Osteomyelitis: Difference between revisions
No edit summary |
|||
| Line 18: | Line 18: | ||
{{CMG}}'''; Associate Editor(s)-In-Chief:''' {{CZ}} | {{CMG}}'''; Associate Editor(s)-In-Chief:''' {{CZ}} | ||
== Presentation == | == Presentation == | ||
| Line 118: | Line 94: | ||
{{#ev:youtube|X2ShDUfeso0}} | {{#ev:youtube|X2ShDUfeso0}} | ||
<br clear="left"/> | <br clear="left"/> | ||
==Treatment== | ==Treatment== | ||
Revision as of 15:54, 27 November 2012
For patient information click here
| Osteomyelitis | |
 | |
|---|---|
| Osteomyelitis of the tibia of a young child. Numerous abscesses in the bone show as radiolucency. | |
| ICD-10 | M86 |
| ICD-9 | 730 |
| DiseasesDB | 9367 |
| MedlinePlus | 000437 |
| MeSH | D010019 |
|
Osteomyelitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteomyelitis On the Web |
|
American Roentgen Ray Society Images of Osteomyelitis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Presentation
Generally, microorganisms may infect bone through one or more of three basic methods: via the bloodstream, contiguously from local areas of infection (as in cellulitis), or penetrating trauma, including iatrogenic causes such as joint replacements or internal fixation of fractures or root-canaled teeth.[1] Once the bone is infected, leukocytes enter the infected area, and in their attempt to engulf the infectious organisms, release enzymes that lyse the bone. Pus spreads into the bone's blood vessels, impairing their flow, and areas of devitalized infected bone, known as sequestra, form the basis of a chronic infection.[1] Often, the body will try to create new bone around the area of necrosis. The resulting new bone is often called an involucrum.[1] On histologic examination, these areas of necrotic bone are the basis for distinguishing between acute osteomyelitis and chronic osteomyelitis. Osteomyelitis is an infective process which encompasses all of the bone (osseous) components, including the bone marrow. When it is chronic it can lead to bone sclerosis and deformity.
In infants, the infection can spread to the joint and cause arthritis. In children, large subperiosteal abscesses can form because the periosteum is loosely attached to the surface of the bone.[1]
Because of the particulars of their blood supply, the tibia, femur, humerus, vertebra, the maxilla, and the mandibular bodies are especially susceptible to osteomyelitis.[2] However, abscesses of any bone may be precipitated by trauma to the affected area. Many infections are caused by Staphylococcus aureus, a member of the normal flora found on the skin and mucous membranes.
- Hematogenous long-bone osteomyelitis
- Abrupt onset of high fever (fever is present in only 50% of neonates with osteomyelitis)
- Fatigue
- Irritability
- Malaise
- Restriction of movement (pseudoparalysis of limb in neonates)
- Local edema, erythema, and tenderness
- Hematogenous vertebral osteomyelitis
- Insidious onset
- History of an acute bacteremic episode
- May be associated with contiguous vascular insufficiency
- Local edema, erythema, and tenderness
- Failure of a young child to sit up normally2
- Chronic osteomyelitis
- Non-healing ulcer
- Sinus tract drainage
- Chronic fatigue
- Malaise
Diagnosis
Diagnosis of osteomyelitis is often based on radiologic results showing a lytic center with a ring of sclerosis, though bone cultures are normally required to identify the specific pathogen[1].
Diagnostic Findings
- Conventional radiographic evaluation of acute osteomyelitis is insufficient because bone changes are not evident for 14–21 days after the onset of infection.
- Although MR imaging is the accepted modality of choice for the early detection and surgical localization of osteomyelitis, in the emergency department, CT is usually more readily available for establishing the diagnosis. [3]
- At CT, features of bacterial osteomyelitis include overlying soft-tissue swelling, periosteal reaction, medullary low-attenuation areas or trabecular coarsening, and focal cortical erosions.
