Intracranial pressure: Difference between revisions
| Line 219: | Line 219: | ||
:* [Differential dx1] | :* [Differential dx1] | ||
:* [Differential dx2] | :* [Differential dx2] | ||
:* [Differential dx3] | :* [Differential dx3] <br /> | ||
: | |||
==Signs and symptoms of increased ICP== | ==Signs and symptoms of increased ICP== | ||
Revision as of 12:50, 18 August 2020
| Intracranial pressure | |
 | |
|---|---|
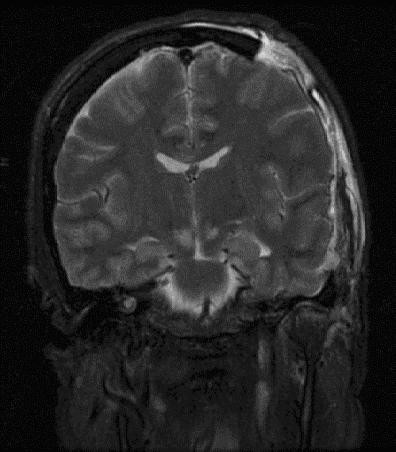
| Severely high ICP can cause herniation. |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Luke Rusowicz-Orazem, B.S.
Overview
Intracranial pressure, (ICP), is the pressure in the cranium and thus in the brain tissue and cerebrospinal fluid (CSF); this pressure is exerted on the brain's intracranial blood circulation vessels. ICP is maintained in a tight normal range dynamically, through the production and absorption of CSF. Because the entire system is contained by bone and strong ligamentous connections, the pressures of the body, such as those caused by straining, exercise, and coughing, do not affect the brain or its environment. ICP is measured in millimeters of mercury (mmHg) and, at rest, is normally 7–15 mmHg for a supine adult, and becomes negative (averaging −10 mmHg) in the vertical position. Changes in ICP are attributed to volume changes in one or more of the constituents contained in the cranium.
Intracranial hypertension, commonly abbreviated IH, is elevation of the pressure in the cranium. ICP is normally 0–10 mm Hg; at 20–25 mm Hg, the upper limit of normal, treatment to reduce ICP is needed.
Historical Perspective[edit | edit source]
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification[edit | edit source]
- [Disease name] may be classified according to [classification method] into [number] subtypes/groups:
- [group1]
- [group2]
- [group3]
- Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3].
Increased ICP
One of the most damaging aspects of brain trauma and other conditions, directly correlated with poor outcome, is an elevated intracranial pressure. ICP is very likely to cause severe harm if it rises beyond 40 mmHg in an adult. Even intracranial pressures between 25 and 30 mm Hg are usually fatal if prolonged, except in children, who can tolerate higher pressures for longer periods. An increase in pressure, most commonly due to head injury leading to intracranial hematoma or cerebral edema can crush brain tissue, shift brain structures, contribute to hydrocephalus, cause the brain to herniate, and restrict blood supply to the brain, leading to an ischemic cascade.
Intracranial Hypertension
Minimal increases in ICP due to compensatory mechanisms is known as stage 1 of intracranial hypertension. When the lesion volume continues to increase beyond the point of compensation, the ICP has no other resource, but to increase. Any change in volume greater than 100–120 mL would mean a drastic increase in ICP. This is stage 2 of intracranial hypertension. Characteristics of stage 2 of intracranial hypertension include compromise of neuronal oxygenation and systemic arteriolar vasoconstriction to increace MAP and CPP. Stage 3 intracranial hypertension is characterised by a sustained increased ICP, with dramatic changes in ICP with small changes in volume. In stage 3, as the ICP approaches the MAP, it becomes more and more difficult to squeeze blood into the intracranial space. The body’s response to a decrease in CPP is to raise blood pressure and dilate blood vessels in the brain. This results in increased cerebral blood volume, which increases ICP, lowering CPP further and causing a vicious cycle. This results in widespread reduction in cerebral flow and perfusion, eventually leading to ischemia and brain infarction. Neurologic changes seen in increased ICP are mostly due to hypoxia and hypercapnea and are as follows: decreased LOC, Cheyne-Stokes respirations, hyperventilation, sluggish dilated pupils and widened pulse pressure.
