Ovarian hyperstimulation syndrome: Difference between revisions
| (25 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
'''For patient information, click [[Ovarian hyperstimulation syndrome (patient information)|here]]''' | |||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = {{PAGENAME}} | | Name = {{PAGENAME}} | ||
| Image = | | Image = Ovarian-hyperstimulation-004.jpg | ||
| Caption = | | Caption = [http://www.radswiki.net Image courtesy of RadsWiki] | ||
| DiseasesDB = 32038 | | DiseasesDB = 32038 | ||
| ICD10 = {{ICD10|N|98|1|n|80}} | | ICD10 = {{ICD10|N|98|1|n|80}} | ||
| Line 8: | Line 9: | ||
| ICDO = | | ICDO = | ||
| OMIM = | | OMIM = | ||
| MedlinePlus = | | MedlinePlus = 007294 | ||
| eMedicineSubj = | | eMedicineSubj = | ||
| eMedicineTopic = | | eMedicineTopic = | ||
| MeshID = | | MeshID = | ||
}} | }} | ||
'''Ovarian hyperstimulation syndrome''' ('''OHSS''') is a complication from some forms of [[fertility medication]]. Most cases are mild, but a small proportion is | {{SI}} | ||
{{CMG}} | |||
==Overview== | |||
'''Ovarian hyperstimulation syndrome''' ('''OHSS''') is a complication from some forms of [[fertility medication]]. Most cases are mild, but a small proportion are severe. | |||
==Etiology== | |||
Ovarian hyperstimulation syndrome is usually iatrogenic secondary to ovarian stimulant drug therapy for infertility but may occur as a spontaneous event in pregnancy. | |||
===Drug Induced=== | |||
* [[Cetrorelix]] | |||
* [[Choriogonadotropin alfa]] | |||
* [[Follitropin beta]] | |||
* [[Urofollitropin]] | |||
==Symptoms== | ==Symptoms== | ||
Symptoms are | |||
Symptoms are classified into three categories: mild, moderate, and severe. | |||
* Mild symptoms include abdominal bloating and feeling of fullness, [[nausea]], [[diarrhea]], and slight [[weight gain]]. | |||
* Moderate symptoms include excessive [[weight gain]] (weight gain of greater than 2 pounds per day), increased abdominal girth, [[vomiting]], [[diarrhea]], darker urine, reduced urine output, excessive thirst, and dry skin and/or hair. | |||
* Severe symptoms are fullness/bloating above the waist, [[shortness of breath]], reduced urine output, calf and [[chest pain]]s, and lower [[abdominal pain]] (in addition to mild and moderate symptoms). | |||
==Classification== | ==Classification== | ||
| Line 23: | Line 46: | ||
==Complications== | ==Complications== | ||
