Membranous glomerulonephritis: Difference between revisions
m (Robot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
'''For patient information page, click [[{{PAGENAME}} (patient information)|here]] | '''For patient information page, click [[{{PAGENAME}} (patient information)|here]] | ||
{{Infobox_Disease | | {{Infobox_Disease | | ||
Name = {{PAGENAME}} | | Name = {{PAGENAME}} | | ||
| Line 13: | Line 13: | ||
MeshID = D015433 | | MeshID = D015433 | | ||
}} | }} | ||
{{ | {{Membranous glomerulonephritis}} | ||
{{CMG}} | {{CMG}} | ||
Revision as of 20:00, 27 September 2012
For patient information page, click here
| Membranous glomerulonephritis | |
 | |
|---|---|
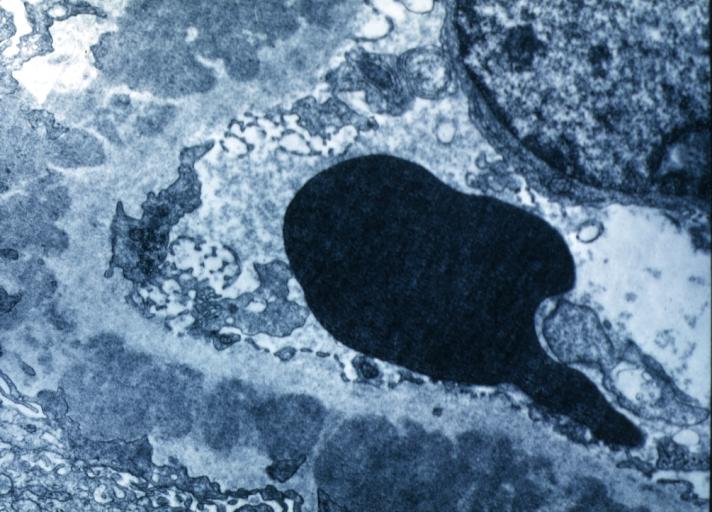
| Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | N03.2 |
| ICD-9 | 583.1 |
| DiseasesDB | 7970 |
| MeSH | D015433 |
|
Membranous glomerulonephritis Microchapters |
|
Differentiating Membranous glomerulonephritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Membranous glomerulonephritis On the Web |
|
American Roentgen Ray Society Images of Membranous glomerulonephritis |
|
Directions to Hospitals Treating Membranous glomerulonephritis |
|
Risk calculators and risk factors for Membranous glomerulonephritis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Membranous glomerulonephritis (MGN), also known as membranous nephropathy, is a slowly progressive disease of the kidney affecting mostly patients between ages of 30 and 50 years. 85% of MGN cases are classified as primary membranous glomerulonephritis -- that is to say, the cause of the disease is idiopathic (unknown). This can also be referred to as idiopathic membranous nephropathy. The remainder is secondary due to :
- autoimmune conditions (e.g., systemic lupus erythematosus)
- infections (e.g., syphilis, malaria, hepatitis B)
- drugs (e.g., captopril, NSAIDs)
- inorganic salts
- malignant tumors (in particular, carcinoma of the lung and colon, and melanoma)
The word membranous refers to the glomerular basement membrane of the kidney; glomerulonephritis means "a kidney disease affecting the capillaries of the glomeruli"; nephropathy is a generic term that just refers to any disease of the kidney.
Pathogenesis
MGN is caused by circulating immune complex. Current research indicates that the majority of the immune complexes are formed via binding of antibodies to antigens in situ to the glomerular basement membrane. The said antigens may be endogenous to (from) the basement membrane, or "planted" from systemic circulation.
The immune complex serves as an activator that triggers a response from the C5b - C9 complements, which form a membrane attack complex (MAC) on the glomerular epithelial cells. This, in turn, stimulates release of proteases and oxidants by the mesangial and epithelial cells, damaging the capillary walls and causing them to become "leaky". In addition, the epithelial cells also seem to secrete an unknown mediator that reduces nephrin synthesis and distribution.
Morphology
The defining point of MGN is the presence of subepithelial immunoglobulin-containing deposits along the glomerular basement membrane (GBM). By light microscopy, the basement membrane is observed to be diffusively thickened. Using Jones' stain, the GBM appears to have a "spiked" or "holey" appearance. On electron microscopy, subepithelial deposits that nestle against the glomerular basement membrane seems to be the cause of the thickening. Also, the podocytes lose their foot processes.
As the disease progresses, the deposits will eventually be cleared, leaving cavities in the basement membrane. These cavities will later be filled with basement membrane-like material, and if the disease continues even further, the glomeruli will become sclerosed and finally hyalinized.
Immunoflourescence microscopy will reveal typical granular deposition of immunoglobulins and complement along the basement membrane.
Clinical Presentation
Some patients may present as nephrotic syndrome with proteinuria, edema with or without renal failure. Others may be asymptomatic and may be picked up on screening or urinalysis as having proteinuria. A definitive diagnosis of membranous nephropathy requires a kidney biopsy.
Treatment
Treatment of secondary membranous nephropathy is guided by the treatment of the original disease. For treatment of idiopathic membranous nephropathy, the treatment options include immunosuppressive drugs and non-specific anti-proteinuric measures.
Immunosuppressive therapy
- Corticosteroids: They have been tried with mixed results, with one study showing prevention of progression to renal failure without improvement in proteinuria.
