Hypoglycemia pathophysiology
|
Hypoglycemia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hypoglycemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Hypoglycemia pathophysiology |
|
Risk calculators and risk factors for Hypoglycemia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Mohammed Abdelwahed M.D[2]
Overview
The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as insulin, glucagon and epinephrine to correct hypoglycemia. Most of these defense mechanisms are hormones that control glycogenolysis and gluconeogenesis.
Pathogenesis
The pathophysiology of hypoglycemia depends on the failure of physiological defense mechanisms and hormones such as insulin, glucagon and epinephrine to correct hypoglycemia. Most of these defense mechanisms are hormones that control glycogenolysis and gluconeogenesis as follows:
The most important and the first mechanism to counter-regulate hypoglycemia is the ability to suppress insulin release. This happens early when blood glucose level is in-between 80–85 mmHg. This cannot occur in patients with absolute beta-cell failure as patients with type 1 diabetes and long-standing type 2 diabetes.[1]High insulin level inhibits hepatic glycogenolysis causing more hypoglycemia.
Hypoglycemia stimulates secretion of glucagon. This happens when blood glucose level falls in-between 65–70 mmHg. Failure to secrete glucagon may be the result of beta-cell failure and high insulin level that inhibits glucagon secretion.[2]
Epinephrine response to hypoglycemia also becomes suppressed in many patients.[3] This happens when blood glucose level falls in-between 65–70mmHg. A suppressed epinephrine response causes defective glucose counter-regulation and hypoglycemia unawareness.[4] This may be due to shifting the glycemic threshold for the sympathoadrenal response to a lower plasma glucose concentration.
The brain is the first organ to be affected by decreased blood glucose level. Impairment of judgment and Seizures may occur resulting in coma.
Gross pathology
On gross pathology insulinomas have a gray to red brown appearance, encapsulated [12]and are usually small and solitary tumors. Although there is a case report of a large(9cm), pedunculated and weighing more than 100g.[5]
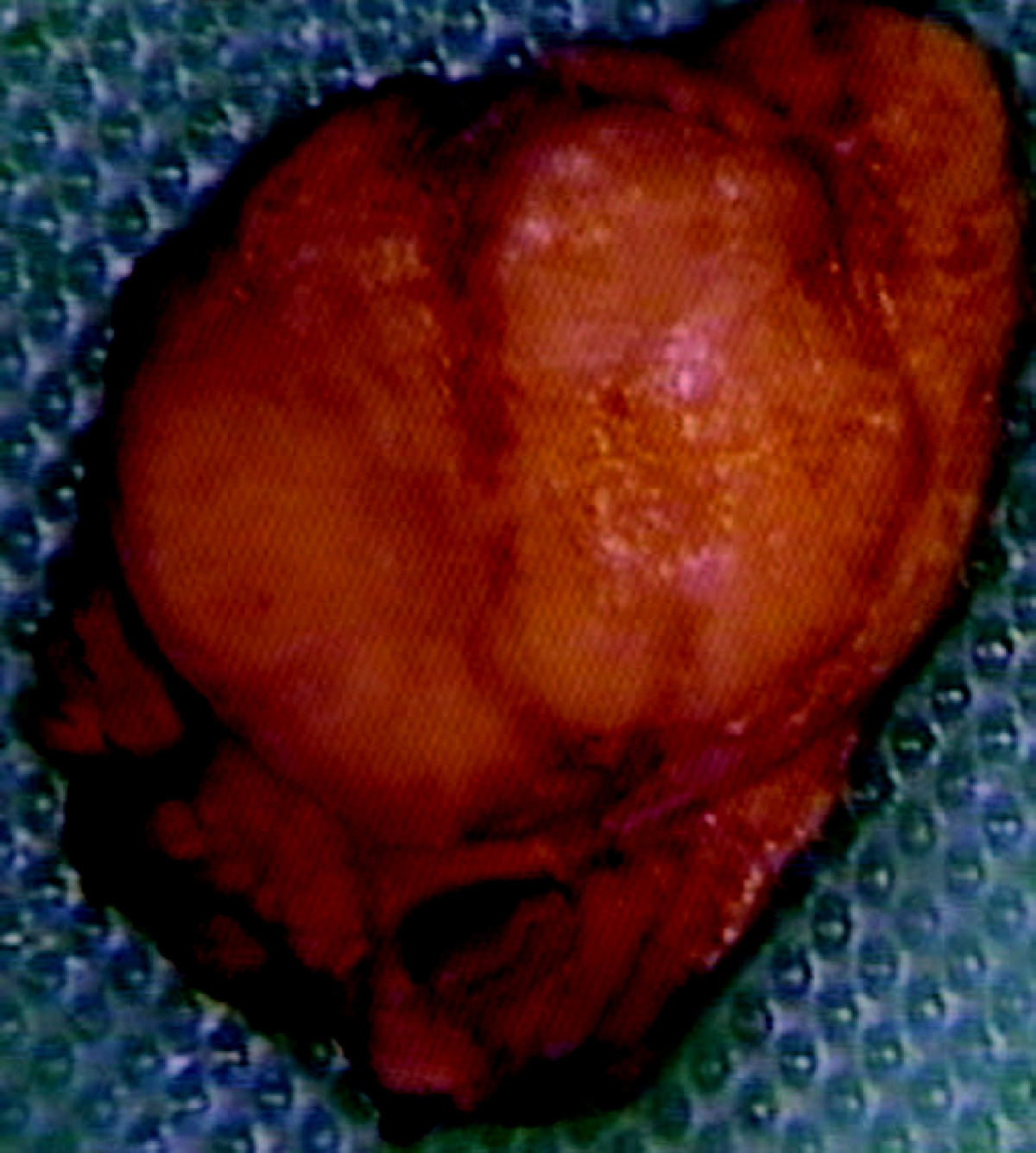
Almost all insulinomas are present throughout the pancreas and extrapancreatic ones causing hypoglycemia are rare(<2%)[14]
Various other findings are noted on gross pathology like[15]
size of the tumor
