826 |doi=10.1210/jcem.81.5.8626826}}</ref> | * Parathyroid adenoma can be associated with overexpression of the [[cyclin D1]] gene.<ref>{{cite journal |author=Hsi ED, Zukerberg LR, Yang WI, Arnold A |title=Cyclin D1/PRAD1 expression in parathyroid adenomas: an immunohistochemical study |journal=The Journal of Clinical Endocrinology and Metabolism |volume=81 |issue=5 |pages=1736–9 |date=May 1996 |pmid=8626826 |doi=10.1210/jcem.81.5.8626826}}</ref> | ||
| Line 29: | Line 23: | ||
:* An inherited syndrome<ref>Parathyroid adenoma. Canadian cancer society(2015). http://www.cancer.ca/en/cancer-information/cancer-type/parathyroid/parathyroid-cancer/benign-tumours/?region=on Accessed on December 29, 2015</ref> | :* An inherited syndrome<ref>Parathyroid adenoma. Canadian cancer society(2015). http://www.cancer.ca/en/cancer-information/cancer-type/parathyroid/parathyroid-cancer/benign-tumours/?region=on Accessed on December 29, 2015</ref> | ||
:* Multiple endocrine neoplasia type 1 (MEN 1) | :* Multiple endocrine neoplasia type 1 (MEN 1) | ||
:* Familial isolated hyperparathyroidism (FIHP) | :* Familial isolated hyperparathyroidism (FIHP) | ||
:* Hyperparathyroidism–jaw tumour (HPT-JT) syndrome | :* Hyperparathyroidism–jaw tumour (HPT-JT) syndrome | ||
| Line 36: | Line 28: | ||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
Hyperparathyroidism is confirmed by blood tests such as calcium and | Hyperparathyroidism is confirmed by blood tests such as calcium and parathormone levels<ref>Parathyroid adenoma. Wikipedia(2015). https://en.wikipedia.org/wiki/Parathyroid_adenoma Accessed on December 29, 2015</ref>. | ||
=== Symptoms === | === Symptoms === | ||
Revision as of 04:54, 30 December 2015
For patient information, click Insert page name here Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Overview
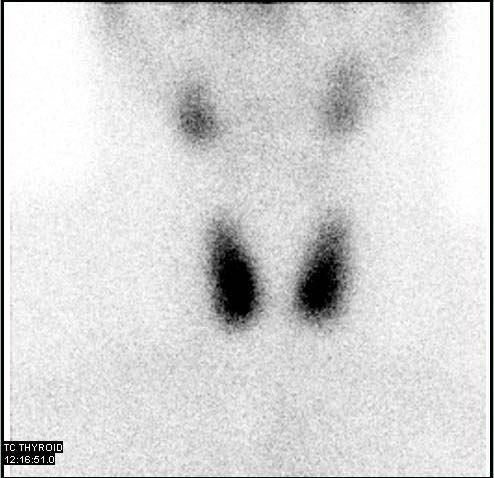
A parathyroid adenoma is a benign tumor of the parathyroid gland. Parathyroid adenoma can be associated with overexpression of the cyclin D1 gene. Hyperparathyroidism is confirmed by blood tests such as calcium and parathormone levels. A specific test for parathyroid adenoma is sestamibi parathyroid scintigraphy, the sestamibi scan. Surgery is the only cure for parathyroid adenomas.
