Hereditary elliptocytosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Infobox_Disease | {{Infobox_Disease | ||
| Name = Hereditary elliptocytosis | | Name = Hereditary elliptocytosis | ||
| Line 14: | Line 13: | ||
| MeshID = | | MeshID = | ||
}} | }} | ||
{{ | {{Hereditary elliptocytosis}} | ||
'''For patient information click [[Hereditary elliptocytosis (patient information)|here]]''' | |||
{{CMG}} | {{CMG}} | ||
Revision as of 16:01, 21 September 2012
| Hereditary elliptocytosis | |
 | |
|---|---|
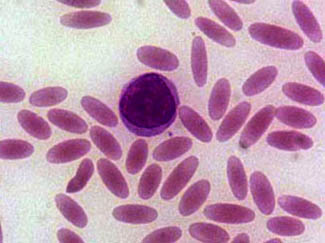
| Blood smear showing elliptocytes | |
| ICD-10 | D58.1 |
| ICD-9 | 282.1 |
| DiseasesDB | 4172 |
| MedlinePlus | 000563 |
|
Hereditary elliptocytosis Microchapters |
|
Differentiating Hereditary elliptocytosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Hereditary elliptocytosis On the Web |
|
American Roentgen Ray Society Images of Hereditary elliptocytosis |
|
Risk calculators and risk factors for Hereditary elliptocytosis |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Hereditary elliptocytosis is a blood disorder in which a large proportion of the sufferer's erythrocytes (i.e. red blood cells) are elliptical rather than bi-concave disc-shaped. It is also known as ovalocytosis. The disorder predisposes to haemolytic anaemia.
Historical perspective
Elliptocytosis was first described in 1904, and was first recognised as a hereditary condition in 1932. More recently it has become clear that there is much genetic heterogeneity amongst sufferers, and the severity of the condition is highly variable.
Aetiology
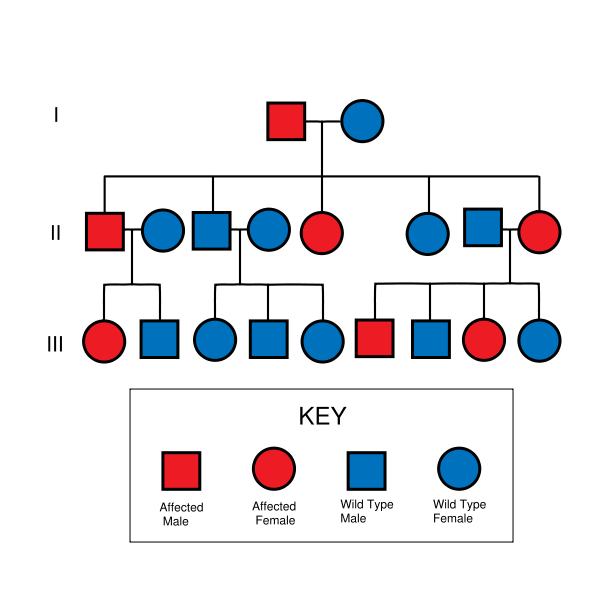
The incidence of hereditary elliptocytosis is hard to determine, as many sufferers of the milder forms of the disorder are asymptomatic and their condition never comes to medical attention. Around 90% of those with this disorder are thought to fall into the asymptomatic population. It is estimated that its incidence is between 3 and 5 per 10,000 in the USA, and that those of African and Mediterranean descent are of higher risk. Some subtypes of hereditary elliptocytosis are significantly more prevalent in regions where malaria is endemic. For example, in equatorial Africa its incidence approaches 160 per 10,000, and in Malayan natives its incidence is over 15% (1500-2000 per 10,000). Being an almost wholly autosomal dominant disorder, there is no predilection towards either sex in hereditary elliptocytosis. The most important exception to this rule of autosomal dominant inheritance is for a subtype of hereditary elliptocytosis called hereditary pyropoikilocytosis (HPP). This condition is autosomal recessive.
