Intussusception pathophysiology: Difference between revisions
Sargun Walia (talk | contribs) |
Sargun Walia (talk | contribs) |
||
| Line 53: | Line 53: | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
The exact pathogenesis of intussusception is not fully understood. | * The exact pathogenesis of intussusception is not fully understood. | ||
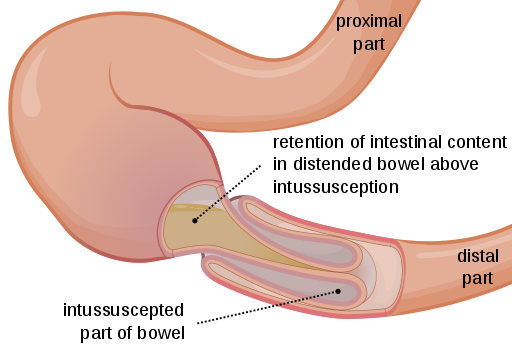
Under normal conditions, a balance between the longitudinal and radial forces maintains the normal structure of intestine. Intussusception occurs if there is an imbalance between the longitudinal forces. This imbalance leads to a segment of intestine to invaginate into another segment and cause entero-enteral intussusception. The proximal portion is called intussusceptum and the | * Under normal conditions, a balance between the longitudinal and radial forces maintains the normal structure of intestine. | ||
* Intussusception occurs if there is an imbalance between the longitudinal forces. | |||
* This imbalance leads to a segment of intestine to invaginate into another segment and cause entero-enteral intussusception. | |||
* The proximal portion is called "intussusceptum" and the distal portion is called "intussuscipien". | |||
* If this telescoping of the intestine continues it can extend till distal colon or sigmoid colon or even through the anus. | |||
[[File:512px-Intussusception EN.svg.png|center|500px|frame|'''Intussusception'''(Source: By Olek Remesz (wiki-pl: Orem, commons: Orem) (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons)]] | [[File:512px-Intussusception EN.svg.png|center|500px|frame|'''Intussusception'''(Source: By Olek Remesz (wiki-pl: Orem, commons: Orem) (Own work) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons)]] | ||
| Line 82: | Line 86: | ||
* '''Idiopathic''':- It is the most common cause of intussusception in children and accounts for about 75% of all cases.Any specific disease trigger point or lead point cannot be recognized. It can be further divided among various causes: | * '''Idiopathic''':- It is the most common cause of intussusception in children and accounts for about 75% of all cases.Any specific disease trigger point or lead point cannot be recognized. It can be further divided among various causes: | ||
** '''Viral Cause''' | ** '''Viral Cause''' | ||
*** Seasonal viral gastro-enteritis.<ref name="pmid17766518">{{cite journal |vauthors=Buettcher M, Baer G, Bonhoeffer J, Schaad UB, Heininger U |title=Three-year surveillance of intussusception in children in Switzerland |journal=Pediatrics |volume=120 |issue=3 |pages=473–80 |year=2007 |pmid=17766518 |doi=10.1542/peds.2007-0035 |url=}}</ref> | *** '''Seasonal viral gastro-enteritis'''.<ref name="pmid17766518">{{cite journal |vauthors=Buettcher M, Baer G, Bonhoeffer J, Schaad UB, Heininger U |title=Three-year surveillance of intussusception in children in Switzerland |journal=Pediatrics |volume=120 |issue=3 |pages=473–80 |year=2007 |pmid=17766518 |doi=10.1542/peds.2007-0035 |url=}}</ref> | ||
*** Rotavirus Vaccine:- Intussusception is known to be caused by certain types of Rotavirus Vaccines. An earlier iteration of the vaccine known as the Rotashield was taken out of the market because it was associated with an increased number of cases of intussusception. If there occurs any case of intussusception after vaccination with rotavirus vaccine, then it should be reported to the Vaccine Adverse Event Reporting System (VAERS) by the providers.