Gastric antral vascular ectasia: Difference between revisions
| Line 84: | Line 84: | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
====Traditional treatments==== | ====Traditional treatments==== | ||
GAVE is treated commonly by means of an endoscope, including [[argon plasma coagulation]] and electrocautery. Since endoscopy with argon photo coagulation is usually effective, surgery is usually not required. Endoscopy with thermal ablation is favored [[medical treatment]] because of its low side effects and low mortality, but is rarely curative. | GAVE is treated commonly by means of an endoscope, including [[argon plasma coagulation]]<ref name=Argon>{{cite journal |last1=Rosenfeld |first1=G |last2=Enns |first2=R |title=Argon photocoagulation in the treatment of gastric antral vascular ectasia and radiation proctitis |journal=Canadian Journal of Gastroenterology |volume=23 |issue=12 |pages=801–4 |year=2009 |pmid=20011731 |pmc=2805515}}</ref> and electrocautery. Since endoscopy with argon photo coagulation is usually effective, surgery is usually not required. Endoscopy with thermal ablation is favored [[medical treatment]] because of its low side effects and low mortality, but is rarely curative. | ||
Complications of coagulation therapy include | Complications of coagulation therapy include | ||
Revision as of 16:06, 5 September 2012
| Gastric antral vascular ectasia | ||
 | ||
|---|---|---|
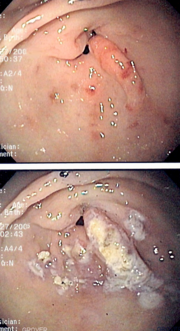
| Endoscopic image of gastric antral vascular ectasia seen as a radial pattern around the pylorus before (top) and after (bottom) treatment with argon plasma coagulation | ||
| DiseasesDB | 29505 | |
| MeSH | C06.405.748.280 | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Watermelon stomach; GAVE
Overview
Gastric antral vascular ectasia is an uncommon cause of chronic gastrointestinal bleeding or iron deficiency anemia. The condition is associated with dilated small blood vessels in the antrum, or the last part of the stomach. It is also called watermelon stomach because streaky long red areas that are present in the stomach may resemble the markings on watermelon[1].
Historical Perspective
The condition was first discovered in 1952, and reported in the literature in 1953.[2] Watermelon disease was first diagnosed by Wheeler et al. in 1979, and definitively described in four living patients by Jabbari et al. only in 1984. As of 2011, the etiology and pathogenesis are still not known.[3] However, there are several competing hypotheses as to various etiologies.
Pathophysiology
GAVE is characterized by dilated capillaries in the lamina propria with fibrin thrombi.
Microscopic Pathology

Asociated Conditions
GAVE is associated with a number of conditions, including
- Portal hypertension
- Chronic renal failure
- Collagen vascular diseases, particularly scleroderma
- Pernicious anemia
- Liver cirrhosis
- Chronic renal failure
- Bone marrow transplantation
Causes
65% of patients with both cirrhosis and GAVE are male, but a total of 30% have both conditions. The causal connection between cirrhosis and GAVE has not been proven.
A connective tissue disease has been suspected in some cases.
Autoimmunity may have something to do with it,[4] as 25% of all sclerosis patients who had a certain anti-RNA marker have GAVE. RNA autoimmunity has been suspected as a cause or marker since at least 1996.
One theory current since the 1990s focuses on a history of prolapse of the stomach into the small intestine.
Gastrin levels may indicate a hormonal connection. This may be due to vasoactive intestinal peptide and 5-hydroxy-tryptamine.
It is also possible that infection by H. pylori can cause it.
Differentiating Gastric antral vascular ectasia from other Diseases
GAVE should be differentiated from other causes of intestinal bleeding such as
The differential diagnosis is important because treatments are different.
Epidemiology and Demographics
Age
The average age of diagnosis for GAVE is 73 years of age for females, and 68 for males. Patients in their thirties have been found to have GAVE. It becomes more common in women in their eighties, rising to 4% of all such gastrointestinal conditions.
Gender
Women are about twice as often diagnosed with gastric antral vascular ectasia than men. 71% of all cases of GAVE are diagnosed in females.
