Hyperparathyroidism x ray: Difference between revisions
(Created page with "__NOTOC__ {{Hyperparathyroidism}} ==Overview== ==X Ray== '''Hand radiographs of a patient with primary hyperparathyroidism''' <gallery> Image: Primary-hyperparathyroidism-00...") |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Hyperparathyroidism}} | {{Hyperparathyroidism}} | ||
{{CMG}}; {{AE}} {{Anmol}} | |||
==Overview== | ==Overview== | ||
X-ray is helpful in diagnosis of hyperparathyroidism. Finding in primary hyperparathyroidism includes subperiosteal [[bone resorption]], endoosteal [[bone resorption]], subchondral [[resorption]], subligamentous [[resorption]], intracortical [[resorption]], [[osteopenia]], [[Brown tumor|brown tumors]], salt and pepper sign in the skull (pepper pot skull), and [[chondrocalcinosis]]. X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. Findings in secondary and tertiary hyperparathyroidism are often associated with the [[osteosclerosis]] of renal [[osteodystrophy]], and the [[osteomalacia]] of [[vitamin D deficiency]] and includes subperiosteal [[bone resorption]],subchondral resorption, subligamentous resorption, severe [[osteopenia]], [[osteosclerosis]], [[brown tumor]], [[amyloid]] deposition, soft tissue and vascular [[calcification]], superior and inferior rib notching, and [[osteonecrosis]]. | |||
==X Ray== | ==X Ray== | ||
===Primary hyperparathyroidism=== | |||
< | {| | ||
|- | |||
| colspan="2" | | |||
Finding in primary hyperparathyroidism includes:<ref name="pmid24614783">{{cite journal |vauthors=Lachungpa T, Sarawagi R, Chakkalakkoombil SV, Jayamohan AE |title=Imaging features of primary hyperparathyroidism |journal=BMJ Case Rep |volume=2014 |issue= |pages= |year=2014 |pmid=24614783 |pmc=3962932 |doi=10.1136/bcr-2013-203521 |url=}}</ref> | |||
*Subperiosteal [[bone resorption]] | |||
**Classically affects the radial aspects of the proximal and middle [[phalanges]] of the index and middle fingers | |||
**Medial aspect of [[tibia]], [[femur]], [[humerus]] | |||
**Phalangeal tuft erosion (acro-osteolysis) | |||
**Lamina dura around teeth (floating teeth) | |||
*Endoosteal [[bone resorption]] | |||
**Widening of [[medullary cavity]] | |||
**Thinning of the inner [[cortex]] | |||
*Subchondral [[resorption]] | |||
**Lateral end of the [[Clavicle|clavicles]] | |||
**[[Pubic symphysis|Symphysis pubis]] | |||
**[[Sacroiliac joint|Sacroiliac joints]] | |||
*Subligamentous [[resorption]] | |||
**[[Ischial tuberosity]] | |||
**Humeral tuberosity | |||
**[[Trochanters]] | |||
**Inferior surface of [[calcaneus]] | |||
**Inferior margin of lateral [[clavicle]] | |||
*Intracortical [[resorption]]: cigar/oval-shaped or tunnel-shaped radiolucency in the cortex | |||