Pathophysiology
- A parathyroid adenoma is a benign tumor of the parathyroid gland. It generally causes hyperparathyroidism; there are very few reports of parathyroid adenomas that were not associated with hyperparathyroidism.[1]
- A human being usually has four parathyroid glands located on the back surface of the thyroid in the neck. The parathyroids secrete parathyroid hormone (PTH), which increases the concentration of calcium in the blood by inducing the bones to release calcium into the blood and the kidneys to reabsorb it from the urine into the blood. When a parathyroid adenoma causes hyperparathyroidism, more parathyroid hormone is secreted, causing the calcium concentration of the blood to rise, resulting in hypercalcemia.[2]
Genetics
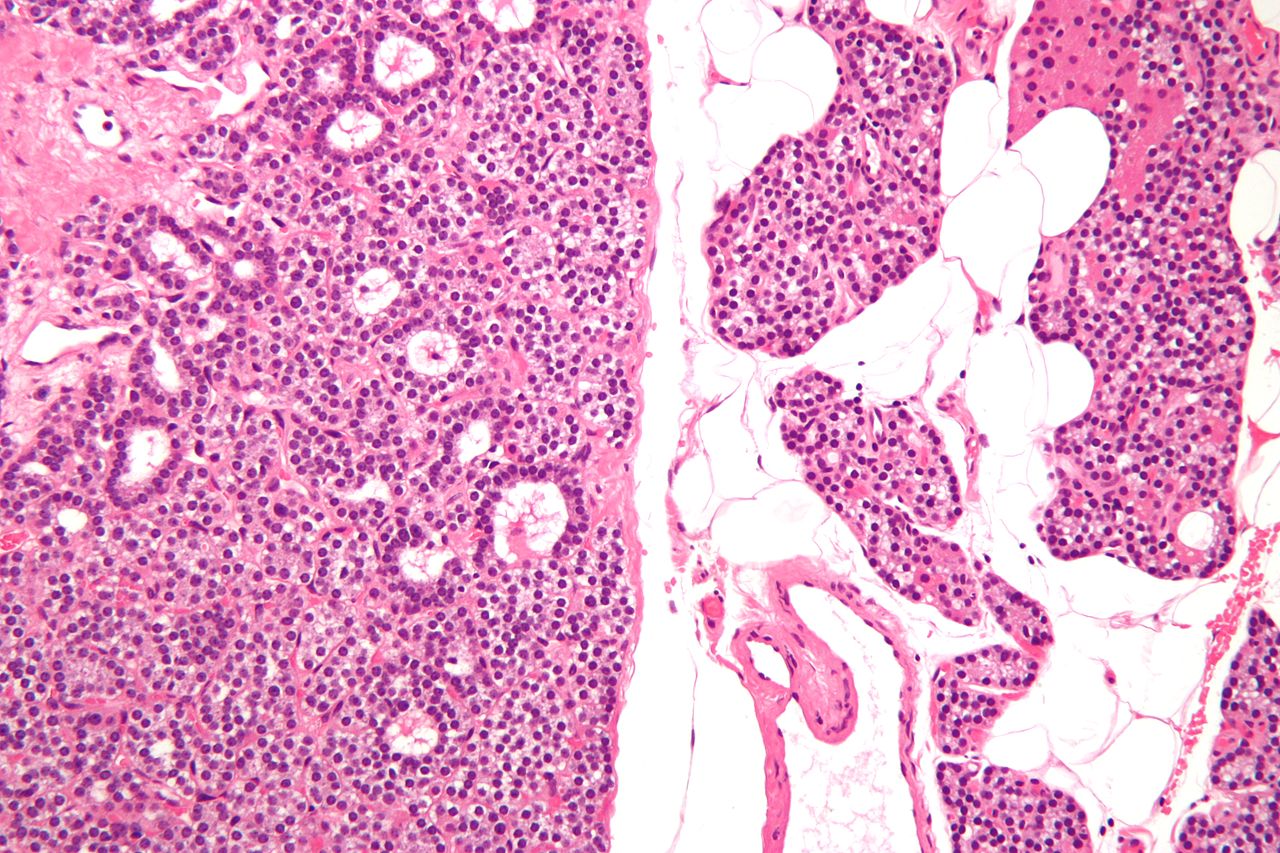
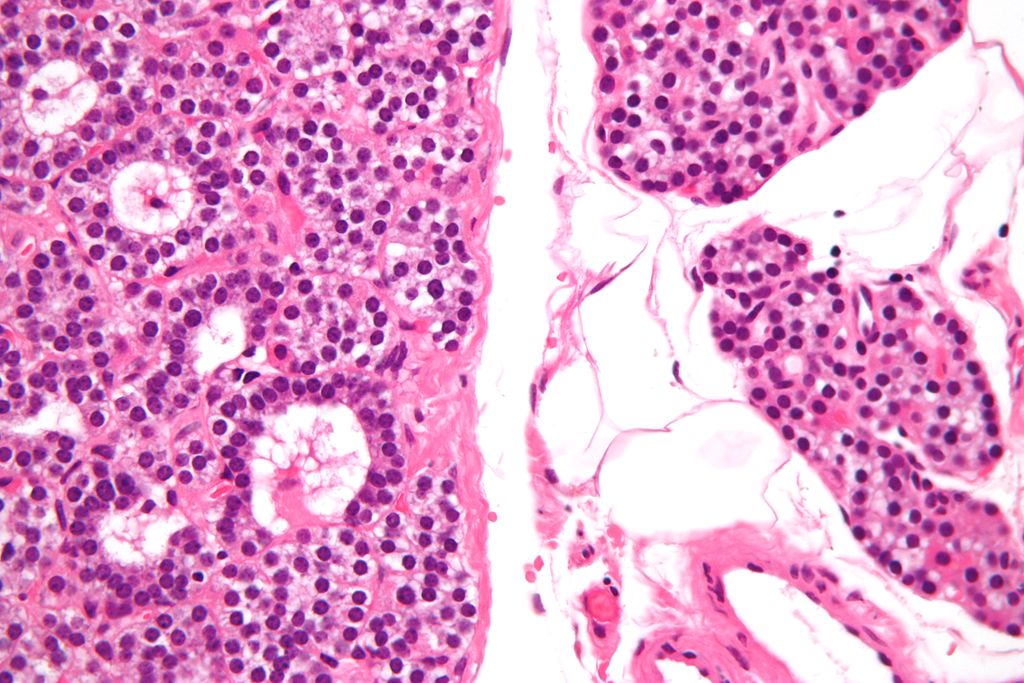
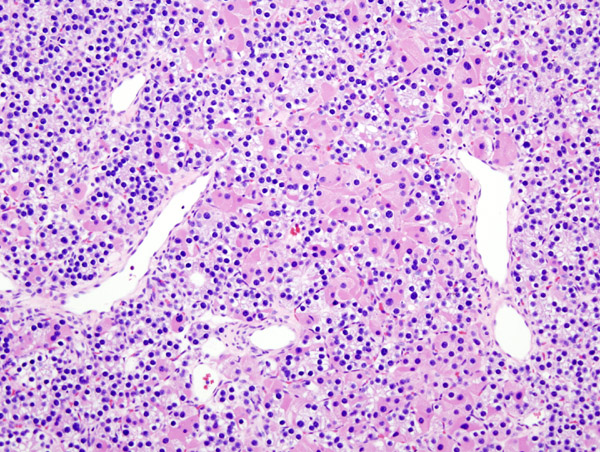
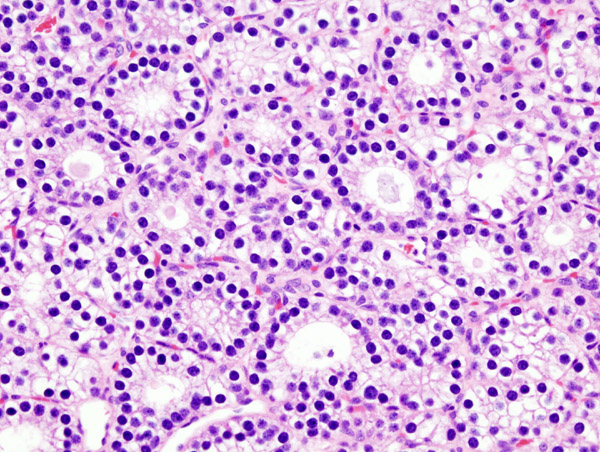
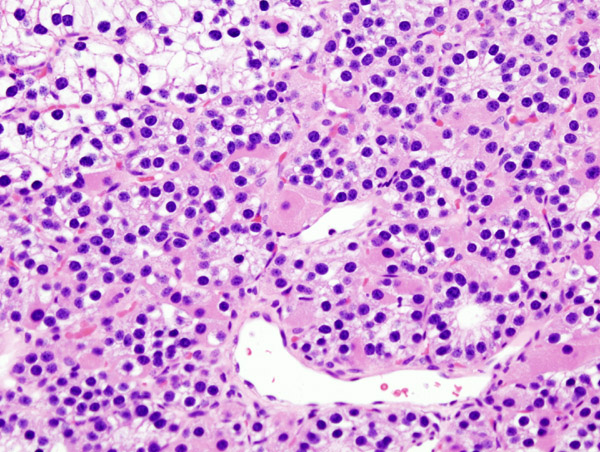
Micrographs of Parathyroid Adenoma
Risk Factors
- The following risk factors may increase a person’s chance of developing a parathyroid adenoma:
- An inherited syndrome[4]
- Multiple endocrine neoplasia type 1 (MEN 1)
- Familial isolated hyperparathyroidism (FIHP)
- Hyperparathyroidism–jaw tumour (HPT-JT) syndrome
- Radiation therapy to the head or neck
Diagnostic Criteria
Hyperparathyroidism is confirmed by blood tests such as calcium and parathormone levels[5].
