Japanese encephalitis
|
Japanese encephalitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Japanese encephalitis On the Web |
|
American Roentgen Ray Society Images of Japanese encephalitis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Epidemiology and Demographics
- Leading cause of viral encephalitis in Asia with 30-50,000 cases reported annually
- Fewer than 1 case/year in U.S. civilians and military personnel traveling to and living in Asia
- Rare outbreaks in U.S. territories in Western Pacific
- Case-fatality rates range from 0.3% to 60%.

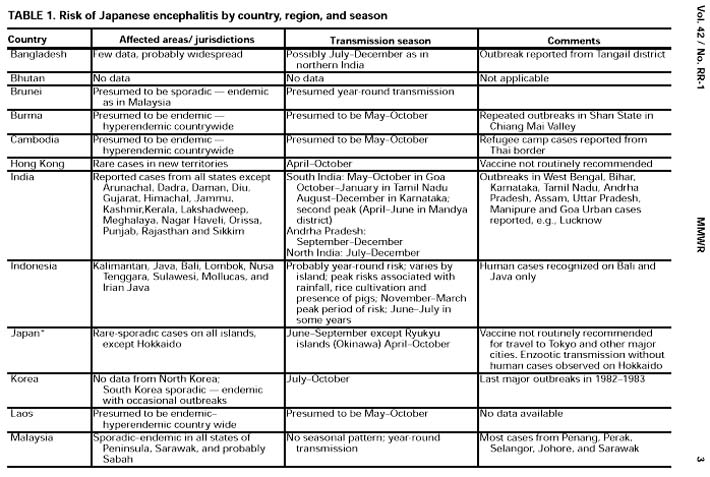
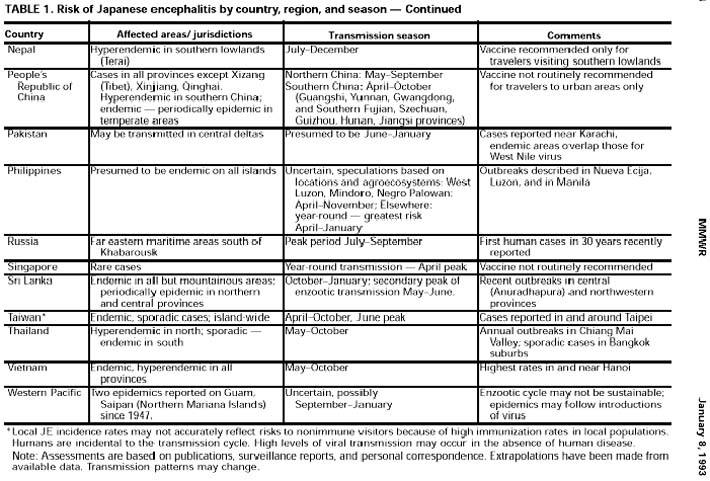
Japanese encephalitis outbreaks are usually circumscribed and do not cover large areas. They usually do not last more than a couple of months, dying out after the majority of the pig amplifying hosts have become infected. Birds are the natural hosts for Japanese encephalitis. Epidemics occur when the virus is brought into the peridomestic environment by mosquito bridge vectors where there are pigs, which serve as amplification hosts, infecting more mosquitoes which then may infect humans. Countries which have had major epidemics in the past, but which have controlled the disease primarily by vaccination, include China, Korea, Japan, Taiwan and Thailand. Other countries that still have periodic epidemics include Viet Nam, Cambodia, Myanmar, India, Nepal, and Malaysia.
Risk Factors
- Residents of rural areas in endemic locations
- Active duty military deployed to endemic areas
- Expatriates in rural areas
- Disease risk extremely low in travelers
Screening
Pathophysiology & Etiology
Etiologic agent:
Japanese encephalitis (JE) virus: flavivirus antigenically related to St. Louis encephalitis virus
Transmission:
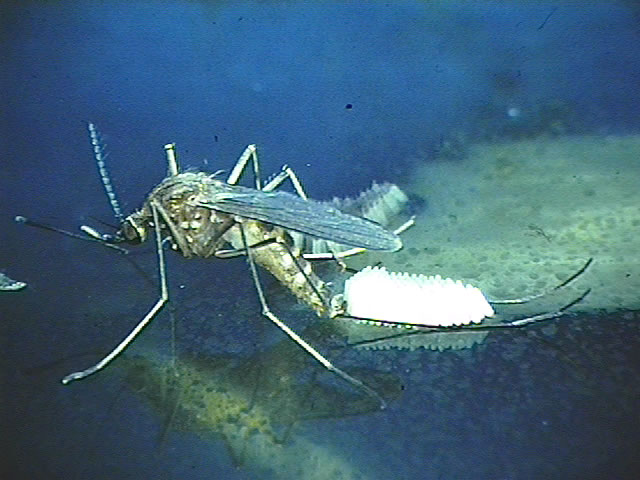
By rice field breeding mosquitoes (primarily Mosquito-borne Culex tritaeniorhynchus group) that become infected with Japanese encephalitis virus (a flavivirus antigenically related to St. Louis encephalitis virus).