*[[Osteopenia]] | |||
*[[Brown tumor|Brown tumors]] | |||
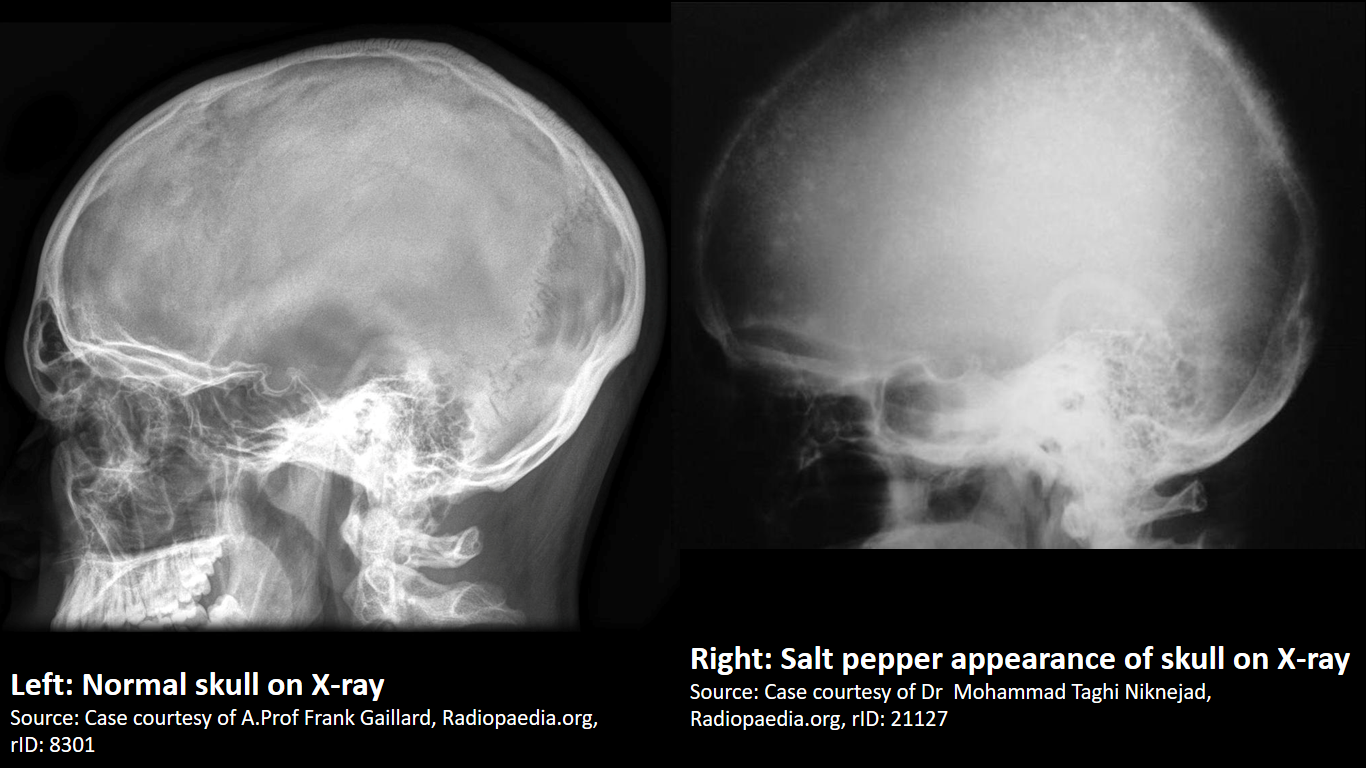
*Salt and pepper sign in the skull (pepper pot skull) | |||
*[[Chondrocalcinosis]] | |||
===Secondary and tertiary hyperparathyroidism=== | |||
X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. <ref name="pmid7785573">{{cite journal |vauthors=Tigges S, Nance EP, Carpenter WA, Erb R |title=Renal osteodystrophy: imaging findings that mimic those of other diseases |journal=AJR Am J Roentgenol |volume=165 |issue=1 |pages=143–8 |year=1995 |pmid=7785573 |doi=10.2214/ajr.165.1.7785573 |url=http://www.ajronline.org/doi/pdf/10.2214/ajr.165.1.7785573}}</ref> Findings in secondary and tertiary hyperparathyroidism are often associated with the [[osteosclerosis]] of renal [[osteodystrophy]], and the [[osteomalacia]] of [[vitamin D deficiency]]: | |||
*Subperiosteal [[bone resorption]] | |||
**Radial aspect of middle [[phalanges]] of index and long fingers are involved. | |||
*Subchondral resorption | |||
**[[Hands]], [[hips]], [[shoulders]], patellofemoral and [[Sacroiliac joint|sacroiliac joints]] are involved. | |||
**Hands are involves in the [[ulnar]] side. | |||
**Distal [[interphalangeal]] and [[metacarpophalangeal]] joints are involved. | |||
**Subchondral [[resorption]] is very severe. It may lead to bony collapse. | |||
*Subligamentous resorption | |||
**Retrocalcaneal bursa and insertion of planter [[aponeurosis]] may be involved. | |||
*Severe [[osteopenia]], may be complicated by pathologic fractures | |||
*[[Osteosclerosis]], e.g. rugger-jersey spine | |||
*[[Brown tumor]] | |||
*[[Amyloid]] deposition | |||
**May be manifested as lytic bone lesion on radiograph | |||
*Soft tissue and vascular [[calcification]] | |||
*Superior and inferior rib notching | |||
*[[Osteonecrosis]] may be often observed in patients in whom [[steroid]] is administered for prevention of [[Kidney transplantation|renal transplant]] rejection. | |||
|- | |||
| | |||
[[image:Subperiosteal bone resorption.gif|thumb|500px|Subperiosteal bone resorption - [https://radiopaedia.org/articles/subperiosteal-bone-resorption Source:Radiopedia]]] | |||
| | |||
[[image:Brown tumor.gif|thumb|500px|Brown tumors - [https://radiopaedia.org/cases/renal-osteodystrophy-and-brown-tumours-1 Source:Case courtesy of A.Prof Frank Gaillard, Radiopedia]]] | |||
|- | |||
| | |||
[[image:Salt-and-pepper-sign-skull compared to normal skull.png|thumb|500px|Normal skull compared to Salt & pepper appearance of skull - [https://radiopaedia.org/cases/21127 Source:Radiopedia]]] | |||