Symptoms
- Fatigue
- Confusion
- Nausea
- Constipation
- Kidney stones
- Muscle aches
- Bone fracture
Other Imaging Findings
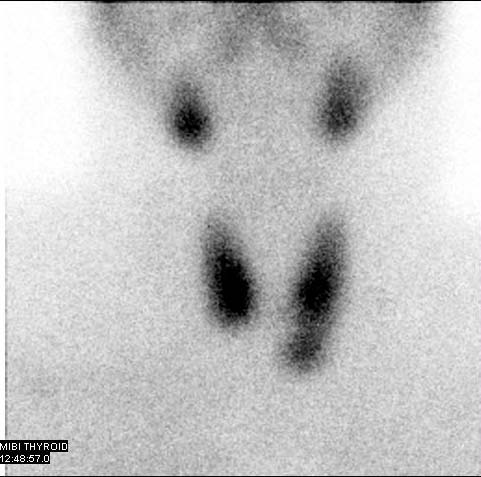
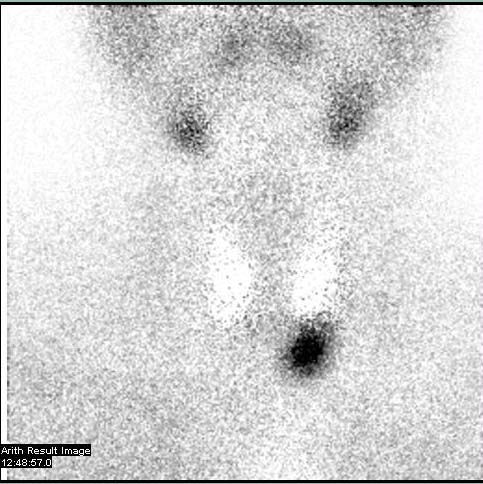
- A specific test for parathyroid adenoma is sestamibi parathyroid scintigraphy, the sestamibi scan. This nuclear imaging technique reveals the presence and location of pathological parathyroid tissue.[6]
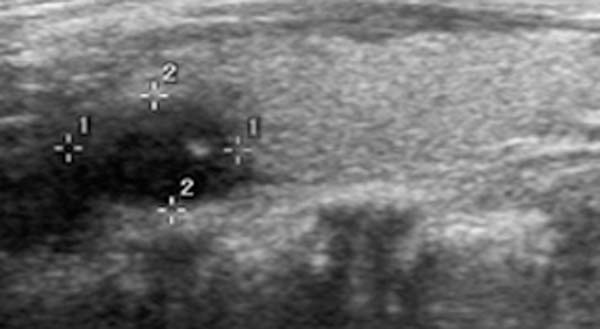
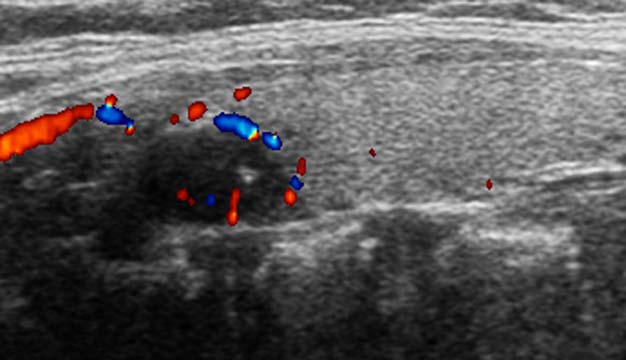
Imaging Findings
Patient #1
Patient #2
Other Diagnostic Studies
Treatment
Surgery
Surgery is the only cure for parathyroid adenomas.[7] It is successful about 95% of the time. Parathyroidectomy is the removal of the affected gland(s). The standard of treatment of primary hyperparathyroidism was formerly a surgical technique called bilateral neck exploration, in which the neck was opened on both sides, the parathyroids were identified, and the affected tissue was removed.[8] By the 1980s, unilateral exploration became more common.[8] Parathyroidectomy can now be performed in a minimally invasive fashion, mainly because imaging techniques can pinpoint the location of the tissue.[8] Minimally invasive techniques include smaller open procedures, radio-guided and video-assisted procedures, and totally endoscopic surgery.[8]
Before surgery is attempted, the affected glandular tissue must be located. Though the parathyroid glands are usually located on the back of the thyroid, their position is variable. Some people have one or more parathyroid glands elsewhere in the neck anatomy or in the chest. About 10% of parathyroid adenomas are ectopic, located not along the back of the thyroid but elsewhere in the body, sometimes in the mediastinum of the chest.[7] This can make them difficult to locate, so various imaging techniques are used, such as the sestamibi scan, single-photon emission computed tomography (SPECT), ultrasound, MRI,[7] and CT scans.[7][9]
References
