Gas gangrene: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
MeshID = D005738 | | MeshID = D005738 | | ||
}} | }} | ||
{{ | {{Gas gangrene}} | ||
{{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | ||
Revision as of 20:16, 26 November 2012
For patient information click here
| Gas gangrene | |
 | |
|---|---|
| Photograph before right leg amputation (hemipelvectomy) of a patient with gas gangrene. The right thigh is swollen, edematous and discoloured with necrotic bullae (large blisters). An impressive crepitation is already palpable. At this juncture, the patient is in shock. | |
| ICD-10 | A48.0 |
| ICD-9 | 040.0 |
| DiseasesDB | 31141 |
| MedlinePlus | 000620 |
| MeSH | D005738 |
|
Gas gangrene Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Gas gangrene On the Web |
|
American Roentgen Ray Society Images of Gas gangrene |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Gas gangrene (also known as "Clostridial myonecrosis"[1]:269, and "Myonecrosis"[2]) is a bacterial infection that produces gas in tissues in gangrene. It is a deadly form of gangrene usually caused by Clostridium perfringens bacteria. It is a medical emergency.
Myonecrosis is a condition of necrotic damage, specifically to muscle tissue. It is often seen in infections with Clostridium perfringens or any of myriad soil-borne anaerobic bacteria. Bacteria cause myonecrosis via specific exotoxins. These microorganisms are opportunistic and generally enter the body via significant skin breakage. In wartime particularly, the unhygienic conditions and frequent gross injuries meant that gangrenous infection of soil-borne bacteria was particularly prevalent. Indeed mankind has long suffered the ill-effects of gangrenous infections throughout history.
Other causes of myonecrosis include ischemic necrosis, caused by vascular blockage (e.g. diabetes type II), tumours that block or hoard blood supply and disseminated intravascular coagulation (DIC) or other thromboses.
Pathophysiology
Gas gangrene is caused by exotoxin-producing Clostridial species (most often Clostridium perfringens), which is mostly found in soil but also found as normal gut flora, and other anaerobes (e.g. Bacteroides and anaerobic streptococci). The exotoxin is commonly found in C. perfringens type A strain and is known as alpha toxin. These environmental bacteria may enter the muscle through a wound and go on to proliferate in necrotic tissue and secrete powerful toxins. These toxins destroy nearby tissue, generating gas at the same time.
A gas composition of 5.9% hydrogen, 3.4% carbon dioxide, 74.5% nitrogen and 16.1% oxygen was reported in one clinical case.[3]
Myonecrosis differs slightly from other types of necrosis. While the underlying causes are almost identical, the type of affected tissue (namely muscle tissue) is significantly more important for the patient's general health. Superficial necrosis is unsightly, and can lead to unattractive scarring but otherwise does not affect the patient's likelihood of survival nor physical capability to the same extent. Conversely, massive myonecrosis will likely result in the loss of movement of the entire region. If the necrotic damage is allowed to continue throughout an affected limb then often that entire limb is lost permanently.
Soil-borne anaerobes are particularly well adapted to surviving harsh conditions. Often there is a scarcity of nutrition and the presence of numerous other species competing for resources. Changes in pH and temperature are often significant also. Competing bacteria often also possess the ability to create exotoxins that assist them in competing with other microbes in their natural environment. When such bacteria are able to enter a living host, they encounter a vast supply of nutrients, warm conditions and an abundance of water. This enables the microbes to rapidly proliferate, far in excess of the immune system's capability to defend, particularly as prokaryotic bacteria possess a far greater capacity for multiplication than the host's immune system. The combination of bacterial load and ability to multiply is the basis for the microbes' ability to cause massive infection. Alongside such rapid proliferation is a corresponding mass production of exotoxin that causes severe damage to local tissue in the host. One such exotoxin is produced by C. perfringens and is responsible for the disease manifestations. This exotoxin is known as alpha toxin.[4]
Following a massive infection, gross injury and depletion of the host's immune capability results in system wide sepsis. This is partly due to the burden on the immune system, its corresponding release of inflammatory cytokines and the distribution of bacterial toxins. Massive infection is likely to result in death from a combination of system wide septic shock and the unintentionally damaging effects of the immune response. In animals, disability and distress caused by all of these factors markedly increases the chance of predation.
Treatment
Any significantly massive infection is a medical emergency. In cases of gangrene, the infection is so severe by the time that a diagnosis is made that countering the bacterial load is impossible even with the strongest available antibiotics, for example gentamycin and vancomycin. Antibiotics alone are not effective because they don't penetrate ischemic muscles enough to be effective. However, penicillin is given as an adjuvant treatment to surgery.
There are two major reasons for this; current antibiotics only prevent replication of bacteria and the production of toxins continues in pre-existing bacteria. Also, the extent of injury caused by the infection may leave the muscle tissues so damaged that the body will never be able to replace the lost structures (including vasculature).
