Osteomyelitis
| Osteomyelitis | |
 | |
|---|---|
| Osteomyelitis of the tibia of a young child. Numerous abscesses in the bone show as radiolucency. | |
| ICD-10 | M86 |
| ICD-9 | 730 |
| DiseasesDB | 9367 |
| MedlinePlus | 000437 |
| eMedicine | ped/1677 |
| MeSH | D010019 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Osteomyelitis is an infection of bone or bone marrow, usually caused by pyogenic bacteria or mycobacteria. It can be usefully subclassifed on the basis of the causative organism, the route, duration and anatomic location of the infection.[1]
Etiology
| Age group | Most common organisms |
| Newborns (younger than 4 mo) | S. aureus, Enterobacter species, and group A and B Streptococcus species |
| Children (aged 4 mo to 4 y) | S. aureus, group A Streptococcus species, Haemophilus influenzae, and Enterobacter species |
| Children, adolescents (aged 4 y to adult) | S. aureus (80%), group A Streptococcus species, H. influenzae, and Enterobacter species |
| Adult | S. aureus and occasionally Enterobacter or Streptococcus species |
In children, the long bones are usually affected. In adults, the vertebrae and the pelvis are most commonly affected.
Acute osteomyelitis almost invariably occurs in children. When adults are affected, it may be because of compromised host resistance due to debilitation, intravenous drug abuse, infectious root-canaled teeth, or other disease or drugs (e.g. immunosuppressive therapy).
Osteomyelitis is a secondary complication in 1-3% of patients with pulmonary tuberculosis[1]. In this case, the bacteria generally spread to the bone through the circulatory system, first infecting the synovium (due to its higher oxygen concentration) before spreading to the adjacent bone[1]. In tubercular osteomyelitis, the long bones and vertebrae are the ones which tend to be affected[1].
Pathogenesis
Staphylococcus aureus is the organism most commonly isolated from all forms of osteomyelitis.[1]
Bloodstream-sourced osteomyelitis is seen most frequently in children, and nearly 90% of cases are caused by Staphylococcus aureus. In infants, S. aureus, Group B streptococci (most common[2]) and Escherichia coli are commonly isolated; in children from 1 to 16 years of age, S. aureus, Streptococcus pyogenes, and Haemophilus influenzae are common. In some subpopulations, including intravenous drug users and splenectomized patients, Gram-negative bacteria, including enteric bacteria, are significant pathogens.[3]
The most common form of the disease in adults is caused by injury exposing the bone to local infection. Staphylococcus aureus is again the most common organism seen in osteomyelitis seeded from areas of contiguous infection, but anaerobes and Gram-negative organisms, including Pseudomonas aeruginosa, E. coli, and Serratia marcescens, are also common, and mixed infections are the rule rather than the exception.[3]
Systemic mycotic (fungal) infections may also cause osteomyelitis. The two most common pathogens involved in such infections are Blastomyces dermatitidis and Coccidioides immitis.
In osteomyelitis involving the vertebral bodies, about half the cases are due to Staphylococcus aureus, and the other half are due to tuberculosis (spread hematogenously from the lungs). Tubercular osteomyelitis of the spine was so common before the initiation of effective antitubercular therapy that it acquired a special name, Pott's disease, by which it is sometimes still known. The Burkholderia cepacia complex have been implicated in vertebral osteomyelitis in intravenous drug abusers. [4]
Factors that may commonly complicate osteomyelitis are fractures of the bone, amyloidosis, endocarditis, or sepsis[1].