metastasis to lymph nodes
extrapancreatic involvement
distant metastasis
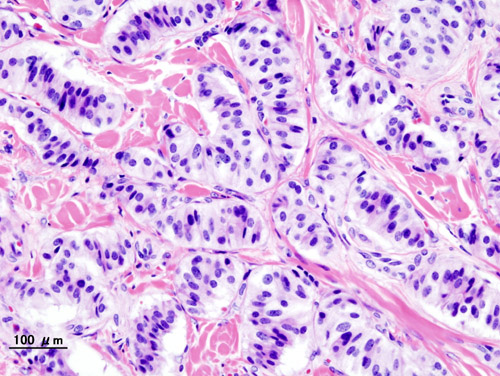
Microscopic pathology
On microscopic histopathological analysis,patterns like trabecular, gyriform, lobular and solid structures particularly with amyloid in fibrovascular stroma are characteristic findings of insulinoma..[6] It is also evaluated for the mitotic index(mitosis per 10 high power field) and immunohistochemistry staining by Chromogranin A, synaptophysin, and Ki-67 index.[7] The structure of tumor cells observed under electron microscopy as: Group A characterised by abundant well-granulated typical B cells with trabecular arrangement and Group B as scarce well -granulated typical B cells and a medullary arrangement.
References
- ↑ Dunning BE, Gerich JE (2007). "The role of alpha-cell dysregulation in fasting and postprandial hyperglycemia in type 2 diabetes and therapeutic implications". Endocr Rev. 28 (3): 253–83. doi:10.1210/er.2006-0026. PMID 17409288.
- ↑ Raju B, Cryer PE (2005). "Loss of the decrement in intraislet insulin plausibly explains loss of the glucagon response to hypoglycemia in insulin-deficient diabetes: documentation of the intraislet insulin hypothesis in humans". Diabetes. 54 (3): 757–64. PMID 15734853.
- ↑ Dagogo-Jack SE, Craft S, Cryer PE (1993). "Hypoglycemia-associated autonomic failure in insulin-dependent diabetes mellitus. Recent antecedent hypoglycemia reduces autonomic responses to, symptoms of, and defense against subsequent hypoglycemia". J Clin Invest. 91 (3): 819–28. doi:10.1172/JCI116302. PMC 288033. PMID 8450063.
- ↑ Geddes J, Schopman JE, Zammitt NN, Frier BM (2008). "Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes". Diabet Med. 25 (4): 501–4. doi:10.1111/j.1464-5491.2008.02413.x. PMID 18387080.
- ↑ Mittendorf EA, Liu YC, McHenry CR (2005). "Giant insulinoma: case report and review of the literature". J Clin Endocrinol Metab. 90 (1): 575–80. doi:10.1210/jc.2004-0825. PMID 15522939.
- ↑ Lloyd, Ricardo (2010). Endocrine pathology : differential diagnosis and molecular advances. New York London: Springer. ISBN 978-1441910684.
- ↑ de Herder, Wouter W.; Niederle, Bruno; Scoazec, Jean-Yves; Pauwels, Stanislas; Klöppel, Günter; Falconi, Massimo; Kwekkeboom, Dik J.; Öberg, Kjel; Eriksson, Barbro; Wiedenmann, Bertram; Rindi, Guido; O’Toole, Dermot; Ferone, Diego (2007). "Well-Differentiated Pancreatic Tumor/Carcinoma: Insulinoma". Neuroendocrinology. 84 (3): 183–188. doi:10.1159/000098010. ISSN 0028-3835.