OHSS may be complicated with ovarian torsion, ovarian rupture, thrombophlebitis and renal insufficiency. Symptoms generally resolve in 1 to 2 weeks, but will be more severe and persist longer if pregnancy is successful. This is likely due to the role of the [[corpus luteum]] | OHSS may be complicated with ovarian torsion, ovarian rupture, thrombophlebitis and renal insufficiency. Symptoms generally resolve in 1 to 2 weeks, but will be more severe and persist longer if pregnancy is successful. This is likely due to the role of the [[corpus luteum]] in sustaining the pregnancy before the [[placenta]] has fully developed. Typically, even in severe OHSS with a developing pregnancy, the duration does not extend beyond the first trimester. | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 29: | Line 52: | ||
OHSS is characterized by the presence of multiple luteinized cysts within the [[ovaries]] leading to ovarian enlargement and secondary complications. | OHSS is characterized by the presence of multiple luteinized cysts within the [[ovaries]] leading to ovarian enlargement and secondary complications. | ||
As the ovary undergoes a process of extensive luteinization, large amounts of [[estrogens]], [[progesterone]], and local [[cytokines]] are released. It | As the ovary undergoes a process of extensive luteinization, large amounts of [[estrogens]], [[progesterone]], and local [[cytokines]] are released. It has been hypothesized that [[vascular endothelial growth factor]] (VEGF) is a key substance that induces OHSS by making local [[capillaries]] "leaky", leading to a shift of fluids from the intravascular system to the abdominal and pleural cavity. Thus, while the patient accumulates fluid in the third space, primarily in the form of [[ascites]], she actually becomes hypovolemic and is at risk for respiratory, circulatory, and renal problems. Patients who are pregnant sustain the ovarian luteinization process by the production of hCG. | ||
==Epidemiology== | ==Epidemiology== | ||
Sporadic OHSS is very rare, and may have a genetic component. [[Clomifene|Clomifene citrate]] therapy can occasionally lead to OHSS, but the vast majority of cases develop after use of [[gonadotropin]] therapy (with administration of [[FSH]]), such as [[Pergonal]], and administration of [[Human chorionic gonadotropin|hCG]] to trigger [[ovulation]], often in conjunction with [[in vitro fertilisation|IVF]]. The frequency varies and depends on patient factors, management, and methods of surveillance. About 5% of treated patients may encounter moderate to severe OHSS. | Sporadic OHSS is very rare, and may have a genetic component. [[Clomifene|Clomifene citrate]] therapy can occasionally lead to OHSS, but the vast majority of cases develop after use of [[gonadotropin]] therapy (with administration of [[FSH]]), such as [[Pergonal]], and administration of [[Human chorionic gonadotropin|hCG]] to trigger [[ovulation]], often in conjunction with [[in vitro fertilisation|IVF]]. The frequency varies and depends on patient factors, management, and methods of surveillance. About 5% of treated patients may encounter moderate to severe OHSS. | ||