Presentation
Generally, microorganisms may infect bone through one or more of three basic methods: via the bloodstream, contiguously from local areas of infection (as in cellulitis), or penetrating trauma, including iatrogenic causes such as joint replacements or internal fixation of fractures or root-canaled teeth.[1] Once the bone is infected, leukocytes enter the infected area, and in their attempt to engulf the infectious organisms, release enzymes that lyse the bone. Pus spreads into the bone's blood vessels, impairing their flow, and areas of devitalized infected bone, known as sequestra, form the basis of a chronic infection.[1] Often, the body will try to create new bone around the area of necrosis. The resulting new bone is often called an involucrum.[1] On histologic examination, these areas of necrotic bone are the basis for distinguishing between acute osteomyelitis and chronic osteomyelitis. Osteomyelitis is an infective process which encompasses all of the bone (osseous) components, including the bone marrow. When it is chronic it can lead to bone sclerosis and deformity.
In infants, the infection can spread to the joint and cause arthritis. In children, large subperiosteal abscesses can form because the periosteum is loosely attached to the surface of the bone.[1]
Because of the particulars of their blood supply, the tibia, femur, humerus, vertebra, the maxilla, and the mandibular bodies are especially susceptible to osteomyelitis.[5] However, abscesses of any bone may be precipitated by trauma to the affected area. Many infections are caused by Staphylococcus aureus, a member of the normal flora found on the skin and mucous membranes.
- Hematogenous long-bone osteomyelitis
- Abrupt onset of high fever (fever is present in only 50% of neonates with osteomyelitis)
- Fatigue
- Irritability
- Malaise
- Restriction of movement (pseudoparalysis of limb in neonates)
- Local edema, erythema, and tenderness
- Hematogenous vertebral osteomyelitis
- Insidious onset
- History of an acute bacteremic episode
- May be associated with contiguous vascular insufficiency
- Local edema, erythema, and tenderness
- Failure of a young child to sit up normally2
- Chronic osteomyelitis
- Non-healing ulcer
- Sinus tract drainage
- Chronic fatigue
- Malaise
Complete Differential Diagnosis of Associated Conditions
- Bacteroides
- Decubitus
- Diabetic angiopathy
- E.Coli
- Gastrointestinal infection
- Klebsiella
- Otitis
- Pneumonia
- Pseudomonas
- Serratia
- Sinusitis
- Skin infection
- Staphylococcus aureus
- Staphylococcus epidermidis
- Streptococcus pyogenes
- Streptococcus pneumoniae
- Tonsilitis
- Urinary tract infection
- Vasculitis [6] [7]
Diagnosis
Diagnosis of osteomyelitis is often based on radiologic results showing a lytic center with a ring of sclerosis, though bone cultures are normally required to identify the specific pathogen[1].
Diagnostic Findings
- Conventional radiographic evaluation of acute osteomyelitis is insufficient because bone changes are not evident for 14–21 days after the onset of infection.
- Although MR imaging is the accepted modality of choice for the early detection and surgical localization of osteomyelitis, in the emergency department, CT is usually more readily available for establishing the diagnosis. [8]
- At CT, features of bacterial osteomyelitis include overlying soft-tissue swelling, periosteal reaction, medullary low-attenuation areas or trabecular coarsening, and focal cortical erosions.