- ↑ Sekine O, Hozumi Y, Takemoto N, Kiyozaki H, Yamada S, Konishi F (March 2004). "Parathyroid adenoma without hyperparathyroidism". Japanese Journal of Clinical Oncology. 34 (3): 155–8. doi:10.1093/jjco/hyh028. PMID 15078912.
- ↑ Felsenfeld AJ, Rodríguez M, Aguilera-Tejero E (November 2007). "Dynamics of parathyroid hormone secretion in health and secondary hyperparathyroidism". Clinical Journal of the American Society of Nephrology. 2 (6): 1283–305. doi:10.2215/CJN.01520407. PMID 17942777.
- ↑ Hsi ED, Zukerberg LR, Yang WI, Arnold A (May 1996). "Cyclin D1/PRAD1 expression in parathyroid adenomas: an immunohistochemical study". The Journal of Clinical Endocrinology and Metabolism. 81 (5): 1736–9. doi:10.1210/jcem.81.5.8626826. PMID 8626826.
- ↑ Parathyroid adenoma. Canadian cancer society(2015). http://www.cancer.ca/en/cancer-information/cancer-type/parathyroid/parathyroid-cancer/benign-tumours/?region=on Accessed on December 29, 2015
- ↑ Parathyroid adenoma. Wikipedia(2015). https://en.wikipedia.org/wiki/Parathyroid_adenoma Accessed on December 29, 2015
- ↑ Goldstein RE, Billheimer D, Martin WH, Richards K (May 2003). "Sestamibi scanning and minimally invasive radioguided parathyroidectomy without intraoperative parathyroid hormone measurement". Annals of Surgery. 237 (5): 722–30, discussion 730–1. doi:10.1097/01.SLA.0000064362.58751.59. PMC 1514518. PMID 12724639.
- ↑ 7.0 7.1 7.2 7.3 Dsouza, Caren; Gopalakrishnan; Bhagavan, KR; Rakesh, K (2012). "Ectopic parathyroid adenoma". Thyroid Research and Practice. 9 (2): 68–70. doi:10.4103/0973-0354.96061.
- ↑ 8.0 8.1 8.2 8.3 Bellantone R, Raffaelli M, DE Crea C, Traini E, Lombardi CP (August 2011). "Minimally-invasive parathyroid surgery". Acta Otorhinolaryngologica Italica. 31 (4): 207–15. PMC 3203720. PMID 22065831.
- ↑ Zald PB, Hamilton BE, Larsen ML, Cohen JI (August 2008). "The role of computed tomography for localization of parathyroid adenomas". The Laryngoscope. 118 (8): 1405–10. doi:10.1097/MLG.0b013e318177098c. PMID 18528308.