Idiopathic pulmonary fibrosis pathophysiology: Difference between revisions
| Line 14: | Line 14: | ||
[[Histology|Histologic]] specimens for the diagnosis of IPF must be large enough that the pathologist can comment on the underlying lung architecture. | [[Histology|Histologic]] specimens for the diagnosis of IPF must be large enough that the pathologist can comment on the underlying lung architecture. | ||
Small biopsies, such as those obtained via transbronchial lung biopsy (performed during [[bronchoscopy]]) are generally not sufficient for this purpose. Hence, larger biopsies obtained surgically via a thoracotomy or thoracoscopy are usually necessary. | Small biopsies, such as those obtained via transbronchial lung biopsy (performed during [[bronchoscopy]]) are generally not sufficient for this purpose. Hence, larger biopsies obtained surgically via a thoracotomy or thoracoscopy are usually necessary. | ||
The histological pattern of fibrosis associated with '''IPF''' is referred to as usual interstitial pneumonia (UIP). | The histological pattern of fibrosis associated with '''IPF''' is referred to as usual interstitial pneumonia (UIP). | ||
Revision as of 19:24, 25 September 2012
|
Idiopathic pulmonary fibrosis Microchapters |
|
Differentiating Idiopathic pulmonary fibrosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Idiopathic pulmonary fibrosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Idiopathic pulmonary fibrosis pathophysiology |
|
Directions to Hospitals Treating Idiopathic pulmonary fibrosis |
|
Risk calculators and risk factors for Idiopathic pulmonary fibrosis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pathophysiology
Pulmonary fibrosis has often been called an autoimmune disease. However, it is perhaps better characterized as an abnormal and excessive deposition of fibrotic tissue in the pulmonary interstitium with minimal associated inflammation.[1] Autoantibodies, a hallmark of autoimmune diseases, are found in a minority of patients with truly idiopathic pulmonary fibrosis. Moreover, many autoimmune diseases associated with "pulmonary fibrosis", such as scleroderma, are more frequently associated with a related but more inflammatory disease, nonspecific interstitial pneumonitis.[2] It is associated with smoking[3] and exhibits some dependency on the amount of smoking.[4]
Pathology
- Histology
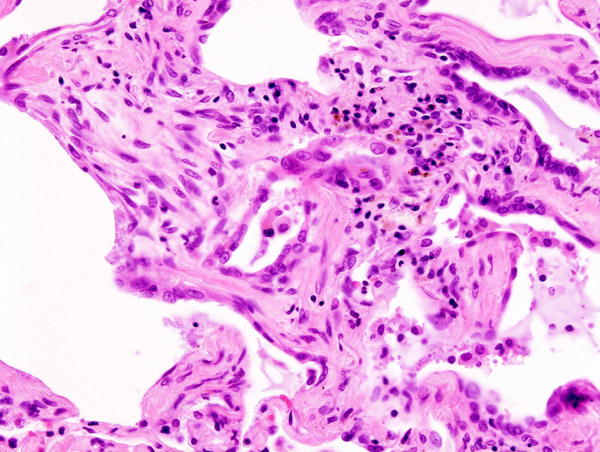
Histologic specimens for the diagnosis of IPF must be large enough that the pathologist can comment on the underlying lung architecture.
Small biopsies, such as those obtained via transbronchial lung biopsy (performed during bronchoscopy) are generally not sufficient for this purpose. Hence, larger biopsies obtained surgically via a thoracotomy or thoracoscopy are usually necessary.
The histological pattern of fibrosis associated with IPF is referred to as usual interstitial pneumonia (UIP).
Although UIP is required for the diagnosis of IPF, it can be seen in other diseases as well.[5]
Key features of UIP include fibroblast foci, a pattern of temporal heterogeneity, dense interstitial fibrosis in a paraseptal and subpleural distribution, and a relatively mild or minor component of interstitial chronic inflammation.[6] To help narrow the differential diagnosis, an absence of significant granulomatous inflammation, microorganisms, eosinophils, and asbestos bodies is required.
References
- ↑ Selman, Moisés (2001). "Idiopathic pulmonary fibrosis: prevailing and evolving hypotheses about its pathogenesis and implications for therapy". Annals of Internal Medicine. 134 (2): 136–51. Unknown parameter
|coauthors=ignored (help) - ↑ King, Jr., Talmadge E. (2005). "Centennial review: clinical advances in the diagnosis and therapy of the interstitial lung diseases". American Journal of Respiratory and Critical Care Medicine. 172 (3): 268–79.
- ↑ Nagai, Sonoko (2000). "Smoking-related interstitial lung diseases". Current Opinion in Pulmonary Medicine. 6 (5): 415–9. PMID 10958232. Unknown parameter
|coauthors=ignored (help) - ↑ Baumgartner, KB (1997). "Cigarette smoking: a risk factor for idiopathic pulmonary fibrosis". American Journal of Respiratory and Critical Care Medicine. 155 (1): 242–248. PMID 9001319. Unknown parameter
|coauthors=ignored (help) - ↑ Kumar, Vinay (2005). Robbins and Cotran's Pathological Basis of Disease (7th ed. ed.). Saunders. p. 729. ISBN 978-0721601878. Unknown parameter
|coauthors=ignored (help) - ↑