Gonorrhea: Difference between revisions
| Line 22: | Line 22: | ||
==[[Gonorrhea history and symptoms|History & Symptoms]]== | ==[[Gonorrhea history and symptoms|History & Symptoms]]== | ||
== Diagnosis == | == Diagnosis == | ||
==[[Gonorrhea laboratory tests|Lab Tests]]== | ==[[Gonorrhea laboratory tests|Lab Tests]]== | ||
Revision as of 14:57, 3 February 2012
Template:DiseaseDisorder infobox
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gonorrhea On the Web |
|
American Roentgen Ray Society Images of Gonorrhea |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Related Key Words and Synonyms: Gonorrhea, Neisseria gonorrhoeae infection, clap, gonococcemia.
Overview
Epidemiology & Demographics
Risk Factors
Pathophysiology
History & Symptoms
Diagnosis
Lab Tests
A quick laboratory test for gonorrhea that can be done in some clinics or doctor's offices is a Gram stain. A Gram stain of a sample from a urethra or a cervix allows the doctor to see the gonorrhea bacterium under a microscope. This test works better for men than for women.
Differentiating Gonorrhea from other Diseases
Treatment
Medical Therapy
Acute Pharmacotherapies
Several antibiotics can successfully cure gonorrhea in adolescents and adults. However, drug-resistant strains of gonorrhea are increasing in many areas of the world, including the United States, and successful treatment of gonorrhea is becoming more difficult. Because many people with gonorrhea also have chlamydia, another sexually transmitted disease, antibiotics for both infections are usually given together. Persons with gonorrhea should be tested for other STDs.
It is important to take all of the medication prescribed to cure gonorrhea. Although medication will stop the infection, it will not repair any permanent damage done by the disease. People who have had gonorrhea and have been treated can get the disease again if they have sexual contact with persons infected with gonorrhea. If a person's symptoms continue even after receiving treatment, he or she should return to a doctor to be reevaluated.
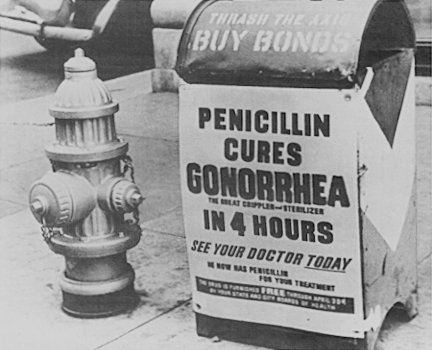
The mainstay of treatment is the appropriate use of antibiotics. While penicillin was the most common antibiotic used to treat gonorrhea up until the 1970s, an increase in antibiotic resistance has led to a decline in its use. Recommendations for first choice treatment of gonorrhea must depend on local information on resistance patterns and it is not possible to make treatment recommendations that are applicable to all parts of the world.
The Centers for Disease Control and Prevention (CDC) released a report on Thursday, April 12, 2007 officially adding gonorrhea to a list of super bugs that are now resistant to common antibiotics according to CDC.
Antibiotics that may be used to treat gonorrhea include:
- Amoxycillin 2 g plus probenecid 1 g orally
- Ampicillin 2 to 3 g plus probenecid 1 g orally
- Azithromycin 2 g orally
- Cefixime 400 mg orally
- Cefotaxime 500 mg by intramuscular injection
- Cefoxitin 2 g by intramuscular injection, plus probenecid 1 g orally
- Cefpodoxime (Vantin) 400 mg orally
- Ceftriaxone (Rocephin) 125 to 250 mg by intramuscular injection
- Ciprofloxacin 500 mg orally
- Levofloxacin 250 mg orally
- Ofloxacin 400 mg orally
- Spectinomycin 2 g by intramuscular injection
These drugs are all given as a single dose.
The level of tetracycline resistance in Neisseria gonorrheae is now so high as to make it completely ineffective in most parts of the world.
The fluoroquinolones (ciprofloxacin, ofloxacin, levofloxacin) cannot be used in pregnancy. It is important to refer all sexual partners to be checked for gonorrhea to prevent spread of the disease and to prevent the patient from becoming re-infected with gonorrhea. Patients should also be offered screening for other sexually transmitted infections. In areas where co-infection with chlamydia is common, doctors may prescribe a combination of antibiotics, such as ceftriaxone with doxycycline or azithromycin, to treat both diseases.
Penicillin is ineffective at treating rectal gonorrhea: this is because other bacteria within the rectum produce β-lactamases that destroy penicillin. All current treatments are less effective at treating gonorrhea of the throat, so the patient must be rechecked by throat swab 72 hours or more after being given treatment, and then retreated if the throat swab is still positive.
Although gonorrhea usually does not require follow-up (with the exception of rectal or pharyngeal disease), patients are usually advised to phone for results five to seven days after diagnosis to confirm that the antibiotic they received was likely to be effective. Patients are advised to abstain from sex during this time.
Drug resistant strains are known to exist.
United States recommendations
The United States does not have a federal system of sexual health clinics, and the majority of infections are treated in family practices. A third-generation cephalosporin antibiotic such as ceftriaxone is recommended for use in most areas. Since some areas such as Hawaii and California have very high levels of resistance to fluoroquinolone antibiotics (ciprofloxacin, ofloxacin, levofloxacin) they are no longer used empirically to treat infections originating in these areas.