MRI
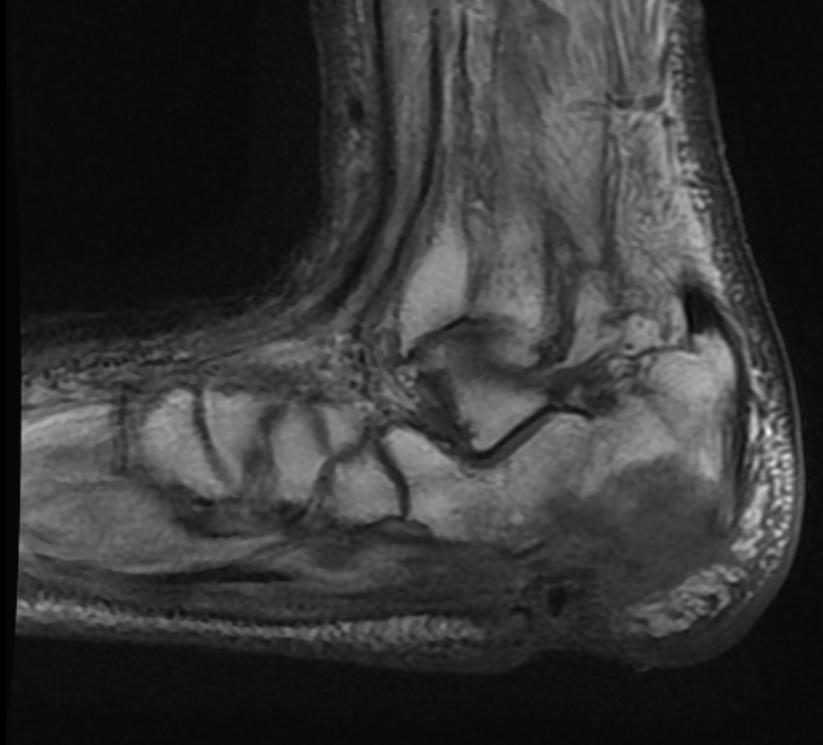
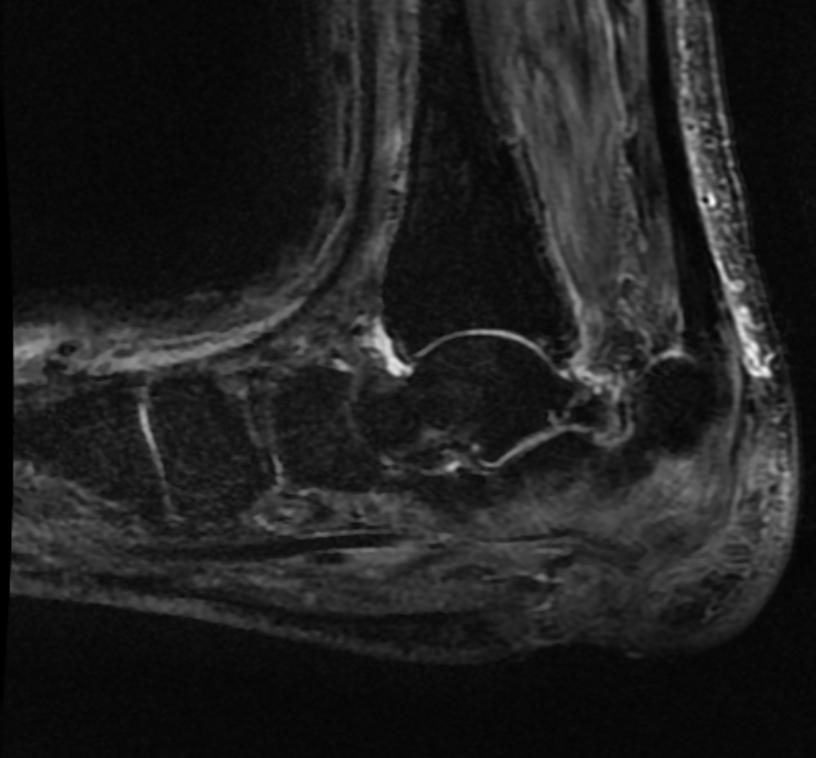
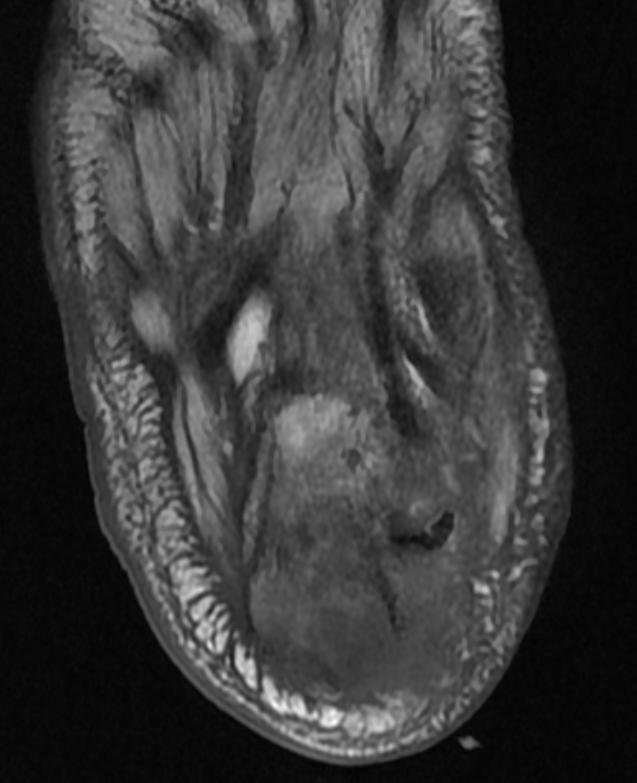
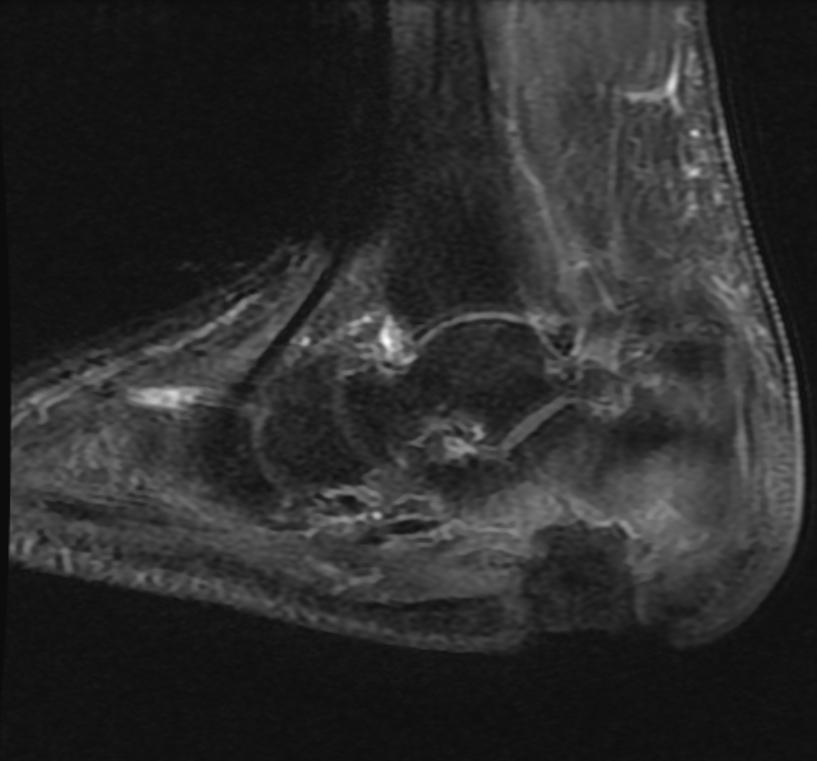
Patient #1 Extensive calcaneal osteomyelitis. Note soft tissue ulceration and cellulitis
-
T1
-
STIR
-
T1
-
STIR
-
T1 fat sat contrast
-
T1 fat sat contrast
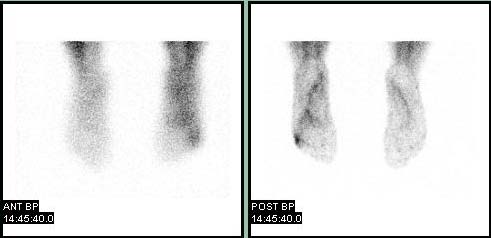
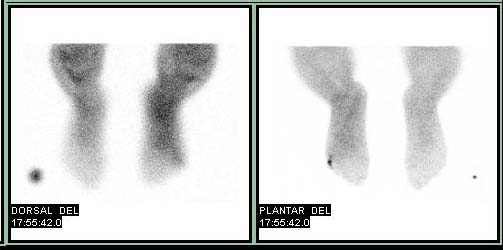
Bone Scan
Patient #2
-
Blood pool
-
Delayed
{{#ev:youtube|X2ShDUfeso0}}
Treatment
Osteomyelitis often requires prolonged antibiotic therapy, with a course lasting a matter of weeks or months. A PICC line or central venous catheter is often placed for this purpose. Osteomyelitis also may require surgical debridement. Severe cases may lead to the loss of a limb. Initial first line antibiotic choice is determined by the patient's history and regional differences in common infective organisms.
