Oral cancer pathophysiology: Difference between revisions
Sargun Walia (talk | contribs) |
Sargun Walia (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Oral cancer}} | {{Oral cancer}} | ||
{{CMG}};{{AE}}{{SSW}} | {{CMG}};{{AE}}{{SSW}}, {{Simrat}} | ||
==Overview== | ==Overview== | ||
It is understood that oral cancer occur as a the result of carcinogen-metabolizing enzymes, alcohol, tobacco and genetic factors. [[Cytotoxicity|Cytotoxic]] enzymes such as [[alcohol dehydrogenase]] result in the production of free radicles and [[DNA]] hydroxylated bases. [[Alcohol dehydrogenase]] oxidizes [[ethanol]] to [[acetaldehyde]] which is [[Cytotoxicity|cytotoxic]] in nature. Cigarette smoke has various carcinogens which can lead to oral cancers. Low reactive free radicals in cigarette smoke interact with redox-active metals in saliva.The development of oral cancer is the result of multiple genetic mutations.These mutations occur in [[Tumor suppressor genes|tumor suppressor genes (TSGs)]] and [[Oncogene|oncogenes]]. [[Squamous cell carcinoma]] is the most common malignancy of the oral cavity. It typically has three gross morphologic growth patterns: exophytic, [[Ulcerated lesion|ulcerative]], and infiltrative. Microscopically, oral cancers are broadly based and invasive through [[papillary]] fronds. Oral cancer constitutes of highly differentiated squamous cells lacking frank cytologic criteria of [[malignancy]] with rare [[Mitosis|mitoses]].The surface of the lesion is covered with compressed invaginating folds of [[keratin]] layers. A stroma-like inflammatory reaction and a blunt pushing margin may be seen. | It is understood that oral cancer occur as a the result of carcinogen-metabolizing enzymes, alcohol, tobacco and genetic factors. [[Cytotoxicity|Cytotoxic]] enzymes such as [[alcohol dehydrogenase]] result in the production of free radicles and [[DNA]] hydroxylated bases. [[Alcohol dehydrogenase]] oxidizes [[ethanol]] to [[acetaldehyde]] which is [[Cytotoxicity|cytotoxic]] in nature. Cigarette smoke has various carcinogens which can lead to oral cancers. Low reactive free radicals in cigarette smoke interact with redox-active metals in saliva.The development of oral cancer is the result of multiple genetic mutations.These mutations occur in [[Tumor suppressor genes|tumor suppressor genes (TSGs)]] and [[Oncogene|oncogenes]]. [[Squamous cell carcinoma]] is the most common malignancy of the oral cavity. It typically has three gross morphologic growth patterns: exophytic, [[Ulcerated lesion|ulcerative]], and infiltrative. Microscopically, oral cancers are broadly based and invasive through [[papillary]] fronds. Oral cancer constitutes of highly differentiated squamous cells lacking frank cytologic criteria of [[malignancy]] with rare [[Mitosis|mitoses]].The surface of the lesion is covered with compressed invaginating folds of [[keratin]] layers. A stroma-like inflammatory reaction and a blunt pushing margin may be seen. | ||
Revision as of 13:42, 9 February 2018
|
Oral cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Oral cancer pathophysiology |
|
Risk calculators and risk factors for Oral cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Sargun Singh Walia M.B.B.S.[2], Simrat Sarai, M.D. [3]
Overview
It is understood that oral cancer occur as a the result of carcinogen-metabolizing enzymes, alcohol, tobacco and genetic factors. Cytotoxic enzymes such as alcohol dehydrogenase result in the production of free radicles and DNA hydroxylated bases. Alcohol dehydrogenase oxidizes ethanol to acetaldehyde which is cytotoxic in nature. Cigarette smoke has various carcinogens which can lead to oral cancers. Low reactive free radicals in cigarette smoke interact with redox-active metals in saliva.The development of oral cancer is the result of multiple genetic mutations.These mutations occur in tumor suppressor genes (TSGs) and oncogenes. Squamous cell carcinoma is the most common malignancy of the oral cavity. It typically has three gross morphologic growth patterns: exophytic, ulcerative, and infiltrative. Microscopically, oral cancers are broadly based and invasive through papillary fronds. Oral cancer constitutes of highly differentiated squamous cells lacking frank cytologic criteria of malignancy with rare mitoses.The surface of the lesion is covered with compressed invaginating folds of keratin layers. A stroma-like inflammatory reaction and a blunt pushing margin may be seen.
