Kallman syndrome: Difference between revisions
| Line 16: | Line 16: | ||
{{CMG}} | {{CMG}} | ||
==Treatment== | ==Treatment== | ||
Revision as of 16:28, 19 September 2012
| Kallman syndrome | |
 | |
|---|---|
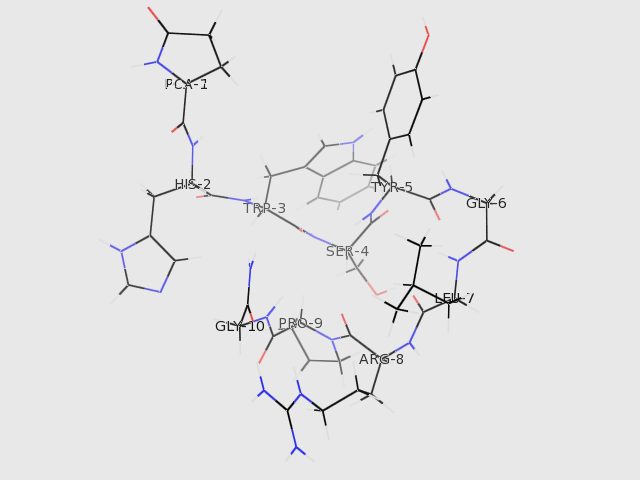
| The structure of GNRH1 (from PDB: 1YY1) | |
| ICD-10 | E23.0 |
| ICD-9 | 253.4 |
| OMIM | 308700 147950 244200 138850 607002 |
| DiseasesDB | 7091 |
| MeSH | D017436 |
|
Kallman syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Kallman syndrome On the Web |
|
American Roentgen Ray Society Images of Kallman syndrome |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Treatment
Treatment is directed at restoring the deficient hormones -- known as hormone therapy (HT). Males are administered human chorionic gonadotropin (hCG) or testosterone. Females are treated with oestrogen and progestins.
To induce fertility in males or females, GnRH (aka LHRH) is administered by an infusion pump, or hCG/hMG/FSH/LH combinations are administered through regular injections. Fertility is only maintained whilst actually being treated with these hormones. Once fertility treatment stops it is necessary to revert to the normal HRT of testosterone for men and oestrogen + progestins for women.
The main health risk, for both men and women, of untreated Kallmann Syndrome is osteoporosis. Therefore, regular bone density scans (every 2 years or so) are advisable, even if being treated with HRT. Additional medication specifically for osteoporosis is necessary in some cases.
Epidemiology
Kallmann syndrome occurs at a rate of 1 in 10,000 male births and 1 in 50,000 female births. It may be inherited as an X-linked condition, an autosomal dominant condition or as an autosomal recessive condition. Statistics are sparse, but it seems that autosomal dominant is the most common form of heredity.
One recent paper [1] quoted an incidence in males of 0.025%, or 1 in 4,000, with the female incidence being 3 to 5 times less.
Even though mutations in the KAL-1 gene on the X chromosome can cause Kallmann syndrome, only 11-14% of patients with Kallmann syndrome have detectable KAL-1 mutations.
Autosomal dominant mutations have been described with the FGFR-1 (8p12) gene, sometimes referred to as the KAL-2 gene. This is thought to cause about 10% of cases. However, the majority of KS cases (70%) would seem to be the result of autosomal dominant genes even though the identity of those genes is not yet known.
Autosomal recessive mutations of the GnRH receptor gene (4q13.2) have also been reported.[1] This defect appears to produce a wider spectrum of physical symptoms than with the other gene defects, and the defect lies in the ability of the pituitary gland to recognize GnRH, rather than the ability of the hypothalamus to produce GnRH. It is debatable as to whether this is in fact Kallmann syndrome since the GnRH receptor development is not related to anosmia.
There may also be no obvious family history of inheritance (sporadic cases). However, it is possible for Kallmann syndrome genes to be passed on to children of a sporadic case.
Psychological Issues
In some cases, the psychological effects of having this condition can outweigh the significance of any physical symptoms.
The social stigma of being left behind by your peer group at a vital stage of physical and emotional development can leave lasting damage to some people. Some people with Kallmann syndrome find it difficult to fit into social groups and may have trouble in forming relationships both on the physical and emotional level. This might be more profound in people who are diagnosed later in life.
Practical Issues
While the lack of sense of smell may not be important when compared to the lack of sexual development, it does give rise to a few situations where care should be taken. These can include:
Personal hygiene.
Gas leaks within the home. Fitting gas detectors within the home is recommended.
Food & drink spoilage. Extra care should be taken with the expiration dates for food and drink.
References
External links
- Updated information web site on Kallmann syndrome
- Information web site on Kallmann's syndrome
- Man, 33, seeks puberty The case of Lawrence Koomson a physician who was treated for the condition as filmed in the documentary. (BBC)
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs
de:Kallmann-Syndrom it:Sindrome di Kallmann he:תסמונת קלמן nl:Syndroom van Kallmann fi:Kallmannin oireyhtymä