Folliculitis: Difference between revisions
| Line 26: | Line 26: | ||
**chronicity of the condition( acute vs chronic/recurrent) | **chronicity of the condition( acute vs chronic/recurrent) | ||
* | *Non-infectious variant of the folliculitis include Pseudofolliculitis barbae,Eosinophilic folliculitis ,Folliculitis decalvans or tufted folliculitis and folliculitis keloidalis to mention a few. | ||
==Pathophysiology== | ==Pathophysiology== | ||
Revision as of 04:33, 24 November 2018
| Folliculitis | |
 | |
|---|---|
| Folliculitis, Fungal; Pustular Diseases Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | L73.8 |
| ICD-9 | xxx |
| DiseasesDB | 31367 |
| eMedicine | DERM/159 |
|
WikiDoc Resources for Folliculitis |
|
Articles |
|---|
|
Most recent articles on Folliculitis Most cited articles on Folliculitis |
|
Media |
|
Powerpoint slides on Folliculitis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Folliculitis at Clinical Trials.gov Clinical Trials on Folliculitis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Folliculitis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Folliculitis Discussion groups on Folliculitis Patient Handouts on Folliculitis Directions to Hospitals Treating Folliculitis Risk calculators and risk factors for Folliculitis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Folliculitis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2].
Overview
Folliculitis is the inflammation of one or more hair follicles. The condition may occur anywhere on the skin.
Classification
- Folliculitis can be classified in a variety of ways based on the:
- Depth of the involvement(superficial vs deep)
- Underlying etiological agent(infectious vs non infectious)
- chronicity of the condition( acute vs chronic/recurrent)
- Non-infectious variant of the folliculitis include Pseudofolliculitis barbae,Eosinophilic folliculitis ,Folliculitis decalvans or tufted folliculitis and folliculitis keloidalis to mention a few.
Pathophysiology
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Clinical Features
Differentiating [disease name] from other Diseases
- Folliculitis must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- Acne vulgaris
- Acne rosasea
- Periorofacial dermatitis
- Acneform Eruptions
- Hidraadenitis suppurativa
- Rosacea
- Transient acantholytic dermatosis
- Insect bite
- Papular urticaria
- Milia
- Contact dermatitis
Epidemiology and Demographics
- Superficial Folliculitis is although commonly seen but the exact incidence is not known.
Age
- Patients of all age groups may develop Folliculitis.
- Superficial Folliculitis and Hot tub folliculitis is more commonly observed among adults than children.
- Demodex folliculitis is more commonly seen in adults however it also has been implicated in facial pustules and papules in children.[1]
Gender
- Superficial Folliculitis affects men and women equally.
- Males are more commonly affected with Herpes folliculitis and Pityrosporum folliculitis[2] than females.
- Eosinophilic Folliculitis has been seen in HIV-infected men, women, and children. [3][4][5]
Race
- There is no racial predilection for Folliculitis however Pseudofolliculitis barbae usually affects individuals of the African descent.
Causes
Most carbuncles and furuncles and other cases of folliculitis develop from Staphylococcus aureus.
Folliculitis starts when hair follicles are damaged by friction from clothing, blockage of the follicle, or shaving. In most cases of folliculitis, the damaged follicles are then infected with the bacteria Staphylococcus (staph).
Iron deficiency anemia is sometimes associated with chronic cases
- Sycosis barbae or barber's itch is a staph infection of the hair follicles in the bearded area of the face, usually the upper lip. Shaving aggravates the condition.
- Tinea barbae is similar to barber's itch, but the infection is caused by the fungus T._rubrum.
- Pseudofolliculitis barbae is a disorder occurring primarily in men of African descent. If curly beard hairs are cut too short, they may curve back into the skin and cause inflammation.
- Hot tub folliculitis is caused by the bacteria Pseudomonas aeruginosa often found in new hot tubs. The folliculitis usually occurs after sitting in a hot tub that was not properly cleaned before use. Symptoms are found around the body parts that sit in the hot tub -- typically the legs, hips and buttocks and surrounding areas. Symptoms are typically amplified around regions that were covered by wet clothing, such as bathing suits.