MRI
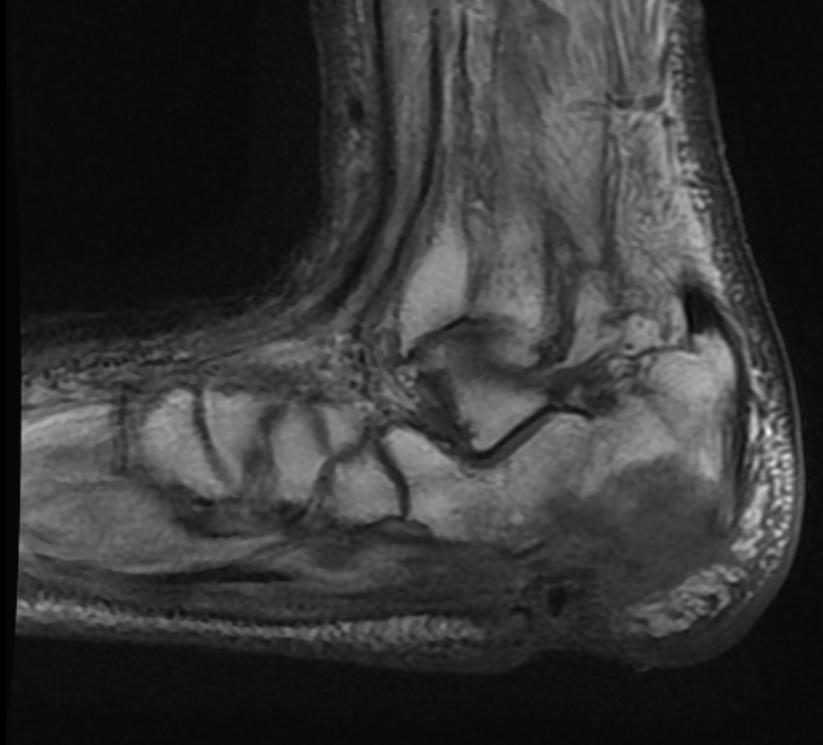
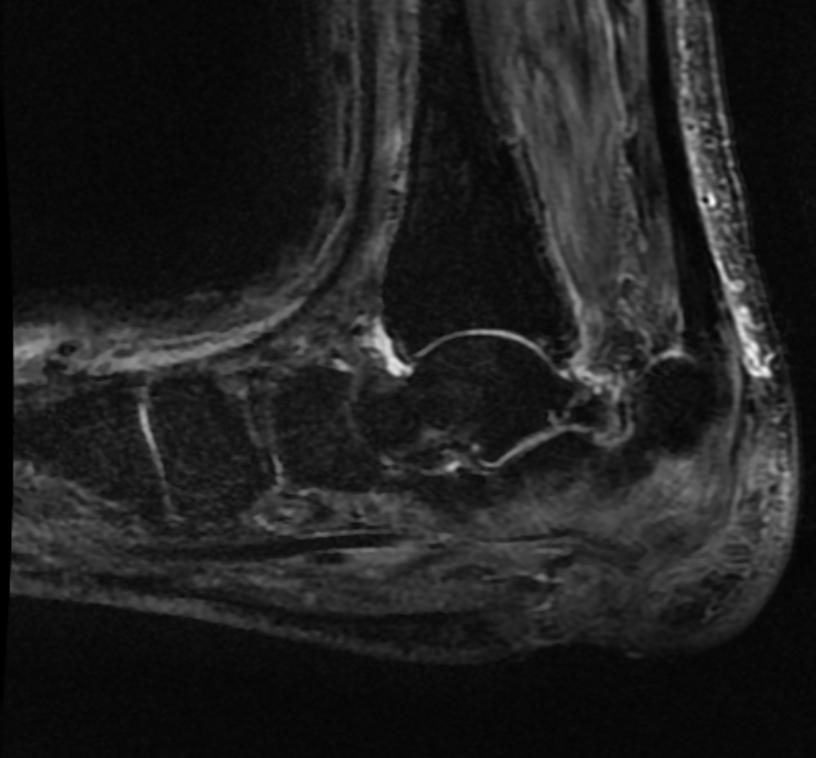
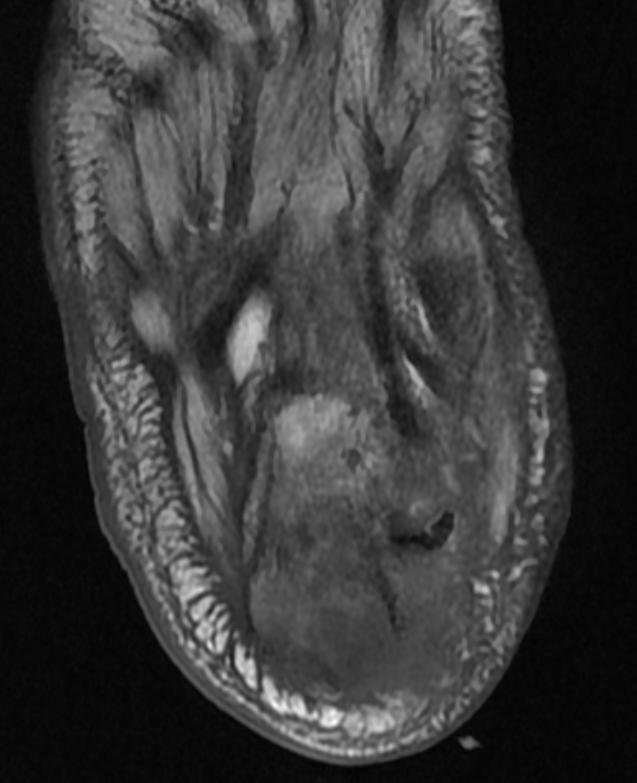
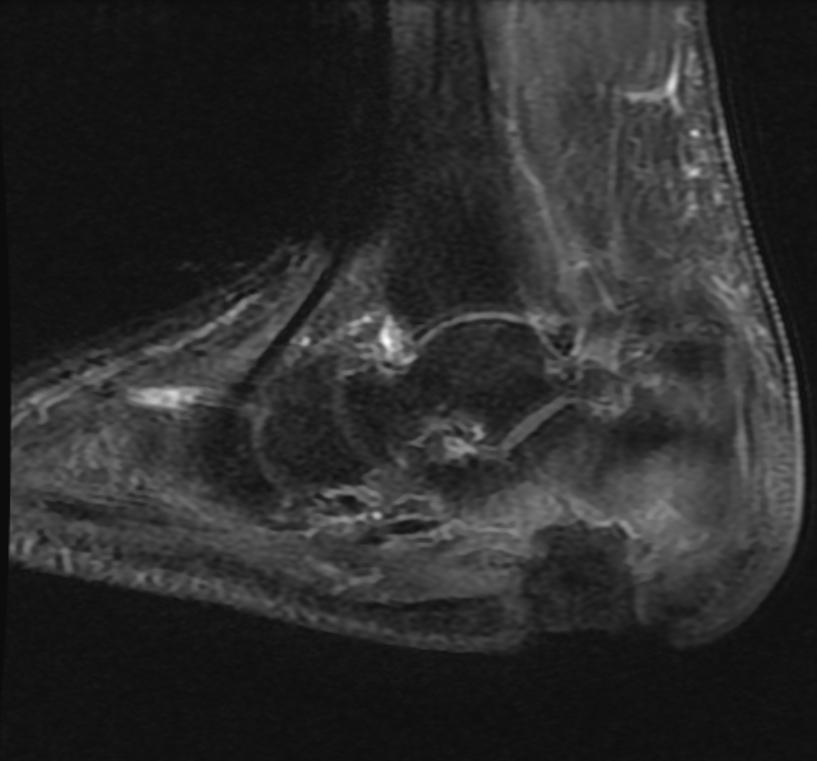
Patient #1 Extensive calcaneal osteomyelitis. Note soft tissue ulceration and cellulitis
-
T1
-
STIR
-
T1
-
STIR
-
T1 fat sat contrast
-
T1 fat sat contrast
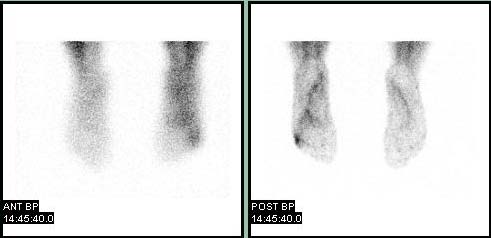
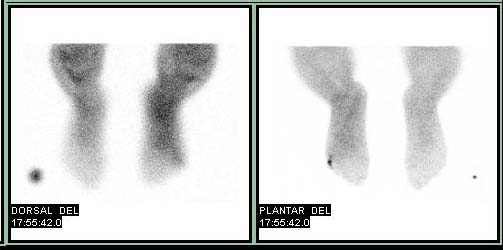
Bone Scan
Patient #2
-
Blood pool
-
Delayed
<youtube v=X2ShDUfeso0/>
Pathological Findings

Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology.