- Chlorambucil
- Cyclosporine
- Tacrolimus
- Cyclophosphamide
- Mycophenolate mofetil
Perhaps the most difficult aspect of membranous glomerulonpehritis is deciding which patients to treat with immunosuppressive therapy as opposed to simple "background" or anti-proteinuric therapies. A large part of this difficulty is due to a lack of ability to predict which patient will progress to end-stage renal disease, or renal disease severe enough to require dialysis. Because the above medications carry risk, treatment should not be initiated without careful consideration as to risk/benefit profile. Of note, corticosteroids (typically Prednisone) alone are of little benefit. They should be combined with one of the other 5 medications, each of which, along with prednisone, has shown some benefit in slowing down progression of membranous nephropathy. It must be kept in mind, however, that each of the 5 medications also carry their own risks, on top of prednisone.
Natural History
About a third of patients have spontaneous remission, another third progress to require dialysis and the last third continue to have proteinuria, without progression of renal failure.
Pathological Findings
-
Membranous Glomerulonephritis: Electron micrography. An excellent example to show thickened basement membrane and immune complexes.
-
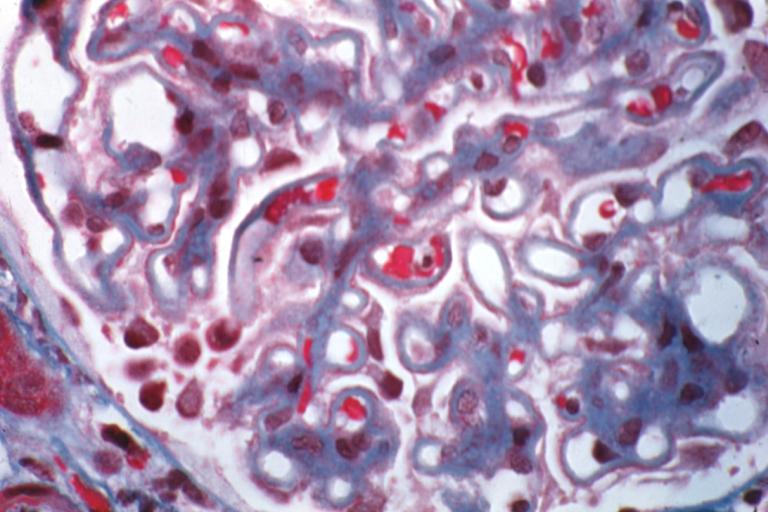
Membranous Glomerulonephritis: Micro trichrome high mag excellent to show thickened capillary basement membranes
-
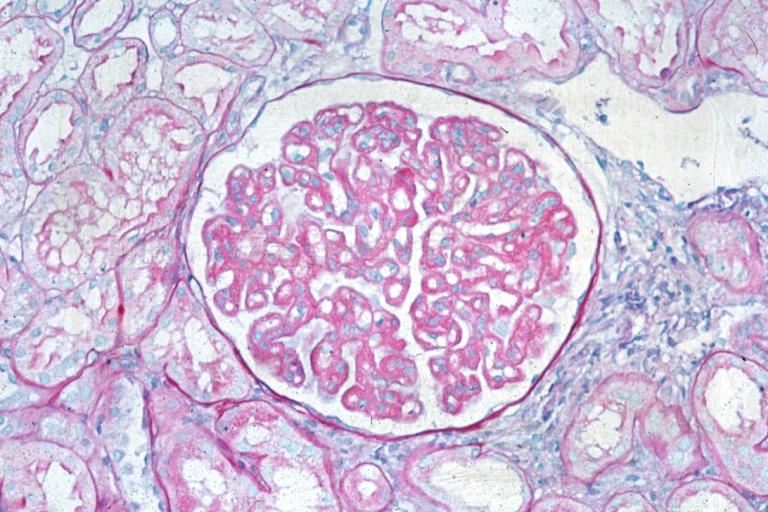
Membranous Glomerulonephritis: Micro PAS high mag excellent example of this lesion
-
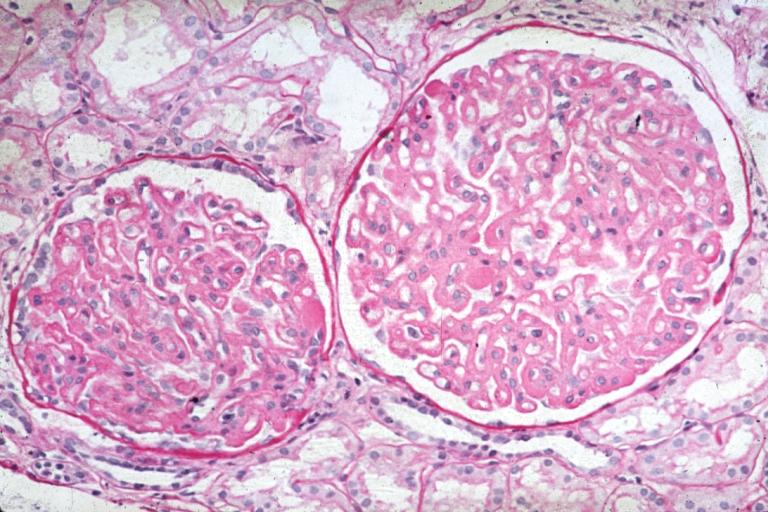
Membranous Glomerulonephritis: Micro PAS med mag
References