- Drug Side Effect: Betamethasone valerate, Betamethasone dipropionate, Clocortolone pivalate, Desoximetasone, Diflorasone, Sorafenib, Mometasone furoate
Risk Factors
- Common risk factors in the development of Folliculitis are:
- Frequent shaving against the direction of the hair growth
- Immunosuppresion
- Presence of dermatosis
- Long term oral antibiotic use
- Hot tub bath
- obesity
- Diabetes
- HIV,late stage esp with low CD4 cell count
- Prolonged used of topical steriods
- Exposure to the hot humid temperature
- Patients treated with EGFR inhibitors[6]
- post vaccination esp after the small pox and anthrax vaccine[7][8]
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of folliculitis include cellulitis, furunculosis, scarring, sinus tract formation, permanent hair loss and recurrence in some cases.
- Prognosis is generally excellent if the causative agent is accurately identified and treated.
Diagnosis
Folliculitis is a clinical diagnosis so diagnosis is usually based on history and physical examination.
Symptoms
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings
- There are no imaging study findings associated with Folliculitis.
Other Diagnostic Studies
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
Treatment of folliculitis depends on the causative agent being involved.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
Gallery
Extremities
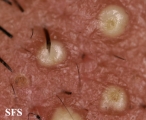
Folliculitis Of Barbae
-
Folliculitis Of Barbae.
With permission from Dermatology Atlas. -
Folliculitis Of Barbae.
With permission from Dermatology Atlas. -
Folliculitis Of Barbae.
With permission from Dermatology Atlas.
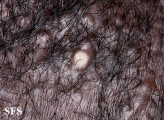
Folliculitis cheloidalis
-
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas -
Folliculitis Cheloidalis.
Used with permission of Dermatology Atlas
Treatment
- Topical antiseptic treatment is adequate for most cases
- Some patients may benefit from systemic flucloxacillin
References
- ↑ Brown M, Hernández-Martín A, Clement A, Colmenero I, Torrelo A (2014). "Severe demodexfolliculorum-associated oculocutaneous rosacea in a girl successfully treated with ivermectin". JAMA Dermatol. 150 (1): 61–3. doi:10.1001/jamadermatol.2013.7688. PMID 24284904.
- ↑ Poli F (2012). "Differential diagnosis of facial acne on black skin". Int J Dermatol. 51 Suppl 1: 24–6, 27–9. doi:10.1111/j.1365-4632.2012.05559.x. PMID 23210948.
- ↑ Basarab T, Russell Jones R (1996). "HIV-associated eosinophilic folliculitis: case report and review of the literature". Br J Dermatol. 134 (3): 499–503. PMID 8731676.
- ↑ Ramdial PK, Morar N, Dlova NC, Aboobaker J (1999). "HIV-associated eosinophilic folliculitis in an infant". Am J Dermatopathol. 21 (3): 241–6. PMID 10380045.
- ↑ Hayes BB, Hille RC, Goldberg LJ (2004). "Eosinophilic folliculitis in 2 HIV-positive women". Arch Dermatol. 140 (4): 463–5. doi:10.1001/archderm.140.4.463. PMID 15096375.
- ↑ Bachet JB, Peuvrel L, Bachmeyer C, Reguiai Z, Gourraud PA, Bouché O; et al. (2012). "Folliculitis induced by EGFR inhibitors, preventive and curative efficacy of tetracyclines in the management and incidence rates according to the type of EGFR inhibitor administered: a systematic literature review". Oncologist. 17 (4): 555–68. doi:10.1634/theoncologist.2011-0365. PMC 3336835. PMID 22426526.
- ↑ Oh RC (2005). "Folliculitis after smallpox vaccination: a report of two cases". Mil Med. 170 (2): 133–6. PMID 15782834.
- ↑ Greenberg RN, Schosser RH, Plummer EA, Roberts SE, Caldwell MA, Hargis DL; et al. (2004). "Urticaria, exanthems, and other benign dermatologic reactions to smallpox vaccination in adults". Clin Infect Dis. 38 (7): 958–65. doi:10.1086/382360. PMID 15034827.