Pathophysiology
- It is understood that oral cancer occur as a the result of carcinogen-metabolizing enzymes, alcohol, tobacco and genetic factors.
Carcinogen-metabolizing enzymes
- Carcinogen-metabolizing enzymes are known to cause cancer in some patients.
- Cytotoxic enzymes such as alcohol dehydrogenase result in the production of:
- Free radicles
- DNA hydroxylated bases
- These cytotoxic enzymes especially predispose oral squamous cell carcinoma.
Alcohol
- Alcohol dehydrogenase oxidizes ethanol to acetaldehyde which is cytotoxic in nature.
- cytochrome P450 IIEI (CYP2E1) also metabolizes ethanol to acetaldehyde.
- Alcohol dehydrogenase type 3 genotype predisposes to oral squamous cell carcinoma.
- Carcinogenic potential increases when combined with tobacco use.
Tobacco
- Cigarette smoke has various carcinogens which can lead to oral cancers.
- Low reactive free radicals in cigarette smoke interact with redox-active metals in saliva.
- This makes saliva to loose its antioxidant potential and become a potent pro-oxidant milieu.[1]
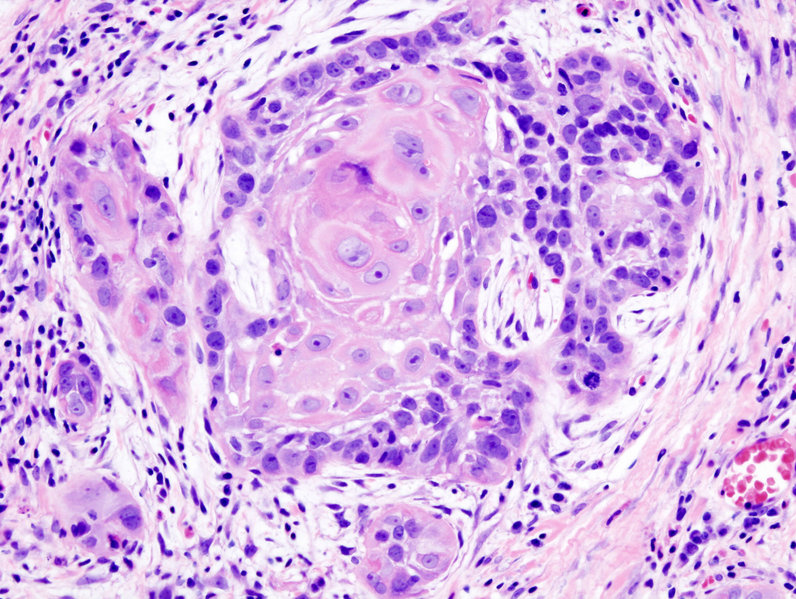
Pathology of classical or conventional squamous cell carcinoma
- Most cancers of the oral cavity are classical or conventional squamous cell carcinoma.
- This type of SCC starts in the squamous epithelium that lines the oral cavity and occurs most often on the lower lip, tongue and floor of the mouth.
- The microscopic features of classical SCC include:
- Epithelial pearls
- These are circular layers of squamous cells around a collection of keratin (a tough fibrous protein) in the centre.
- Epithelial pearls
- The cancer starts in the squamous cells of the epithelium and invades the deeper layers of the oral cavity.
Pathology of variants of squamous cell carcinoma
- These squamous cell carcinomas have distinct microscopic features that make them look and behave differently from classical SCC.
- Verrucous carcinoma
- These tumours make up less than 5% of all oral cavity tumours.
- They have a wart-like appearance and develop most often on the gums (gingiva), lining of the cheeks (buccal mucosa) and larynx.
- Verrucous carcinomas are low grade, slow growing and rarely spread.
- They are associated with the chronic use of snuff or chewing tobacco.
- Basaloid SCC
- This is a rare but aggressive subtype of squamous cell carcinoma.
- It is more common in men older than 60 years.
- Papillary SCC
- This is a rare subtype of squamous cell carcinoma that grows outward from the surface of the epithelium (exophytic).
- HPV infection may have a role in the development of this type of cancer.