Often the only available cure is amputation, which physically removes the source of infection. Understandably this is not the favoured option unless circumstances are particularly dire.
In addition to surgery and antibiotics, hyperbaric oxygen therapy (HBOT) is used and acts to inhibit the growth of and kill the anaerobic C. perfringens.

Case Studies
Case #1: Clostridial myonecrosis
Clinical Summary
This 68-year-old white male with insulin-dependent diabetes was admitted one day before his death. The chief complaints were the occurrence of chills and fever since passing a kidney stone two days earlier. In the last day, the right leg had become swollen. The most striking physical findings were redness of the right posterior calf and crepitance in both legs. The patient's white blood cell count was found to be 34,000 cells/cmm and the packed red blood cell volume (PCV) was 18%. Within hours, the right calf became tense and the crepitance spread up to the nipple line. The patient vomited, aspirated the vomitus, and died 10 hours after admission.
Histopathological Findings
-
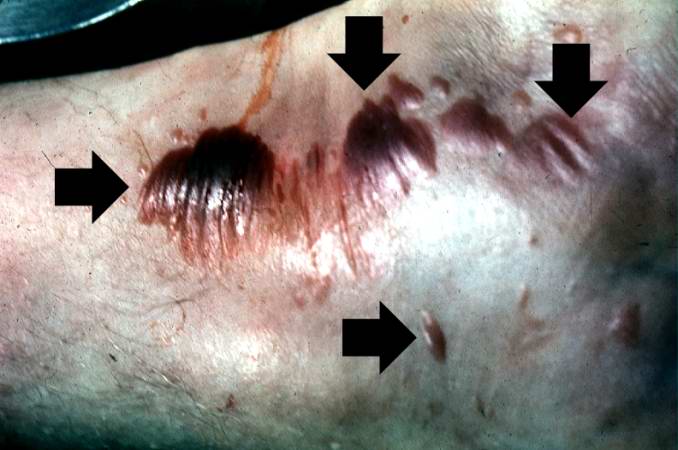
This gross photograph shows a close-up view of hemorrhagic blebs (arrows) on the skin. The blebs on the skin are accumulations of gas being discharged into the tissues from the Clostridium perfringens. This gas produces crepitance.
-
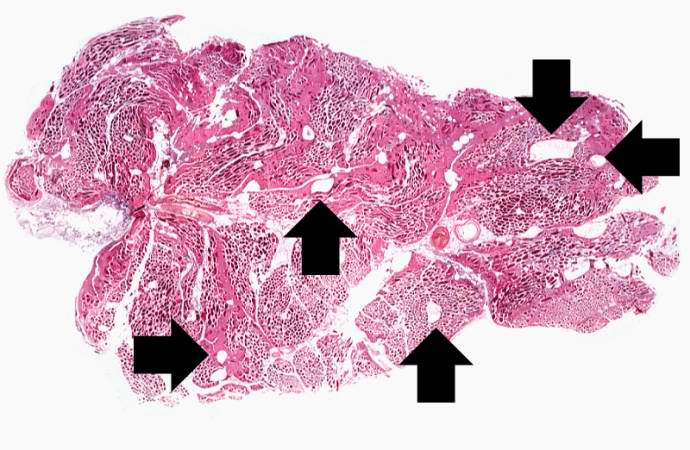
This is a low-power photomicrograph of muscle fascicles containing large gas bubbles (arrows). Note that there is no inflammatory reaction in this section.
-
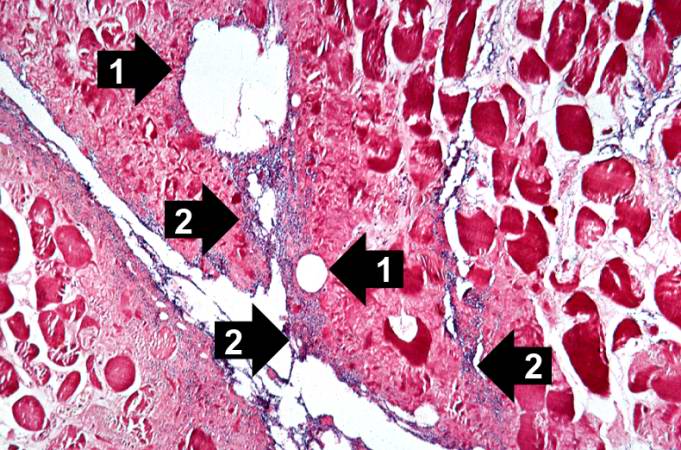
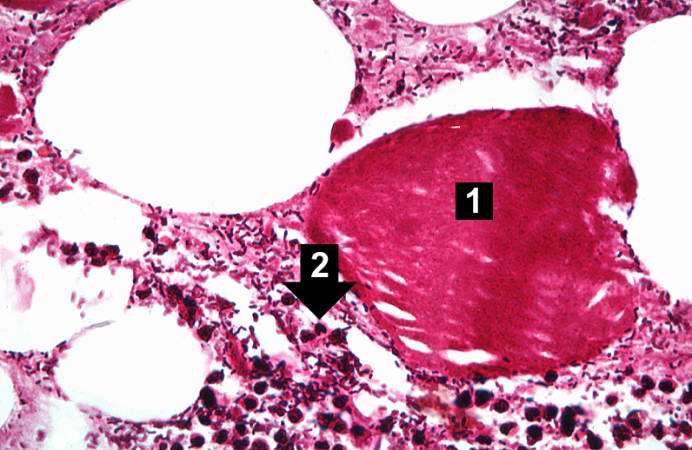
This is a high-power photomicrograph of skeletal muscle. The muscle cells are hypereosinophilic and most do not contain nuclei, indicating that these cells are dead or dying. The round clear spaces (1) in this tissue correspond to gas accumulations prior to death. In between the bundles of muscle cells, accumulations of small dark blue-staining bacterial organisms can be seen (2). Also note that there is no inflammatory response in this tissue.