<ref name="pmid26209838">{{cite journal |vauthors=Shimabukuro TT, Nguyen M, Martin D, DeStefano F |title=Safety monitoring in the Vaccine Adverse Event Reporting System (VAERS) |journal=Vaccine |volume=33 |issue=36 |pages=4398–405 |year=2015 |pmid=26209838 |pmc=4632204 |doi=10.1016/j.vaccine.2015.07.035 |url=}}</ref> | *** '''Rotavirus Vaccine''':- Intussusception is known to be caused by certain types of Rotavirus Vaccines. An earlier iteration of the vaccine known as the Rotashield was taken out of the market because it was associated with an increased number of cases of intussusception. If there occurs any case of intussusception after vaccination with rotavirus vaccine, then it should be reported to the Vaccine Adverse Event Reporting System (VAERS) by the providers.<ref name="pmid26209838">{{cite journal |vauthors=Shimabukuro TT, Nguyen M, Martin D, DeStefano F |title=Safety monitoring in the Vaccine Adverse Event Reporting System (VAERS) |journal=Vaccine |volume=33 |issue=36 |pages=4398–405 |year=2015 |pmid=26209838 |pmc=4632204 |doi=10.1016/j.vaccine.2015.07.035 |url=}}</ref> | ||
*** Adenovirus:- There is a strong association with adenovirus infection. A case control study conducted in Vietnam and Australia shows that Specie C of adenovirus is a strong predictor of intussusception in children.<ref name="pmid17011313">{{cite journal |vauthors=Bines JE, Liem NT, Justice FA, Son TN, Kirkwood CD, de Campo M, Barnett P, Bishop RF, Robins-Browne R, Carlin JB |title=Risk factors for intussusception in infants in Vietnam and Australia: adenovirus implicated, but not rotavirus |journal=J. Pediatr. |volume=149 |issue=4 |pages=452–60 |year=2006 |pmid=17011313 |doi=10.1016/j.jpeds.2006.04.010 |url=}}</ref> | *** '''Adenovirus''':- There is a strong association with adenovirus infection. A case control study conducted in Vietnam and Australia shows that Specie C of adenovirus is a strong predictor of intussusception in children.<ref name="pmid17011313">{{cite journal |vauthors=Bines JE, Liem NT, Justice FA, Son TN, Kirkwood CD, de Campo M, Barnett P, Bishop RF, Robins-Browne R, Carlin JB |title=Risk factors for intussusception in infants in Vietnam and Australia: adenovirus implicated, but not rotavirus |journal=J. Pediatr. |volume=149 |issue=4 |pages=452–60 |year=2006 |pmid=17011313 |doi=10.1016/j.jpeds.2006.04.010 |url=}}</ref> | ||
***Viral infections stimulate the lymphatic tissue in the intestine and lead to the hypertrophy of the payers patches in the terminal ileum and cause the formation of a lead point. This may act as an obstruction and lead to intussusception. Due to this association with hyperplasia, use of glucocorticoids may be used to prevent recurrence but it is not encouraged. | ***Viral infections stimulate the lymphatic tissue in the intestine and lead to the hypertrophy of the payers patches in the terminal ileum and cause the formation of a lead point. This may act as an obstruction and lead to intussusception. Due to this association with hyperplasia, use of glucocorticoids may be used to prevent recurrence but it is not encouraged. | ||
** '''Bacterial enteritis''':- A retrospective cohort study done in children aged 0-5 years shows a strong association between bacterial enteritis and intussusception.<ref name="pmid20138300">{{cite journal |vauthors=Nylund CM, Denson LA, Noel JM |title=Bacterial enteritis as a risk factor for childhood intussusception: a retrospective cohort study |journal=J. Pediatr. |volume=156 |issue=5 |pages=761–5 |year=2010 |pmid=20138300 |doi=10.1016/j.jpeds.2009.11.026 |url=}}</ref> There is an increased risk of development of intussusception with Shigella, Salmonella, E coli and Campylobacter infections. | ** '''Bacterial enteritis''':- A retrospective cohort study done in children aged 0-5 years shows a strong association between bacterial enteritis and intussusception.