There are a number of different subtypes of hereditary elliptocytosis. A clinically significant haemolytic anaemia occurs only in 5-10% of sufferers, with a strong bias towards those with more severe subtypes of the disorder. The following categorisation of the disorder demonstrates its heterogeneity (in approximate order from least severe to most severe)[1]:
- Common hereditary elliptocytosis
- With asymptomatic carrier status - the individual has no symptoms of disease and diagnosis is only able to be made on blood film
- With mild disease - the individual has no symptoms and a mild and compensated haemolytic anaemia
- With sporadic haemolysis - the individual has a predilection towards haemolysis in the presence of particular comorbidities, including infections, and [[Cyanocobalamin|vitamin BTemplate:Ssub]] deficiency
- With neonatal poikilocytosis - during the first year of life only the individual has a symptomatic haemolytic anaemia with poikilocytosis
- With chronic haemolysis - the individual has a moderate to severe symptomatic haemolytic anaemia (this subtype has variable penetrance in some pedigrees)
- With homozygosity or compound heterozygosity - depending on the exact mutations involved, the individual may lie anywhere in the spectrum between having a mild haemolytic anaemia and having a life-threatening haemolytic anaemia with symptoms mimicking those of HPP (see below)
- With pyropoikilocytosis (HPP) - the individual is typically of African descent and has a life-threateningly severe haemolytic anaemia with micropoikilocytosis (small and misshapen erythrocytes) that is compounded by a marked instability of erythrocytes in even mildly elevated temperatures (pyropoikilocytosis is often found in burns victims and is the term is commonly used in reference to such people)
- Spherocytic elliptocytosis (also called hereditary haemolytic ovalocytosis) - the individual is typically of European descent and both elliptocytes and spherocytes are simultaneously present in their blood
- South-east Asian ovalocytosis (SAO) (also called stomatocytic elliptocytosis) - the individual is of South-East Asian descent (typically Malaysian, Indonesian, Melanesian, New Guinean or Filipino, has a mild haemolytic anaemia, and has resistance to malaria
Treatment
The vast majority of those with hereditary elliptocytosis require no treatment whatsoever. They have a mildly increased risk of developing gallstones, which is treated surgically with a cholecystectomy if pain becomes problematic.
Folate helps to reduce the extent of haemolysis in those with significant haemolysis due to hereditary elliptocytosis.
Because the spleen is the bodily organ which breaks down old and worn-out blood cells, those individuals with more severe forms of hereditary elliptocytosis can have a splenomegaly which causes a worsening of the signs and symptoms of their anaemia. These can include:
- Vague, poorly localised abdominal pain
- Fatigue and dyspnoea
- Growth failure
- Leg ulcers
- Gallstones.
Removal of the spleen (splenectomy) is effective in reducing the severity of these complications, but is associated with an increased risk of overwhelming bacterial septicaemia, and is only performed on those with significant complications. Because many neonates with severe elliptocytosis progress to have only a mild disease, and because this age group is particularly susceptible to pneumococcal infections, a splenectomy is only performed on those under 5 years old when it is absolutely necessary.
Because chronic haemolysis increases an individual's risk of gallstones, people with elliptocytosis have an increased risk of suffering from gallstones. This risk is relative to the severity of the disease, and those with symptomatic elliptocytosis should have regular abdominal ultrasounds to monitor the progression of their gall bladder disease.
Prognosis
Those with hereditary elliptocytosis have a good prognosis, only those with very severe disease have a shortened life expectancy.
References
- ↑ Coetzer T, Lawler J, Prchal JT and Palek J (1987). "Molecular Determinants of Clinical Expression of Hereditary Elliptocytosis and Pyropoikilocytosis" (PDF). Blood. 70 (3): 491–588. Retrieved 2006-10-31. Unknown parameter
|month=ignored (help)