Prior to the widespread availability and use of antibiotics, blow fly larvae were sometimes deliberately introduced to the wounds to feed on the infected material, effectively scouring them clean. [4][5]
Hyperbaric oxygen therapy has been shown to be a useful adjunct to the treatment of refractory osteomyelitis.[6][7] A treatment lasting 42 days is practiced in a number of facilities.[8]
References
- ↑ 1.0 1.1 1.2 1.3 1.4
- ↑ King MD, Randall W. (2006-07-13). "Osteomyelitis". eMedicine. WebMD. Retrieved 2007-11-11. Unknown parameter
|coauthors=ignored (help) - ↑ Laura M. Fayad, John A. Carrino, and Elliot K. Fishman. Musculoskeletal Infection: Role of CT in the Emergency Department. RadioGraphics 2007 27: 1723-1736.
- ↑ Baer M.D., William S. (1931). "The Treatment of Chronic Osteomyelitis with the Maggot (Larva of the Blow Fly)". Journal of Bone and Joint Surgery. 13: 438–475. Retrieved 2007-11-12.
- ↑ McKeever, Duncan Clark (2008). "The classic: maggots in treatment of osteomyelitis: a simple inexpensive method. 1933". Clin. Orthop. Relat. Res. 466 (6): 1329–35. doi:10.1007/s11999-008-0240-5. PMID 18404291. Unknown parameter
|quotes=ignored (help); Unknown parameter|month=ignored (help) - ↑ Mader JT, Adams KR, Sutton TE (1987). "Infectious diseases: pathophysiology and mechanisms of hyperbaric oxygen". J. Hyperbaric Med. 2 (3): 133–140. Retrieved 2008-05-16.
- ↑ Kawashima M, Tamura H, Nagayoshi I, Takao K, Yoshida K, Yamaguchi T (2004). "Hyperbaric oxygen therapy in orthopedic conditions". Undersea Hyperb Med. 31 (1): 155–62. PMID 15233171. Retrieved 2008-05-16.
- ↑ Putland M.D, Michael S., Hyperbaric Medicine, Capital Regional Medical Center, Tallahassee, Florida, personal inquiry June 2008.
See also
External Links
Additional Resources
Template:Diseases of the musculoskeletal system and connective tissue
de:Osteomyelitis it:Osteomielite nl:Osteomyelitis no:Ostomyelitt