<ref name="pmid20138300">{{cite journal |vauthors=Nylund CM, Denson LA, Noel JM |title=Bacterial enteritis as a risk factor for childhood intussusception: a retrospective cohort study |journal=J. Pediatr. |volume=156 |issue=5 |pages=761–5 |year=2010 |pmid=20138300 |doi=10.1016/j.jpeds.2009.11.026 |url=}}</ref> There is an increased risk of development of intussusception with Shigella, Salmonella, E coli and Campylobacter infections. | ||
* '''Lead Point''':- Lead point can be defined as any lesion that gets trapped in the intestine by peristaltic forces, which then gets dragged into the distal segment of the intestine leading to the formation of intussusception. Lead point accounts for 25% cases of iintussusception in childhood and almost 95% of cases of intussusception seen in adults. Lead point can be caused due to various pathological reasons which are as follows:- | * '''Lead Point''':- Lead point can be defined as any lesion that gets trapped in the intestine by peristaltic forces, which then gets dragged into the distal segment of the intestine leading to the formation of intussusception. Lead point accounts for 25% cases of iintussusception in childhood and almost 95% of cases of intussusception seen in adults. Lead point can be caused due to various pathological reasons which are as follows:- | ||
** Henoch-Schönlein purpura (HSP):- It is is an IgA mediated inflammatory disorder which causes inflammation and bleeding of the small blood vessels in skin, intestine, joints, and kidneys. HSP is most commonly seen in children less than 7 years of age. In HSP, hematoma formation in the small intestine may act as a lead point. Intussusception mostly occur once the abdominal pain subsides.<ref name="pmid18351468">{{cite journal |vauthors=Ebert EC |title=Gastrointestinal manifestations of Henoch-Schonlein Purpura |journal=Dig. Dis. Sci. |volume=53 |issue=8 |pages=2011–9 |year=2008 |pmid=18351468 |doi=10.1007/s10620-007-0147-0 |url=}}</ref><ref name="pmid1955678">{{cite journal |vauthors=Little KJ, Danzl DF |title=Intussusception associated with Henoch-Schonlein purpura |journal=J Emerg Med |volume=9 Suppl 1 |issue= |pages=29–32 |year=1991 |pmid=1955678 |doi= |url=}}</ref>. Intussusception in HSP mostly originates in the ileum or jejunum , and more than one-half of cases are confined to the small bowel. In contrast to idiopathic intussusception, where the majority (80%-90%) are ileo-colic. | ** '''Henoch-Schönlein purpura''' (HSP):- It is is an IgA mediated inflammatory disorder which causes inflammation and bleeding of the small blood vessels in skin, intestine, joints, and kidneys. HSP is most commonly seen in children less than 7 years of age. In HSP, hematoma formation in the small intestine may act as a lead point. Intussusception mostly occur once the abdominal pain subsides.<ref name="pmid18351468">{{cite journal |vauthors=Ebert EC |title=Gastrointestinal manifestations of Henoch-Schonlein Purpura |journal=Dig. Dis. Sci. |volume=53 |issue=8 |pages=2011–9 |year=2008 |pmid=18351468 |doi=10.1007/s10620-007-0147-0 |url=}}</ref><ref name="pmid1955678">{{cite journal |vauthors=Little KJ, Danzl DF |title=Intussusception associated with Henoch-Schonlein purpura |journal=J Emerg Med |volume=9 Suppl 1 |issue= |pages=29–32 |year=1991 |pmid=1955678 |doi= |url=}}</ref>. Intussusception in HSP mostly originates in the ileum or jejunum , and more than one-half of cases are confined to the small bowel. In contrast to idiopathic intussusception, where the majority (80%-90%) are ileo-colic. | ||
** Cystic Fibrosis:- Intussusception is one of the complication of cystic fibrosis. In this thick inspissated/impacted stool acts as a lead point.<ref name="pmid2053797">{{cite journal |vauthors=Holmes M, Murphy V, Taylor M, Denham B |title=Intussusception in cystic fibrosis |journal=Arch. Dis. Child. |volume=66 |issue=6 |pages=726–7 |year=1991 |pmid=2053797 |pmc=1793149 |doi= |url=}}</ref><ref name="pmid2657054">{{cite journal |vauthors=Webb AK, Khan A |title=Chronic intussusception in a young adult with cystic fibrosis |journal=J R Soc Med |volume=82 Suppl 16 |issue= |pages=47–8 |year=1989 |pmid=2657054 |pmc=1291920 |doi= |url=}}</ref><ref name="pmid4045671">{{cite journal |vauthors=Gross K, Desanto A, Grosfeld JL, West KW, Eigen H |title=Intra-abdominal complications of cystic fibrosis |journal=J. Pediatr. Surg. |volume=20 |issue=4 |pages=431–5 |year=1985 |pmid=4045671 |doi= |url=}}</ref> | ** '''Cystic Fibrosis''':- Intussusception is one of the complication of cystic fibrosis. In this thick inspissated/impacted stool acts as a lead point.