Diagnosis
Symptoms
Endoscopy
The endoscopic appearance of GAVE is similar to portal hypertensive gastropathy. Dilated capillaries are seen in the endoscopy which resemble the tell-tale watermelon stripes.
Treatment
Medical Therapy
Traditional treatments
GAVE is treated commonly by means of an endoscope, including argon plasma coagulation[6] and electrocautery. Since endoscopy with argon photo coagulation is usually effective, surgery is usually not required. Endoscopy with thermal ablation is favored medical treatment because of its low side effects and low mortality, but is rarely curative.
Complications of coagulation therapy include
- Oozing
- Bleeding
- Relapse
Other treatments
Other medical treatments have been tried and include estrogen and progesterone therapy, and anti-fibrinolytic drugs such as tranexamic acid. Corticosteroids are effective, but are limited by their side effects.
Treatment of co-morbid conditions
A transjugular intrahepatic portosystemic shunt (TIPS or TIPSS) procedure is used to treat portal hypertension when that is present as an associated condition. Unfortunately, the TIPSS, which has been used for similar conditions, may cause or exacerbate hepatic encephalopathy.[7][8] TIPSS-related encephalopathy occurs in about 30% of cases, with the risk being higher in those with previous episodes of encephalopathy, higher age, female sex, and liver disease due to causes other than alcohol.[9] The patient, with his or her physician and family, must balance out a reduction in bleeding caused by TIPS with the significant risk of encephalopathy. Various shunts have been shown in a meta-study of 22 studies to be effective treatment to reduce bleeding, yet none have any demonstrated survival advantage.
If there is cirrhosis of the liver that has progressed to liver failure, then lactulose may be prescribed for hepatic encephalopathy, especially for Type C encephalopathy with diabetes. Also, antibiotics such as neomycin, metronidazole, and rifaximin may be used effectively to treat the encephalopathy by removing nitrogen-producing bacteria from the gut.
Paracentesis, a medical procedure involving needle drainage of fluid from a body cavity,[10] may be used to remove fluid from the peritoneal cavity in the abdomen for such cases. This procedure uses a large needle, similar to the better-known amniocentesis.
Surgery
Surgery, consisting of excision of part of the lower stomach, also called antrectomy, is another option. Antrectomy is the resection, or surgical removal, of a part of the stomach known as the antrum.[11]
Laparoscopic surgery is possible in some cases, and as of 2003, was a novel approach to treating watermelon stomach.[12]
A treatment used sometimes is endoscopic band ligation.[13]
In 2010, a team of Japanese surgeons performed a novel endoscopic ablation of gastric antral vascular ectasia.[14] The experimental procedure resulted in no complications.[14]
Relapse is possible, even after treatment by argon plasma coagulation and progesterone.[15] In such cases of relapse, surgery may be the only option; in one case that involved Endoscopic mucosal resection.[16]
Antrectomy or other surgery is used as a last resort for GAVE. The risks of surgery should be considered. It is said that surgery is the only cure for GAVE.
References
- ↑ Suit P, Petras R, Bauer T, Petrini J (1987). "Gastric antral vascular ectasia. A histologic and morphometric study of "the watermelon stomach"". Am J Surg Pathol. 11 (10): 750–7. PMID 3499091.
- ↑ Rider, JA; Klotz, AP; Kirsner, JB (1953). "Gastritis with veno-capillary ectasia as a source of massive gastric hemorrhage". Gastroenterology. 24 (1): 118–23. PMID 13052170.
- ↑ Tuveri, Massimiliano; Borsezio, Valentina; Gabbas, Antonio; Mura, Guendalina (2007). "Gastric antral vascular ectasia—an unusual cause of gastric outlet obstruction: report of a case". Surgery today. 37 (6): 503–5. doi:10.1007/s00595-006-3430-3. PMID 17522771.
- ↑ Valdez, BC; Henning, D; Busch, RK; Woods, K; Flores-Rozas, H; Hurwitz, J; Perlaky, L; Busch, H (1996). "A nucleolar RNA helicase recognized by autoimmune antibodies from a patient with watermelon stomach disease". Nucleic Acids Research. 24 (7): 1220–4. doi:10.1093/nar/24.7.1220. PMC 145780. PMID 8614622.