Osteomyelitis and Chondritis of Vertebrae
<youtube v=KTfOwYS1ykY/>
Treatment
Osteomyelitis often requires prolonged antibiotic therapy, with a course lasting a matter of weeks or months. A PICC line or central venous catheter is often placed for this purpose. Osteomyelitis also may require surgical debridement. Severe cases may lead to the loss of a limb. Initial first line antibiotic choice is determined by the patient's history and regional differences in common infective organisms.
Prior to the widespread availability and use of antibiotics, blow fly larvae were sometimes deliberately introduced to the wounds to feed on the infected material, effectively scouring them clean. [9][10]
Hyperbaric oxygen therapy has been shown to be a useful adjunct to the treatment of refractory osteomyelitis.[11][12] A treatment lasting 42 days is practiced in a number of facilities.[13]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; & Mitchell, Richard N. (2007). Robbins Basic Pathology (8th ed.). Saunders Elsevier. pp. 810-811 ISBN 978-1-4160-2973-1
- ↑ Haggerty, Maureen (2002). "Streptococcal Infections". Gale Encyclopedia of Medicine. The Gale Group. Retrieved 2008-03-14.
- ↑ 3.0 3.1 Carek, P.J. (2001-06-15). "Diagnosis and management of osteomyelitis". Am Fam Physician. 63 (12): 2413–20. Unknown parameter
|coauthors=ignored (help) - ↑ Weinstein, Lenny (2007-12-16). "Cervical osteomyelitis caused by Burkholderia cepacia after rhinoplasty". J Infect Developing Countries. 2 (1): 76–77. ISSN 1972-2680. Unknown parameter
|coauthors=ignored (help) - ↑ King MD, Randall W. (2006-07-13). "Osteomyelitis". eMedicine. WebMD. Retrieved 2007-11-11. Unknown parameter
|coauthors=ignored (help) - ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Laura M. Fayad, John A. Carrino, and Elliot K. Fishman. Musculoskeletal Infection: Role of CT in the Emergency Department. RadioGraphics 2007 27: 1723-1736.
- ↑ Baer M.D., William S. (1931). "The Treatment of Chronic Osteomyelitis with the Maggot (Larva of the Blow Fly)". Journal of Bone and Joint Surgery. 13: 438–475. Retrieved 2007-11-12.
- ↑ McKeever, Duncan Clark (2008). "The classic: maggots in treatment of osteomyelitis: a simple inexpensive method. 1933". Clin. Orthop. Relat. Res. 466 (6): 1329–35. doi:10.1007/s11999-008-0240-5. PMID 18404291. Unknown parameter
|quotes=ignored (help); Unknown parameter|month=ignored (help) - ↑ Mader JT, Adams KR, Sutton TE (1987). "Infectious diseases: pathophysiology and mechanisms of hyperbaric oxygen". J. Hyperbaric Med. 2 (3): 133–140. Retrieved 2008-05-16.
- ↑ Kawashima M, Tamura H, Nagayoshi I, Takao K, Yoshida K, Yamaguchi T (2004). "Hyperbaric oxygen therapy in orthopedic conditions". Undersea Hyperb Med. 31 (1): 155–62. PMID 15233171. Retrieved 2008-05-16.
- ↑ Putland M.D, Michael S., Hyperbaric Medicine, Capital Regional Medical Center, Tallahassee, Florida, personal inquiry June 2008.
See also
External Links
Additional Resources
Template:Diseases of the musculoskeletal system and connective tissue
de:Osteomyelitis it:Osteomielite nl:Osteomyelitis no:Ostomyelitt