<ref name="pmid2053797">{{cite journal |vauthors=Holmes M, Murphy V, Taylor M, Denham B |title=Intussusception in cystic fibrosis |journal=Arch. Dis. Child. |volume=66 |issue=6 |pages=726–7 |year=1991 |pmid=2053797 |pmc=1793149 |doi= |url=}}</ref><ref name="pmid2657054">{{cite journal |vauthors=Webb AK, Khan A |title=Chronic intussusception in a young adult with cystic fibrosis |journal=J R Soc Med |volume=82 Suppl 16 |issue= |pages=47–8 |year=1989 |pmid=2657054 |pmc=1291920 |doi= |url=}}</ref><ref name="pmid4045671">{{cite journal |vauthors=Gross K, Desanto A, Grosfeld JL, West KW, Eigen H |title=Intra-abdominal complications of cystic fibrosis |journal=J. Pediatr. Surg. |volume=20 |issue=4 |pages=431–5 |year=1985 |pmid=4045671 |doi= |url=}}</ref> | ||
** Celiac disease:- Recent studies show that celiac disease is associated with increased risk of intussusception. Celiac disease may lead to small bowel intussusception by causing dysmotility and excessive secretions in bowel wall or by causing small bowel weakness.<ref name="pmid23679928">{{cite journal |vauthors=Ludvigsson JF, Nordenskjöld A, Murray JA, Olén O |title=A large nationwide population-based case-control study of the association between intussusception and later celiac disease |journal=BMC Gastroenterol |volume=13 |issue= |pages=89 |year=2013 |pmid=23679928 |pmc=3661363 |doi=10.1186/1471-230X-13-89 |url=}}</ref><ref name="pmid11294274">{{cite journal |vauthors=Martinez G, Israel NR, White JJ |title=Celiac disease presenting as entero-enteral intussusception |journal=Pediatr. Surg. Int. |volume=17 |issue=1 |pages=68–70 |year=2001 |pmid=11294274 |doi=10.1007/s003830000395 |url=}}</ref><ref name="pmid10626866">{{cite journal |vauthors=Mushtaq N, Marven S, Walker J, Puntis JW, Rudolf M, Stringer MD |title=Small bowel intussusception in celiac disease |journal=J. Pediatr. Surg. |volume=34 |issue=12 |pages=1833–5 |year=1999 |pmid=10626866 |doi= |url=}}</ref> | ** '''Celiac disease''':- Recent studies show that celiac disease is associated with increased risk of intussusception. Celiac disease may lead to small bowel intussusception by causing dysmotility and excessive secretions in bowel wall or by causing small bowel weakness.<ref name="pmid23679928">{{cite journal |vauthors=Ludvigsson JF, Nordenskjöld A, Murray JA, Olén O |title=A large nationwide population-based case-control study of the association between intussusception and later celiac disease |journal=BMC Gastroenterol |volume=13 |issue= |pages=89 |year=2013 |pmid=23679928 |pmc=3661363 |doi=10.1186/1471-230X-13-89 |url=}}</ref><ref name="pmid11294274">{{cite journal |vauthors=Martinez G, Israel NR, White JJ |title=Celiac disease presenting as entero-enteral intussusception |journal=Pediatr. Surg. Int. |volume=17 |issue=1 |pages=68–70 |year=2001 |pmid=11294274 |doi=10.1007/s003830000395 |url=}}</ref><ref name="pmid10626866">{{cite journal |vauthors=Mushtaq N, Marven S, Walker J, Puntis JW, Rudolf M, Stringer MD |title=Small bowel intussusception in celiac disease |journal=J. Pediatr. Surg. |volume=34 |issue=12 |pages=1833–5 |year=1999 |pmid=10626866 |doi= |url=}}</ref> | ||
** Crohns disease:- Crohns disease is a chronic granulomatous inflammatory disease which may lead to intussusception due to inflammation and stricture formation in the intestine. <ref name="pmid19529808">{{cite journal |vauthors=López-Tomassetti Fernández EM, Lorenzo Rocha N, Arteaga González I, Carrillo Pallarés A |title=Ileoileal