- ↑ Spahr, L; Villeneuve, J-P; Dufresne, M-P; Tasse, D; Bui, B; Willems, B; Fenyves, D; Pomier-Layrargues, G (1999). "Gastric antral vascular ectasia in cirrhotic patients: absence of relation with portal hypertension". Gut. 44 (5): 739. doi:10.1136/gut.44.5.739. PMC 1727493. PMID 10205216.
- ↑ Rosenfeld, G; Enns, R (2009). "Argon photocoagulation in the treatment of gastric antral vascular ectasia and radiation proctitis". Canadian Journal of Gastroenterology. 23 (12): 801–4. PMC 2805515. PMID 20011731.
- ↑ Khan S, Tudur Smith C, Williamson P, Sutton R (2006). Khan, Saboor A, ed. "Cochrane Database of Systematic Reviews". Cochrane Database Syst Rev (4): CD000553. doi:10.1002/14651858.CD000553.pub2. PMID 17054131.
|chapter=ignored (help) - ↑ Saab S, Nieto JM, Lewis SK, Runyon BA (2006). Saab, Sammy, ed. "TIPSS versus paracentesis for cirrhotic patients with refractory ascites". Cochrane Database Syst Rev (4): CD004889. doi:10.1002/14651858.CD004889.pub2. PMID 17054221.
|chapter=ignored (help) - ↑ Sundaram V, Shaikh OS (2009). "Hepatic encephalopathy: pathophysiology and emerging therapies". Med. Clin. North Am. 93 (4): 819–36, vii. doi:10.1016/j.mcna.2009.03.009. PMID 19577116. Unknown parameter
|month=ignored (help) - ↑ Template:DorlandsDict
- ↑ Surgery Encyclopedia website page on Antrectomy. Accessed September 29, 2010.
- ↑ Sherman, V; Klassen, DR; Feldman, LS; Jabbari, M; Marcus, V; Fried, GM (2003). "Laparoscopic antrectomy: a novel approach to treating watermelon stomach". Journal of the American College of Surgeons. 197 (5): 864. doi:10.1016/S1072-7515(03)00600-8. PMID 14585429.
- ↑ Wells, C; Harrison, M; Gurudu, S; Crowell, M; Byrne, T; Depetris, G; Sharma, V (2008). "Treatment of gastric antral vascular ectasia (watermelon stomach) with endoscopic band ligation". Gastrointestinal Endoscopy. 68 (2): 231. doi:10.1016/j.gie.2008.02.021. PMID 18533150.
- ↑ 14.0 14.1 Komiyama, Masae; Fu, K; Morimoto, T; Konuma, H; Yamagata, T; Izumi, Y; Miyazaki, A; Watanabe, S (2010). "A novel endoscopic ablation of gastric antral vascular ectasia". World Journal of Gastrointestinal Endoscopy. 2 (8): 298. doi:10.4253/wjge.v2.i8.298. PMC 2999147. PMID 21160630.
- ↑ Shibukawa, G; Irisawa, A; Sakamoto, N; Takagi, T; Wakatsuki, T; Imamura, H; Takahashi, Y; Sato, A; Sato, M (2007). "Gastric antral vascular ectasia (GAVE) associated with systemic sclerosis: relapse after endoscopic treatment by argon plasma coagulation". Internal medicine (Tokyo, Japan). 46 (6): 279–83. doi:10.2169/internalmedicine.46.6203. PMID 17379994.
- ↑ Katsinelos, P; Chatzimavroudis, G; Katsinelos, T; Panagiotopoulou, K; Kotakidou, R; Tsolkas, G; Triantafillidis, I; Papaziogas, B (2008). "Endoscopic mucosal resection for recurrent gastric antral vascular ectasia". VASA. Zeitschrift fur Gefasskrankheiten. Journal for vascular diseases. 37 (3): 289–92. doi:10.1024/0301-1526.37.3.289. PMID 18690599.