Mortality is low, but several fatal cases have been reported. | Mortality is low, but several fatal cases have been reported. | ||
==Diagnostic Findings== | |||
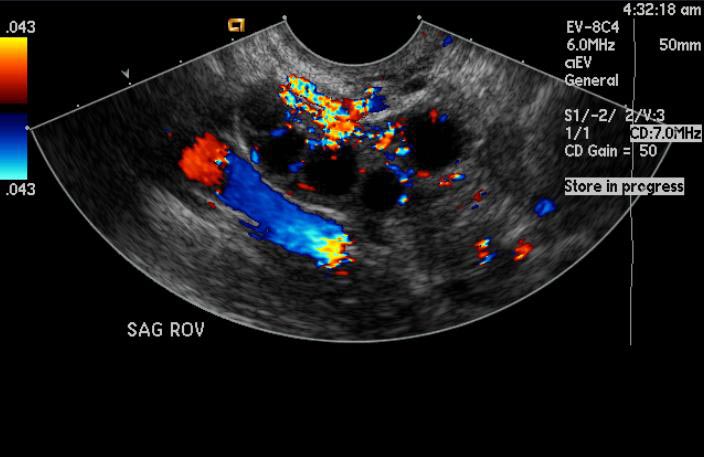
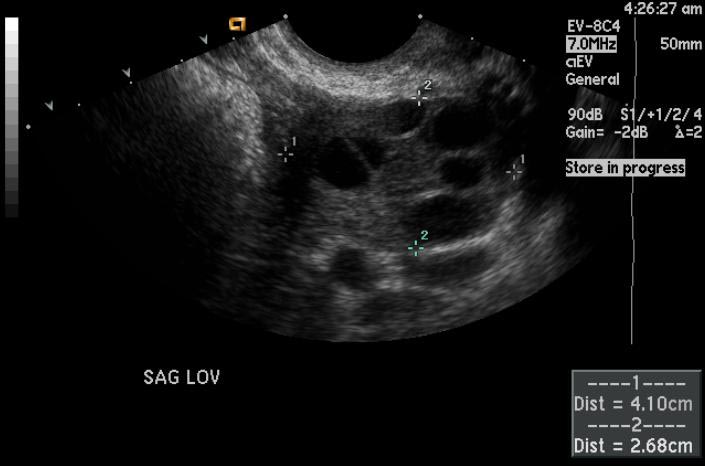
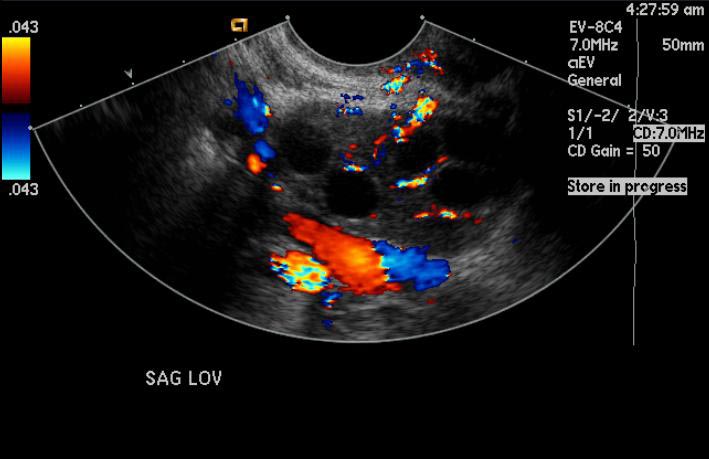
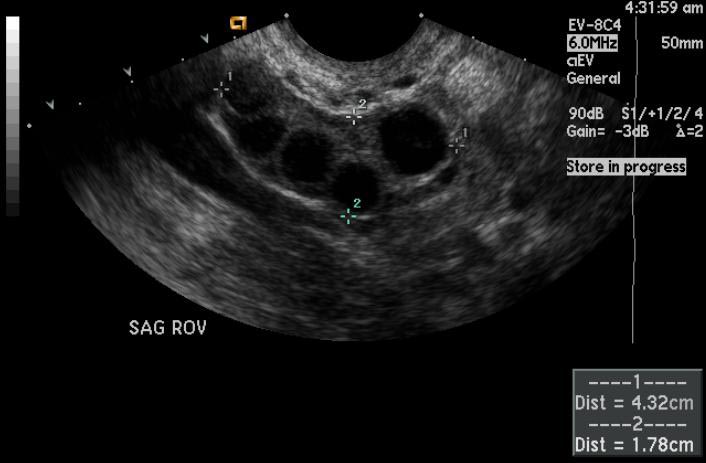
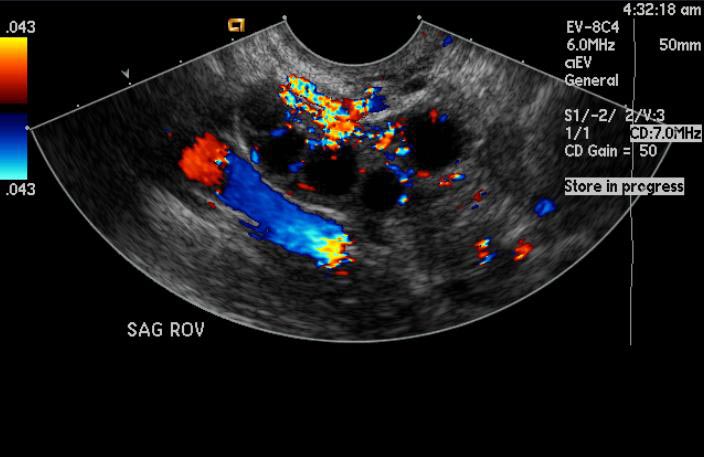
*The imaging findings are similar on ultrasound, CT, and MR imaging. | |||
*Ovarian enlargement is present caused by distended corpora lutea cysts of varying sizes. | |||
*Because the enlarged follicles are often peripheral in location, a '''"wheel spoke"''' appearance has been described, with stromal ovarian tissue located centrally with surrounding cysts. | |||
*Familiarity with ovarian hyperstimulation syndrome and the appropriate clinical setting should help avoid the incorrect diagnosis of an ovarian cystic neoplasm. | |||
[http://www.radswiki.net Images courtesy of RadsWiki] | |||
[[Image:Ovarian-hyperstimulation-001.jpg|left|thumb|250px|]] | |||
<br clear="left"/> | |||
[[Image:Ovarian-hyperstimulation-002.jpg|left|thumb|250px|]] | |||
<br clear="left"/> | |||
[[Image:Ovarian-hyperstimulation-003.jpg|left|thumb|250px|]] | |||
<br clear="left"/> | |||
[[Image:Ovarian-hyperstimulation-004.jpg|left|thumb|250px|]] | |||
<br clear="left"/> | |||
==Treatment== | ==Treatment== | ||
Physicians can reduce the risk of OHSS by monitoring of FSH therapy to use this medication judiciously, and by withholding hCG medication. Once OHSS develops, reduction in physical activity, closely monitoring fluid and electrolyte balance, and aspiration of accumulated fluid (ascites) from the abdominal/pleural cavity may be necessary, as well as opioids for the pain. If the OHSS develops within an IVF protocol, it can be prudent to postpone transfer of the pre-embryos since establishment of pregnancy can lengthen the recovery time or contribute to a more severe course. Over time, if carefully monitored, the condition will naturally reverse to normal - so treatment is typically supportive, although patient may need to be treated or hospitalized for pain, paracentesis, and/or intravenous hydration. | Physicians can reduce the risk of OHSS by monitoring of FSH therapy to use this medication judiciously, and by withholding hCG