intussusception as initial manifestation of Crohn's disease |journal=Mcgill J Med |volume=9 |issue=1 |pages=34–7 |year=2006 |pmid=19529808 |pmc=2687895 |doi= |url=}}</ref><ref name="pmid1573498">{{cite journal |vauthors=Cohen DM, Conard FU, Treem WR, Hyams JS |title=Jejunojejunal intussusception in Crohn's disease |journal=J. Pediatr. Gastroenterol. Nutr. |volume=14 |issue=1 |pages=101–3 |year=1992 |pmid=1573498 |doi= |url=}}</ref> | ** '''Crohns disease''':- Crohns disease is a chronic granulomatous inflammatory disease which may lead to intussusception due to inflammation and stricture formation in the intestine. <ref name="pmid19529808">{{cite journal |vauthors=López-Tomassetti Fernández EM, Lorenzo Rocha N, Arteaga González I, Carrillo Pallarés A |title=Ileoileal intussusception as initial manifestation of Crohn's disease |journal=Mcgill J Med |volume=9 |issue=1 |pages=34–7 |year=2006 |pmid=19529808 |pmc=2687895 |doi= |url=}}</ref><ref name="pmid1573498">{{cite journal |vauthors=Cohen DM, Conard FU, Treem WR, Hyams JS |title=Jejunojejunal intussusception in Crohn's disease |journal=J. Pediatr. Gastroenterol. Nutr. |volume=14 |issue=1 |pages=101–3 |year=1992 |pmid=1573498 |doi= |url=}}</ref> | ||
** Meckel's diverticulum | ** '''Meckel's diverticulum''' | ||
** Polyp | ** '''Polyp''' | ||
** Duplication Cyst | ** '''Duplication Cyst''' | ||
** Lymphomas | ** '''Lymphomas''' | ||
** Areas of reactive lymphoid hyperplasia | ** Areas of '''reactive lymphoid hyperplasia''' | ||
* '''Post-operative''' :- Small bowel intussusception can occur in postoperative cases. Most commonly seen are jejuno- jejunal or ileo-ileal cases. Most cases are seen after open procedures but can also be seen after non abdominal procedures. It can occur due to uncoordinated peristaltic activity and/or traction from sutures or devices such as a gastrojejunal feeding tube.<ref name="pmid7138069">{{cite journal |vauthors=Ein SH, Ferguson JM |title=Intussusception--the forgotten postoperative obstruction |journal=Arch. Dis. Child. |volume=57 |issue=10 |pages=788–90 |year=1982 |pmid=7138069 |pmc=1627910 |doi= |url=}}</ref><ref name="pmid9880741">{{cite journal |vauthors=Linke F, Eble F, Berger S |title=Postoperative intussusception in childhood |journal=Pediatr. Surg. Int. |volume=14 |issue=3 |pages=175–7 |year=1998 |pmid=9880741 |doi=10.1007/s003830050479 |url=}}</ref><ref name="pmid10843370">{{cite journal |vauthors=Kidd J, Jackson R, Wagner CW, Smith SD |title=Intussusception following the Ladd procedure |journal=Arch Surg |volume=135 |issue=6 |pages=713–5 |year=2000 |pmid=10843370 |doi= |url=}}</ref><ref name="pmid23571141">{{cite journal |vauthors=Klein JD, Turner CG, Kamran SC, Yu AY, Ferrari L, Zurakowski D, Fauza DO |title=Pediatric postoperative intussusception in the minimally invasive surgery era: a 13-year, single center experience |journal=J. Am. Coll. Surg. |volume=216 |issue=6 |pages=1089–93 |year=2013 |pmid=23571141 |doi=10.1016/j.jamcollsurg.2013.01.059 |url=}}</ref> | * '''Post-operative''' :- Small bowel intussusception can occur in postoperative cases. Most commonly seen are jejuno- jejunal or ileo-ileal cases. Most cases are seen after open procedures but can also be seen after non abdominal procedures. It can occur due to uncoordinated peristaltic activity and/or traction from sutures or devices such as a gastrojejunal feeding tube.