Mosquitoes become infected by feeding on domestic pigs and wild birds infected with the Japanese encephalitis virus. Infected mosquitoes then transmit the Japanese encephalitis virus to humans and animals during the feeding process. The Japanese encephalitis virus is amplified in the blood systems of domestic pigs and wild birds.
- Japanese encephalitis virus is NOT transmitted from person-to-person. For example, you cannot get the virus from touching or kissing a person who has the disease, or from a health care worker who has treated someone with the disease.
- Only domestic pigs and wild birds are carriers of the Japanese encephalitis virus.
Diagnosis
History and Symptoms
- Mild infections occur without apparent symptoms other than fever with headache.
- More severe infection is marked by quick onset, headache, high fever, neck stiffness, stupor, disorientation, coma, tremors, occasional convulsions (especially in infants) and spastic (but rarely flaccid) paralysis.
The incubation period for Japanese encephalitis is usually from 5 to 15 days.
Risk Stratification and Prognosis
- Case-fatality ratio: 30%
- Serious neurologic sequela: 30%
Treatment
There is no specific therapy. Intensive supportive therapy is indicated.
Primary Prevention
Who should be vaccinated against Japanese encephalitis:
- U.S. Expatriates: Japanese encephalitis vaccine is recommended for persons who plan to reside in areas where Japanese encephalitis is endemic or epidemic (residence during a transmission season). Risk for acquiring Japanese encephalitis is highly variable within the endemic regions. The incidence of Japanese encephalitis in the location of intended residence, the conditions of housing, nature of activities, and the possibility of unexpected travel to high-risk areas are factors that should be considered in the decision to seek vaccination.
- Travelers: Japanese encephalitis vaccine is NOT recommended for all travelers to Asia. In general, vaccine should be offered to persons spending a month or longer in endemic areas during the trans-mission season, especially if travel will include rural areas. Under specific circumstances, vaccine should be considered for persons spending <30 days in endemic areas, e.g., travelers to areas experiencing epidemic transmission and persons whose activities, such as extensive outdoor activities in rural areas, place them at high risk for exposure. In all instances, travelers should be advised to take personal precautions; e.g., to reduce exposure to mosquito bites. The decision to use Japanese encephalitis vaccine should balance the risks for exposure to the virus and for developing illness, the availability and acceptability of repellents and other alternative protective measures, and the side effects of vaccination. Risk assessments should be interpreted cautiously since risk can vary within areas and from year to year and available data are incomplete. Estimates suggest that risk of Japanese encephalitis in highly endemic areas during the transmission season can reach 1 per 5,000 per month of exposure; risk for most short-term travelers may be 1 per million. Although Japanese encephalitis vaccine is reactogenic, rates of serious allergic reactions (generalized urticaria or angioedema) are low (1 to 104 per 10,000). Advanced age may be a risk factor for developing symptomatic illness after infection. Japanese encephalitis acquired during pregnancy carries the potential for intrauterine infection and fetal death. These special factors should be considered when advising elderly persons and pregnant women who plan visits to areas where Japanese encephalitis is endemic.
Secondary Prevention
Cost-Effectiveness of Therapy
- Domestic: < $1 million/year - largely cost of immunizing travelers and military personnel
- International: no data, probably tens of millions of dollars
References
- http://www.cdc.gov/ncidod/dvbid/jencephalitis/index.htm
- http://www.cdc.gov/ncidod/dvbid/jencephalitis/facts.htm
- http://www.cdc.gov/ncidod/dvbid/jencephalitis/qa.htm
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D.