United Kingdom recommendations
In the United Kingdom, the majority of patients with gonorrhea are treated in dedicated sexual health clinics. The current recommendation is for ceftriaxone or cefixime as first line therapy; no resistance to either drug has yet been reported in the UK. Levels of spectinomycin resistance in the UK are less than 1%, which would make it a good choice in theory, but intramuscular spectinomycin injection is very painful.
Azithromycin (given as a single dose of 2 g) is recommended if there is concurrent infection with chlamydia. A single dose of oral ciprofloxacin 500 mg is effective if the organism is known to be sensitive, but fluoroquinolones were removed from the UK recommendations for empirical therapy in 2003 because of increasing resistance rates. In 2005, resistance rates for ciprofloxacin were 22% for the whole of the UK (42% for London, 10% for the rest of the UK).[1]
Historical Perspective of Treatment
Historically it has been suggested that mercury was used as a treatment for gonorrhea. Surgeons tools on board the recovered English warship the Mary Rose included a syringe that, according to some, was used to inject the mercury via the urinary meatus into any unfortunate crewman suffering from gonorrhea. Silver nitrate was one of the widely used drugs in the 19th century, but it became replaced by Protargol. Arthur Eichengrün invented this type of collodial silver which was marketed by Bayer from 1897 on. The silver based treatment was used until the first antibiotics came in use in the 1940's. [2]
Natural history, Complications, and Prognosis
In men, inflammation of the epididymis (epididymitis), prostate gland (prostatitis) and urethral structure (urethritis) can result from untreated gonorrhea.
In women, untreated gonorrhea can result in cyst and abscess formation in one or more of the greater vestibular glands (bartholinitis), causing trouble walking; PID; and Fitz-Hugh-Curtis syndrome.
The most common result of untreated gonorrhea is pelvic inflammatory disease, a serious infection of the female reproductive tract. PID causes scarring of the fallopian tubes which leads to increased risks of causing an ectopic pregnancy as a fertilized egg may not be able to pass through the narrowed, scarred fallopian tube. Ectopic pregnancies are serious conditions which are potentially life-threatening to the mother.
In both sexes, disseminated gonococcal infection (DGI) can occur, leading to multiple distant sites of infection which can include the brain, heart and joints.
When joints become involved, gonococcal arthritis can develop. Gonococcal arthritis occurs after primary infection of the genitalia, anus, or throat. This occurs in about 1% of patients who are infected with gonorrhea and is more common in women than men. Typical symptoms include a 5–7 day history of fever, shaking, chills, multiple skin lesions, fleeting migratory polyarthralgias and tenosynovitis in fingers, wrists, toes or ankles. This should be evaluated promptly with a culture of the synovial fluid, blood, cervix, urethra, rectum, skin lesion fluid, or pharynx. The underlying gonorrhea should be treated; if this is done then usually a good prognosis will follow.
Slang terms
"The clap"
Gonorrhea is also commonly known by the slang term "the clap". One suggested etymology refers to a traditional treatment used to clear the blockage in the urethra from gonorrheal pus, where the penis would be "clapped" on both sides simultaneously.[3] It could also refer to the painful sting in the male urethra, which feels like the sting of a clap (as in clapping hands) when infected with the disease. Yet another suggested source is from the old French word "clapier", meaning "brothel". Another suggested source for the term is from a notorious 18th century keeper of a brothel, Margaret Clap (better known as "Mother Clap"), though perhaps her name itself was derived from the slang term. This term has, in recent years, come to be used by extension to refer to any unspecified sexually transmitted disease.
References
- ↑ Health Protection Agency. "The gonococcal resistance to antimicrobials surveillance programme: Annual report 2005" (PDF). Retrieved 2006-10-28.
- ↑ Max Bender (1898). "Ueber neuere Antigonorrhoica (insbes. Argonin und Protargol)". Archives of Dermatological Research. 43 (1): 31–36. doi:10.1007/BF01986890.
- ↑ http://std-gov.org/stds/gonorrhea.htm
External links
| Wikimedia Commons has media related to Gonorrhea. |
- Gonorrhea Support, Information, Pictures & Videos
- http://www.cdc.gov/ncidod/diseases/submenus/sub_gonorrhea.htm
- http://www.cdc.gov/std/
- http://wwwn.cdc.gov/travel/yellowBookCh4-STD.aspx
- Gonorrhea Symptoms and Pictures
- Centers for Disease Control and Prevention: Gonorrhea Information
- Drug-resistant gonorrhea on rise among gay men
- National Institute of Allergy and Infectious Diseases: Gonorrhea Factsheet
- MayoClinic.Com: Gonorrhea
- Gonhorrhea News & Treatment Information
- It's Your Health - Gonorrhea at Health Canada Retrieved 2 May, 2007.
ar:سيلان (مرض) bg:Гонорея ca:Gonorrea cs:Kapavka da:Gonoré de:Gonorrhoe et:Gonorröa eo:Gonoreo fa:سوزاک ko:임질 id:Kencing nanah it:Blenorragia he:זיבה lt:Gonorėja hu:Kankó ms:Gonorea nl:Gonorroe no:Gonoré nn:Gonorré nds:Drüpper simple:Gonorrhea sl:Gonoreja sr:Гонореја fi:Tippuri sv:Gonorré ta:கொணோறியா uk:Гонорея