<ref name="pmid7138069">{{cite journal |vauthors=Ein SH, Ferguson JM |title=Intussusception--the forgotten postoperative obstruction |journal=Arch. Dis. Child. |volume=57 |issue=10 |pages=788–90 |year=1982 |pmid=7138069 |pmc=1627910 |doi= |url=}}</ref><ref name="pmid9880741">{{cite journal |vauthors=Linke F, Eble F, Berger S |title=Postoperative intussusception in childhood |journal=Pediatr. Surg. Int. |volume=14 |issue=3 |pages=175–7 |year=1998 |pmid=9880741 |doi=10.1007/s003830050479 |url=}}</ref><ref name="pmid10843370">{{cite journal |vauthors=Kidd J, Jackson R, Wagner CW, Smith SD |title=Intussusception following the Ladd procedure |journal=Arch Surg |volume=135 |issue=6 |pages=713–5 |year=2000 |pmid=10843370 |doi= |url=}}</ref><ref name="pmid23571141">{{cite journal |vauthors=Klein JD, Turner CG, Kamran SC, Yu AY, Ferrari L, Zurakowski D, Fauza DO |title=Pediatric postoperative intussusception in the minimally invasive surgery era: a 13-year, single center experience |journal=J. Am. Coll. Surg. |volume=216 |issue=6 |pages=1089–93 |year=2013 |pmid=23571141 |doi=10.1016/j.jamcollsurg.2013.01.059 |url=}}</ref> | ||
| Line 103: | Line 107: | ||
*Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3]. | *Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3]. | ||
*The development of [disease name] is the result of multiple genetic mutations. | *The development of [disease name] is the result of multiple genetic mutations. | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 120: | Line 116: | ||
{{WS}} | {{WS}} | ||
{{WH}} | {{WH}} | ||
<references /> | |||
Revision as of 21:51, 27 November 2017
| https://https://www.youtube.com/watch?v=5KvJ3iJnCQk%7C350}} |
|
Intussusception Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Intussusception On the Web |
|
American Roentgen Ray Society Images of Intussusception |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Gross Pathology
Intussusception is caused by part of the intestine being pulled inward into itself. This can block the passage of food through the intestine. If the blood supply is cut off, the segment of intestine pulled inside can die.
The pressure created by the walls of the intestine pressing together causes:
- Decreased blood flow
- Irritation
- Swelling
The intestine can die, and the patient can have significant bleeding. If a hole occurs, infection, shock, and dehydration can take place very rapidly.
Overview
The exact pathogenesis of [disease name] is not fully understood.
OR
It is thought that [disease name] is the result of / is mediated by / is produced by / is caused by either [hypothesis 1], [hypothesis 2], or [hypothesis 3].
OR
[Pathogen name] is usually transmitted via the [transmission route] route to the human host.
OR
Following transmission/ingestion, the [pathogen] uses the [entry site] to invade the [cell name] cell.
OR
[Disease or malignancy name] arises from [cell name]s, which are [cell type] cells that are normally involved in [function of cells].
OR
The progression to [disease name] usually involves the [molecular pathway].
OR
The pathophysiology of [disease/malignancy] depends on the histological subtype.
Pathophysiology
Pathogenesis
- The exact pathogenesis of intussusception is not fully understood.
- Under normal conditions, a balance between the longitudinal and radial forces maintains the normal structure of intestine.
- Intussusception occurs if there is an imbalance between the longitudinal forces.
- This imbalance leads to a segment of intestine to invaginate into another segment and cause entero-enteral intussusception.
- The proximal portion is called "intussusceptum" and the distal portion is called "intussuscipien".
- If this telescoping of the intestine continues it can extend till distal colon or sigmoid colon or even through the anus.
| Types | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ileocolic | Ileo-Ileo-Colic | Jejuno-jejunal | Jejuno-Ileal | Colo-Colic | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
- Intussusception is the most common abdominal emergency in children < 2 years of age.
| Children | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Idiopathic- no lead point | Pathologic- Lead point | ||||||||||||||||||||||||||||||||||||||||||||||||||
- uncommon in adults but when it occurs the most common cause is pathological due to lead point.