- Spindle cell carcinoma (SpCC)
- This is an aggressive, rare variant of squamous cell carcinoma.
- These tumors contain a mixture of conventional squamous cell carcinoma and spindle cells that resemble a sarcoma.
It is also known as sarcomatoid carcinoma, pseudosarcoma, carcinosarcoma, pleomorphic carcinoma, metaplastic carcinoma, collision tumor and Lane tumor.
- Acantholytic SCC
- This is a rare variant of SCC in which the connections between the malignant squamous cells break down.
- This results in microscopic spaces in the tumour tissue, which appear like glands or vascular spaces.
- Adenosquamous carcinoma
- This is a very rare, aggressive type of squamous cell carcinoma.
- It looks like classical squamous cell carcinoma, but also has mucus-containing gland cells.
- Lymphoepithelial carcinoma
- This is a rare subtype of squamous cell carcinoma.
- The microscopic appearance is similar to undifferentiated nasopharyngeal carcinoma.
- It is also called undifferentiated carcinoma.
Genetics
- The development of oral cancer is the result of multiple genetic mutations.
- These mutations include:
- Tumor suppressor genes (TSGs)
- Oncogenes
Tumor suppressor genes (TSGs)
- Oral cavity cancer may be the result of allelic imbalance which is caused by chromosomal changes particularly in chromosome 3,9,11 and 17.
- These changes lead to mutation in tumor suppressor genes (TSGs).
- Normally TSGs modulate normal growth.
- Mutation of these TSGs leads to dysfunctional growth control.
- Mutation most commonly occurs in either of the following:
- Short arm of chromosome 3
- TSG termed P16 on chromosome 9
- TSG termed TP53 on chromosome 17
- Cytochrome P450 genotypes is related to mutations in some TSGs and lead to oral squamous cell carcinoma.
- In western countries (eg, United Kingdom, United States, Australia) TP53 mutations are the most common molecular change that leads to oral squamous cell carcinoma.
Oncogenes
- Cancer may also occur if there is mutation to other genes that control cell growth, mainly oncogenes.
- Oncogenes most commonly involved are:
- Chromosome 11 (PRAD1)
- Chromosome 17 (Harvey ras [H-ras])
- In eastern countries (eg, India, Southeast Asia), ras oncogenes is a more common cause of oral squamous cell carcinoma.
Gross Pathology
- Squamous cell carcinoma is the most common malignancy of the oral cavity.
- It typically has three gross morphologic growth patterns: exophytic, ulcerative, and infiltrative.
- The infiltrative and ulcerative are the types most commonly observed in the oral cavity.
- The macroscopic appearance of oral cancer depends on the following:
- Duration of the lesion
- The amount of keratinization
- The changes in the adjoining mucosa
- A fully developed oral cavity lesion appears as an exophytic bulky lesion that is gray to grayish-red and has a rough, shaggy, or papillomatous surface.

Microscopic Pathology
- Microscopically, oral cancers are broadly based and invasive through papillary fronds.
- Oral cancer constitutes of highly differentiated squamous cells lacking frank cytologic criteria of malignancy with rare mitoses.
- The surface of the lesion is covered with compressed invaginating folds of keratin layers.
- A stroma-like inflammatory reaction and a blunt pushing margin may be seen.
- SCC is subdivided by the WHO into:[2]
- Keratinizing type: Worst prognosis.
- Undifferentiated type: Intermediate prognosis, EBV association.[3]
- Nonkeratinizing type: Good prognosis, EBV association.
References
- ↑ Nagler R, Dayan D (2006). "The dual role of saliva in oral carcinogenesis". Oncology. 71 (1–2): 10–7. doi:10.1159/000100445. PMID 17344667.
- ↑ Peterson BR, Nelson BL (2013). "Nonkeratinizing undifferentiated nasopharyngeal carcinoma". Head Neck Pathol. 7 (1): 73–5. doi:10.1007/s12105-012-0401-4. PMC 3597164. PMID 23015393.
- ↑ Pathmanathan R, Prasad U, Chandrika G, Sadler R, Flynn K, Raab-Traub N (1995). "Undifferentiated, nonkeratinizing, and squamous cell carcinoma of the nasopharynx. Variants of Epstein-Barr virus-infected neoplasia". Am J Pathol. 146 (6): 1355–67. PMC 1870892. PMID 7778675.