Pathophysiology
- mass effect such as brain tumor, infarction with edema, contusions, subdural or epidural hematoma, or abscess all tend to deform the adjacent brain.
- generalized brain swelling can occur in ischemic-anoxia states, acute liver failure, hypertensive encephalopathy, pseudotumor cerebri, hypercarbia, and Reye hepatocerebral syndrome. These conditions tend to decrease the cerebral perfusion pressure but with minimal tissue shifts.
- increase in venous pressure can be due to venous sinus thrombosis, heart failure, or obstruction of superior mediastinal or jugular veins.
- obstruction to CSF flow and/or absorption can occur in hydrocephalus (blockage in ventricles or subarachnoid space at base of brain, e.g., by Arnold-Chiari malformation), extensive meningeal disease (e.g., infectious, carcinomatous, granulomatous, or hemorrhagic), or obstruction in cerebral convexities and superior sagittal sinus (decreased absorption).
- increased CSF production can occur in meningitis, subarachnoid hemorrhage, or choroid plexus tumor.
- Drugs Albendazole, Ciprofloxacin
The Monro-Kellie Hypothesis:
Causes
Common Causes
- Aneurysm
- Arnold-chiari malformation
- Behçet's disease
- Brain tumor
- Cerebral edema
- Cerebral venous sinus thrombosis
- Choroid plexus tumor
- Chronic kidney disease
- Colloid cyst of third ventricle
- Contusions
- Crouzon craniofacial dysostosis
- Cushing's syndrome
- Dural arteriovenous fistula
- Encephalitis
- Epidural haemorrhage
- Epidural hematoma
- Erdheim-chester disease
- Excess cerebrospinal fluid
- Head trauma
- Hydrocephalus
- Hypertensive brain hemorrhage
- Hypertensive encephalopathy
- Idiopathic intracranial hypertension
- Insulin like growth factor 1
- Intracranial granuloma
- Intracranial haemorrhage
- Intraventricular hemorrhage
- Meningioma
- Meningitis
- Meningoencephalitis
- Multiple hamartoma syndrome
- Obstruction of superior mediastinal veins
- Obstruction of jugular veins
- Status epilepticus
- Stroke
- Subarachnoid haemorrhage
- Subdural haemorrhage
- Subdural hematoma
- Vasculitis
- Venous sinus thrombosis
Causes by Organ System
Differential Diagnosis of Increased Intracranial Pressure (ICP)
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Signs and symptoms of increased ICP
- Headache
- Nausea
- Vomiting
- Ocular palsies (abducens (CrN VI) palsies)
- Altered level of consciousness
- Papilledema
- Pupillary dilatation
- Cushing's triad ( Elevated systolic blood pressure, a widened pulse pressure, bradycardia, and an abnormal respiratory pattern.
- Cheyne-Stokes respiration
- Hyperventilation (due to injury to brain stem or tegmentum is damaged.[1]
- Bulging of fontanels in infants
Treatment
References
Additional Resources
- Monroe A. Observations on the structure and function of the nervous system, Edinburgh: Creech & Johnson; 1783.
- Kelly G. An account of the appearances observed in the dikssection of two of three individuals presumed to have perished in the storm of the 3rd, and whose bodies were deiscovered in the vicinity of the Leith on the morning of the 4th of November 1821, with some reflections on the pathology of the brain, Trans Med Chir Sci Edinb 1824;1:84–169.
External links
- Gruen P. 2002. "Monro-Kellie Model" Neurosurgery Infonet. USC Neurosurgery. Accessed January 4, 2007.
- National Guideline Clearinghouse. 2005. Guidelines for the management of severe traumatic brain injury. Firstgov. Accessed January 4, 2007.