Onchocerciasis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
m (Changes made per Mahshid's request) |
||
| (15 intermediate revisions by 4 users not shown) | |||
| Line 17: | Line 17: | ||
}} | }} | ||
{{Onchocerciasis}} | {{Onchocerciasis}} | ||
'''For patient information, click [[Onchocerciasis (patient information)|here]]''' | |||
''' | |||
{{CMG}} {{AE}} {{KD}} | |||
{{SK}} Onchocercosis; river blindness; Robles disease; onchocerca volvulus infection | |||
==[[Onchocerciasis overview|Overview]]== | |||
==[[Onchocerciasis historical perspective|Historical Perspective]]== | |||
== | ==[[Onchocerciasis classification|Classification]]== | ||
==[[Onchocerciasis pathophysiology|Pathophysiology]]== | |||
==[[Onchocerciasis causes|Causes]]== | |||
==[[Onchocerciasis differential diagnosis|Differentiating Onchocerciasis from other Diseases]]== | |||
== | ==[[Onchocerciasis epidemiology and demographics|Epidemiology and Demographics]]== | ||
==[[Onchocerciasis risk factors|Risk Factors]]== | |||
==[[Onchocerciasis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== | |||
==Diagnosis== | |||
[[Onchocerciasis history and symptoms| History and Symptoms]] | [[Onchocerciasis physical examination | Physical Examination]] | [[Onchocerciasis laboratory findings|Laboratory Findings]] | [[Onchocerciasis other diagnostic studies|Other Diagnostic Studies]] | |||
==Treatment== | |||
[[Onchocerciasis medical therapy|Medical Therapy]] | [[Onchocerciasis primary prevention|Primary Prevention]] | [[Onchocerciasis cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Onchocerciasis future or investigational therapies|Future or Investigational Therapies]] | |||
===Antimicrobial therapy=== | |||
:* '''Cutaneous filariasis - Onchocercia volvulus, Loa loa'''<ref name="pmid20739055">{{cite journal| author=Taylor MJ, Hoerauf A, Bockarie M| title=Lymphatic filariasis and onchocerciasis. | journal=Lancet | year= 2010 | volume= 376 | issue= 9747 | pages= 1175-85 | pmid=20739055 | doi=10.1016/S0140-6736(10)60586-7 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20739055 }} </ref><ref name="pmid22632644">{{cite journal| author=Knopp S, Steinmann P, Hatz C, Keiser J, Utzinger J| title=Nematode infections: filariases. | journal=Infect Dis Clin North Am | year= 2012 | volume= 26 | issue= 2 | pages= 359-81 | pmid=22632644 | doi=10.1016/j.idc.2012.02.005 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22632644 }} </ref> | |||
::* Preferred regimen (1): [[Doxycycline]] 150 μg/kg single dose | |||
::* Preferred regimen (2): ([[Doxycycline]] 100 mg PO qd for 6 weeks {{or}} 200 mg PO qd for 4 weeks) {{then}} [[Ivermectin]] after 4-6 months 150 μg/kg single dose | |||
::* Preferred regimen (3): [[Doxycycline]] 200 mg PO qd for 6 weeks {{then}} [[Ivermectin]] after 4-6 months 150 μg/kg single dose | |||
==Case Studies== | |||
[[Onchocerciasis case study one|Case #1]] | |||
==External Links== | |||
* [http://www.cdc.gov/parasites/onchocerciasis/ CDC Fact Sheet] | |||
{{Helminthiases}} | {{Helminthiases}} | ||
{{Eye pathology}} | {{Eye pathology}} | ||
[[Category:Tropical disease]] | [[Category:Tropical disease]] | ||
[[Category:Parasitic diseases]] | [[Category:Parasitic diseases]] | ||
[[Category:Neglected diseases]] | [[Category:Neglected diseases]] | ||
[[Category:Disease]] | |||
[[de:Onchozerkose]] | [[de:Onchozerkose]] | ||
| Line 90: | Line 76: | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WS}} | {{WS}} | ||
==References== | |||
{{reflist|2}} | |||
Latest revision as of 18:31, 18 September 2017
| Onchocerca volvulus | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
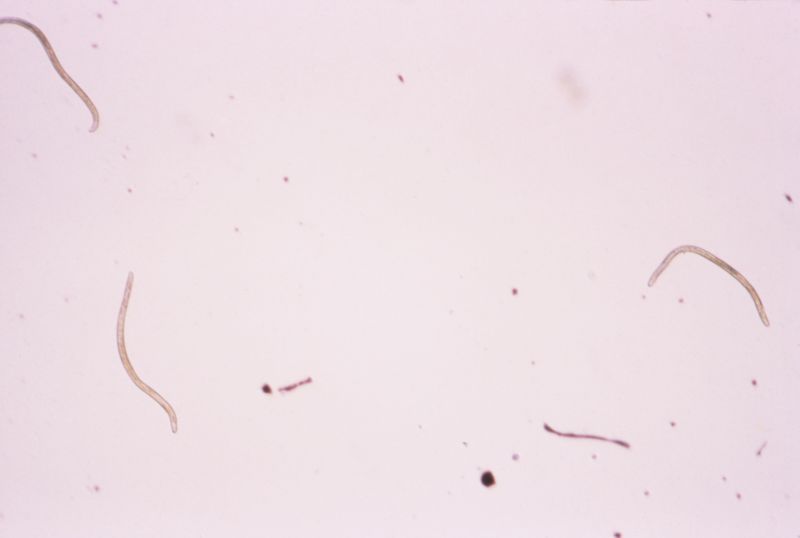 O. volvulus, the causative agent of river blindness.
| ||||||||||||||
| Scientific classification | ||||||||||||||
| ||||||||||||||
| Binomial name | ||||||||||||||
| Onchocerca volvulus Bickel 1982 |
|
Onchocerciasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Onchocerciasis On the Web |
|
American Roentgen Ray Society Images of Onchocerciasis |
For patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Kalsang Dolma, M.B.B.S.[2]
Synonyms and keywords: Onchocercosis; river blindness; Robles disease; onchocerca volvulus infection
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Onchocerciasis from other Diseases
Epidemiology and Demographics
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory Findings | Other Diagnostic Studies
Treatment
Medical Therapy | Primary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Antimicrobial therapy
-
- Preferred regimen (1): Doxycycline 150 μg/kg single dose
- Preferred regimen (2): (Doxycycline 100 mg PO qd for 6 weeks OR 200 mg PO qd for 4 weeks) THEN Ivermectin after 4-6 months 150 μg/kg single dose
- Preferred regimen (3): Doxycycline 200 mg PO qd for 6 weeks THEN Ivermectin after 4-6 months 150 μg/kg single dose
Case Studies
External Links
de:Onchozerkose
it:Oncocercosi
fi:Jokisokeus
References
- ↑ Taylor MJ, Hoerauf A, Bockarie M (2010). "Lymphatic filariasis and onchocerciasis". Lancet. 376 (9747): 1175–85. doi:10.1016/S0140-6736(10)60586-7. PMID 20739055.
- ↑ Knopp S, Steinmann P, Hatz C, Keiser J, Utzinger J (2012). "Nematode infections: filariases". Infect Dis Clin North Am. 26 (2): 359–81. doi:10.1016/j.idc.2012.02.005. PMID 22632644.