If the mesentry invaginates along with the intestine it can lymphatic and venous congestion leading to intestinal edema. If not treated then eventually it leads to ischemia which further can lead to peritonitis or even perforation.
Etiology
- Idiopathic:- It is the most common cause of intussusception in children and accounts for about 75% of all cases.Any specific disease trigger point or lead point cannot be recognized. It can be further divided among various causes:
- Viral Cause
- Seasonal viral gastro-enteritis.[1]
- Rotavirus Vaccine:- Intussusception is known to be caused by certain types of Rotavirus Vaccines. An earlier iteration of the vaccine known as the Rotashield was taken out of the market because it was associated with an increased number of cases of intussusception. If there occurs any case of intussusception after vaccination with rotavirus vaccine, then it should be reported to the Vaccine Adverse Event Reporting System (VAERS) by the providers.[2]
- Adenovirus:- There is a strong association with adenovirus infection. A case control study conducted in Vietnam and Australia shows that Specie C of adenovirus is a strong predictor of intussusception in children.[3]
- Viral infections stimulate the lymphatic tissue in the intestine and lead to the hypertrophy of the payers patches in the terminal ileum and cause the formation of a lead point. This may act as an obstruction and lead to intussusception. Due to this association with hyperplasia, use of glucocorticoids may be used to prevent recurrence but it is not encouraged.
- Bacterial enteritis:- A retrospective cohort study done in children aged 0-5 years shows a strong association between bacterial enteritis and intussusception.[4] There is an increased risk of development of intussusception with Shigella, Salmonella, E coli and Campylobacter infections.
- Viral Cause
- Lead Point:- Lead point can be defined as any lesion that gets trapped in the intestine by peristaltic forces, which then gets dragged into the distal segment of the intestine leading to the formation of intussusception. Lead point accounts for 25% cases of iintussusception in childhood and almost 95% of cases of intussusception seen in adults. Lead point can be caused due to various pathological reasons which are as follows:-
- Henoch-Schönlein purpura (HSP):- It is is an IgA mediated inflammatory disorder which causes inflammation and bleeding of the small blood vessels in skin, intestine, joints, and kidneys. HSP is most commonly seen in children less than 7 years of age. In HSP, hematoma formation in the small intestine may act as a lead point. Intussusception mostly occur once the abdominal pain subsides.[5][6]. Intussusception in HSP mostly originates in the ileum or jejunum , and more than one-half of cases are confined to the small bowel. In contrast to idiopathic intussusception, where the majority (80%-90%) are ileo-colic.
- Cystic Fibrosis:- Intussusception is one of the complication of cystic fibrosis. In this thick inspissated/impacted stool acts as a lead point.[7][8][9]
- Celiac disease:- Recent studies show that celiac disease is associated with increased risk of intussusception. Celiac disease may lead to small bowel intussusception by causing dysmotility and excessive secretions in bowel wall or by causing small bowel weakness.[10][11][12]
- Crohns disease:- Crohns disease is a chronic granulomatous inflammatory disease which may lead to intussusception due to inflammation and stricture formation in the intestine. [13][14]
- Meckel's diverticulum
- Polyp
- Duplication Cyst
- Lymphomas
- Areas of reactive lymphoid hyperplasia
- Post-operative :- Small bowel intussusception can occur in postoperative cases. Most commonly seen are jejuno- jejunal or ileo-ileal cases. Most cases are seen after open procedures but can also be seen after non abdominal procedures. It can occur due to uncoordinated peristaltic activity and/or traction from sutures or devices such as a gastrojejunal feeding tube.[15][16][17][18]
Genetics
- [Disease name] is transmitted in [mode of genetic transmission] pattern.
- Genes involved in the pathogenesis of [disease name] include [gene1], [gene2], and [gene3].
- The development of [disease name] is the result of multiple genetic mutations.
References
- ↑ Buettcher M, Baer G, Bonhoeffer J, Schaad UB, Heininger U (2007). "Three-year surveillance of intussusception in children in Switzerland". Pediatrics. 120 (3): 473–80. doi:10.1542/peds.2007-0035. PMID 17766518.
- ↑ Shimabukuro TT, Nguyen M, Martin D, DeStefano F (2015). "Safety monitoring in the Vaccine Adverse Event Reporting System (VAERS)". Vaccine. 33 (36): 4398–405. doi:10.1016/j.vaccine.2015.07.035. PMC 4632204. PMID 26209838.