| | |||
[[image:Acro-osteolytis.gif|thumb|500px|Acro-osteolytis, terminal tufts erosion - [https://radiopaedia.org/cases/9738 Source:Case courtesy of Dr Andrew Dixon, Radiopedia]]] | |||
|} | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
| |||
[[Category:Disease]] | |||
[[Category:Medicine]] | |||
[[Category:Endocrinology]] | |||
[[Category:Parathyroid disorders]] | [[Category:Parathyroid disorders]] | ||
[[Category: | [[Category:Up-To-Date]] | ||
[[Category:Radiology]] | |||
Latest revision as of 22:17, 29 July 2020
|
Hyperparathyroidism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hyperparathyroidism x ray On the Web |
|
American Roentgen Ray Society Images of Hyperparathyroidism x ray |
|
Risk calculators and risk factors for Hyperparathyroidism x ray |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Anmol Pitliya, M.B.B.S. M.D.[2]
Overview
X-ray is helpful in diagnosis of hyperparathyroidism. Finding in primary hyperparathyroidism includes subperiosteal bone resorption, endoosteal bone resorption, subchondral resorption, subligamentous resorption, intracortical resorption, osteopenia, brown tumors, salt and pepper sign in the skull (pepper pot skull), and chondrocalcinosis. X-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. Findings in secondary and tertiary hyperparathyroidism are often associated with the osteosclerosis of renal osteodystrophy, and the osteomalacia of vitamin D deficiency and includes subperiosteal bone resorption,subchondral resorption, subligamentous resorption, severe osteopenia, osteosclerosis, brown tumor, amyloid deposition, soft tissue and vascular calcification, superior and inferior rib notching, and osteonecrosis.
X Ray
Primary hyperparathyroidism
|
Finding in primary hyperparathyroidism includes:[1]
Secondary and tertiary hyperparathyroidismX-ray is the preferred imaging for diagnosis of secondary hyperparathyroidism as majority of findings are radiological. [2] Findings in secondary and tertiary hyperparathyroidism are often associated with the osteosclerosis of renal osteodystrophy, and the osteomalacia of vitamin D deficiency:
| |
 |
 |
 |
 |
References
- ↑ Lachungpa T, Sarawagi R, Chakkalakkoombil SV, Jayamohan AE (2014). "Imaging features of primary hyperparathyroidism". BMJ Case Rep. 2014. doi:10.1136/bcr-2013-203521. PMC 3962932. PMID 24614783.
- ↑ Tigges S, Nance EP, Carpenter WA, Erb R (1995). "Renal osteodystrophy: imaging findings that mimic those of other diseases". AJR Am J Roentgenol. 165 (1): 143–8. doi:10.2214/ajr.165.1.7785573. PMID 7785573.