medication. Once OHSS develops, reduction in physical activity, closely monitoring fluid and electrolyte balance, and aspiration of accumulated fluid (ascites) from the abdominal/pleural cavity may be necessary, as well as opioids for the pain. If the OHSS develops within an IVF protocol, it can be prudent to postpone transfer of the pre-embryos since establishment of pregnancy can lengthen the recovery time or contribute to a more severe course. Over time, if carefully monitored, the condition will naturally reverse to normal - so treatment is typically supportive, although patient may need to be treated or hospitalized for pain, paracentesis, and/or intravenous hydration. | ||
| Line 43: | Line 86: | ||
* {{cite journal | author = Delvigne A, Rozenberg S | title = Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS). | journal = Hum Reprod Update | volume = 9 | issue = 1 | pages = 77-96 | year = 2003 | id = PMID 12638783 | url=http://humupd.oupjournals.org/cgi/reprint/9/1/77 | format=PDF}} | * {{cite journal | author = Delvigne A, Rozenberg S | title = Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS). | journal = Hum Reprod Update | volume = 9 | issue = 1 | pages = 77-96 | year = 2003 | id = PMID 12638783 | url=http://humupd.oupjournals.org/cgi/reprint/9/1/77 | format=PDF}} | ||
{{Diseases of the pelvis, genitals and breasts}} | |||
{{ | |||
[[de:Ovarielles Hyperstimulationssyndrom]] | [[de:Ovarielles Hyperstimulationssyndrom]] | ||
{{WH}} | |||
{{WikiDoc Sources}} | |||
[[Category:Disease]] | |||
[[Category:Gynecology]] | |||
Latest revision as of 19:12, 29 April 2015
For patient information, click here
| Ovarian hyperstimulation syndrome | |
 | |
|---|---|
| Image courtesy of RadsWiki | |
| ICD-10 | N98.1 |
| ICD-9 | xxx |
| DiseasesDB | 32038 |
| MedlinePlus | 007294 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ovarian hyperstimulation syndrome (OHSS) is a complication from some forms of fertility medication. Most cases are mild, but a small proportion are severe.
Etiology
Ovarian hyperstimulation syndrome is usually iatrogenic secondary to ovarian stimulant drug therapy for infertility but may occur as a spontaneous event in pregnancy.
Drug Induced
Symptoms
Symptoms are classified into three categories: mild, moderate, and severe.
- Mild symptoms include abdominal bloating and feeling of fullness, nausea, diarrhea, and slight weight gain.
- Moderate symptoms include excessive weight gain (weight gain of greater than 2 pounds per day), increased abdominal girth, vomiting, diarrhea, darker urine, reduced urine output, excessive thirst, and dry skin and/or hair.