- ↑ Bines JE, Liem NT, Justice FA, Son TN, Kirkwood CD, de Campo M, Barnett P, Bishop RF, Robins-Browne R, Carlin JB (2006). "Risk factors for intussusception in infants in Vietnam and Australia: adenovirus implicated, but not rotavirus". J. Pediatr. 149 (4): 452–60. doi:10.1016/j.jpeds.2006.04.010. PMID 17011313.
- ↑ Nylund CM, Denson LA, Noel JM (2010). "Bacterial enteritis as a risk factor for childhood intussusception: a retrospective cohort study". J. Pediatr. 156 (5): 761–5. doi:10.1016/j.jpeds.2009.11.026. PMID 20138300.
- ↑ Ebert EC (2008). "Gastrointestinal manifestations of Henoch-Schonlein Purpura". Dig. Dis. Sci. 53 (8): 2011–9. doi:10.1007/s10620-007-0147-0. PMID 18351468.
- ↑ Little KJ, Danzl DF (1991). "Intussusception associated with Henoch-Schonlein purpura". J Emerg Med. 9 Suppl 1: 29–32. PMID 1955678.
- ↑ Holmes M, Murphy V, Taylor M, Denham B (1991). "Intussusception in cystic fibrosis". Arch. Dis. Child. 66 (6): 726–7. PMC 1793149. PMID 2053797.
- ↑ Webb AK, Khan A (1989). "Chronic intussusception in a young adult with cystic fibrosis". J R Soc Med. 82 Suppl 16: 47–8. PMC 1291920. PMID 2657054.
- ↑ Gross K, Desanto A, Grosfeld JL, West KW, Eigen H (1985). "Intra-abdominal complications of cystic fibrosis". J. Pediatr. Surg. 20 (4): 431–5. PMID 4045671.
- ↑ Ludvigsson JF, Nordenskjöld A, Murray JA, Olén O (2013). "A large nationwide population-based case-control study of the association between intussusception and later celiac disease". BMC Gastroenterol. 13: 89. doi:10.1186/1471-230X-13-89. PMC 3661363. PMID 23679928.
- ↑ Martinez G, Israel NR, White JJ (2001). "Celiac disease presenting as entero-enteral intussusception". Pediatr. Surg. Int. 17 (1): 68–70. doi:10.1007/s003830000395. PMID 11294274.
- ↑ Mushtaq N, Marven S, Walker J, Puntis JW, Rudolf M, Stringer MD (1999). "Small bowel intussusception in celiac disease". J. Pediatr. Surg. 34 (12): 1833–5. PMID 10626866.
- ↑ López-Tomassetti Fernández EM, Lorenzo Rocha N, Arteaga González I, Carrillo Pallarés A (2006). "Ileoileal intussusception as initial manifestation of Crohn's disease". Mcgill J Med. 9 (1): 34–7. PMC 2687895. PMID 19529808.
- ↑ Cohen DM, Conard FU, Treem WR, Hyams JS (1992). "Jejunojejunal intussusception in Crohn's disease". J. Pediatr. Gastroenterol. Nutr. 14 (1): 101–3. PMID 1573498.
- ↑ Ein SH, Ferguson JM (1982). "Intussusception--the forgotten postoperative obstruction". Arch. Dis. Child. 57 (10): 788–90. PMC 1627910. PMID 7138069.
- ↑ Linke F, Eble F, Berger S (1998). "Postoperative intussusception in childhood". Pediatr. Surg. Int. 14 (3): 175–7. doi:10.1007/s003830050479. PMID 9880741.
- ↑ Kidd J, Jackson R, Wagner CW, Smith SD (2000). "Intussusception following the Ladd procedure". Arch Surg. 135 (6): 713–5. PMID 10843370.
- ↑ Klein JD, Turner CG, Kamran SC, Yu AY, Ferrari L, Zurakowski D, Fauza DO (2013). "Pediatric postoperative intussusception in the minimally invasive surgery era: a 13-year, single center experience". J. Am. Coll. Surg. 216 (6): 1089–93. doi:10.1016/j.jamcollsurg.2013.01.059. PMID 23571141.