-
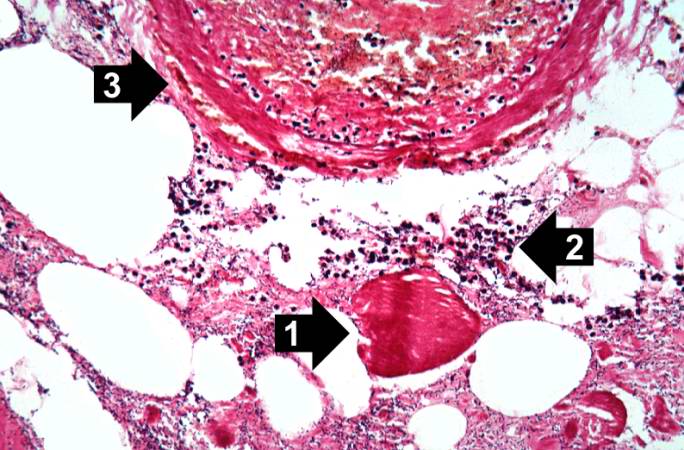
This high-power photomicrograph shows the gas accumulation present in the tissue, a necrotic muscle cell (1), and a mild inflammatory response (2). There is also a thrombosed blood vessel (3). The blue-staining rods (bacterial organisms) can barely be appreciated at this magnification.
-
This higher-power photomicrograph of the previous image provides a clearer view of gas bubbles in the tissue, the necrotic hypereosinophilic muscle cell (1), and the mild inflammatory reaction (2). At this magnification, the bacteria located throughout this section can be better appreciated.
-
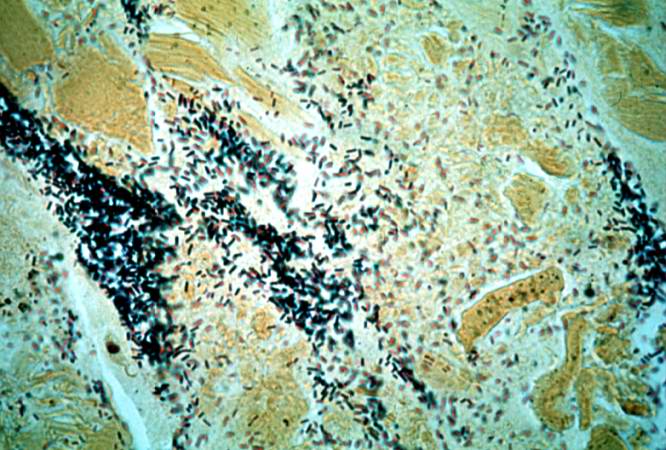
This is a high-power photomicrograph of a tissue section stained with a tissue Gram's stain (Brown & Brenn). The Gram-positive bacilli can be seen throughout this tissue section.
References
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ↑ Rapini, Ronald P.; Bolognia, Jean L.; Jorizzo, Joseph L. (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 1-4160-2999-0.
- ↑ ^ Chi CH, Chen KW, Huang JJ, Chuang YC, Wu MH (1995). "Gas composition in Clostridium septicum gas gangrene". J Formos Med Assoc. 94 (12): 757–9. PMID 8541740.
- ↑ Awad, M.M., Bryant, A.E., Stevens, D.L. & Rood, J.I. Virulence studies on chromosomal alpha-toxin and alpha-toxin mutants constructed by allelic exchange provide genetic evidence for the essential role of alpha-toxin in Clostridium perfringens-mediated gas gangrene. Mol. Microbiol. 15:191−202 (1995).