- Severe symptoms are fullness/bloating above the waist, shortness of breath, reduced urine output, calf and chest pains, and lower abdominal pain (in addition to mild and moderate symptoms).
Classification
In mild forms of OHSS the ovaries are enlarged, in moderate forms there is additional accumulation of ascites with mild abdominal distension, while in severe forms of OHSS there may be hemoconcentration, thrombosis, abdominal pain and distension, oliguria (decreased urine production), pleural effusion, and respiratory distress. Early OHSS develops before pregnancy testing, and late OHSS is seen in early pregnancy.
Complications
OHSS may be complicated with ovarian torsion, ovarian rupture, thrombophlebitis and renal insufficiency. Symptoms generally resolve in 1 to 2 weeks, but will be more severe and persist longer if pregnancy is successful. This is likely due to the role of the corpus luteum in sustaining the pregnancy before the placenta has fully developed. Typically, even in severe OHSS with a developing pregnancy, the duration does not extend beyond the first trimester.
Pathophysiology
OHSS is characterized by the presence of multiple luteinized cysts within the ovaries leading to ovarian enlargement and secondary complications.
As the ovary undergoes a process of extensive luteinization, large amounts of estrogens, progesterone, and local cytokines are released. It has been hypothesized that vascular endothelial growth factor (VEGF) is a key substance that induces OHSS by making local capillaries "leaky", leading to a shift of fluids from the intravascular system to the abdominal and pleural cavity. Thus, while the patient accumulates fluid in the third space, primarily in the form of ascites, she actually becomes hypovolemic and is at risk for respiratory, circulatory, and renal problems. Patients who are pregnant sustain the ovarian luteinization process by the production of hCG.
Epidemiology
Sporadic OHSS is very rare, and may have a genetic component. Clomifene citrate therapy can occasionally lead to OHSS, but the vast majority of cases develop after use of gonadotropin therapy (with administration of FSH), such as Pergonal, and administration of hCG to trigger ovulation, often in conjunction with IVF. The frequency varies and depends on patient factors, management, and methods of surveillance. About 5% of treated patients may encounter moderate to severe OHSS.
Mortality is low, but several fatal cases have been reported.
Diagnostic Findings
- The imaging findings are similar on ultrasound, CT, and MR imaging.
- Ovarian enlargement is present caused by distended corpora lutea cysts of varying sizes.
- Because the enlarged follicles are often peripheral in location, a "wheel spoke" appearance has been described, with stromal ovarian tissue located centrally with surrounding cysts.
- Familiarity with ovarian hyperstimulation syndrome and the appropriate clinical setting should help avoid the incorrect diagnosis of an ovarian cystic neoplasm.
Treatment
Physicians can reduce the risk of OHSS by monitoring of FSH therapy to use this medication judiciously, and by withholding hCG medication. Once OHSS develops, reduction in physical activity, closely monitoring fluid and electrolyte balance, and aspiration of accumulated fluid (ascites) from the abdominal/pleural cavity may be necessary, as well as opioids for the pain. If the OHSS develops within an IVF protocol, it can be prudent to postpone transfer of the pre-embryos since establishment of pregnancy can lengthen the recovery time or contribute to a more severe course. Over time, if carefully monitored, the condition will naturally reverse to normal - so treatment is typically supportive, although patient may need to be treated or hospitalized for pain, paracentesis, and/or intravenous hydration.
References
- Delvigne A, Rozenberg S (2002). "Epidemiology and prevention of ovarian hyperstimulation syndrome (OHSS): a review" (PDF). Hum Reprod Update. 8 (6): 559–77. PMID 12498425.
- Delvigne A, Rozenberg S (2003). "Review of clinical course and treatment of ovarian hyperstimulation syndrome (OHSS)" (PDF). Hum Reprod Update. 9 (1): 77–96. PMID 12638783.
Template:Diseases of the pelvis, genitals and breasts
de:Ovarielles Hyperstimulationssyndrom Template:WH Template:WikiDoc Sources