Fibroadenoma other diagnostic studies
|
Fibroadenoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Fibroadenoma other diagnostic studies On the Web |
|
American Roentgen Ray Society Images of Fibroadenoma other diagnostic studies |
|
Risk calculators and risk factors for Fibroadenoma other diagnostic studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2] Associate Editor(s)-in-Chief: Haytham Allaham, M.D. [3]
Overview
The definitive diagnosis of fibroadenoma is confirmed by an ultrasound guided biopsy. Characteristic findings for fibroadenoma on microscopic histopathological analysis can be found here.[1]
Other Diagnostic Studies
Aspiration Cytology
- The definitive diagnosis of fibroadenoma is confirmed by an ultrasound guided biopsy. Characteristic findings for fibroadenoma on microscopic histopathological analysis can be found here.[1]
- In combination with clinical diagnosis of fibroadenoma, fine needle aspiration (FNA) can improve the sensitivity of the diagnosis to 86%, with a specificity of 76%.[2]
- Aspiration cytology may confuse fibroadenomas with other benign breast lesions, false diagnosis of a malignant process is uncommmon.[2]
- Indications for an ultrasound guided biopsy include:[3]
- Rapidly enlarging mass
- Atypical findings on ultrasound such as non-circumscribed margins, complex solid and cystic components, posterior acoustic shadowing,
- A lesion greater than 3 cm in size, with no previous studies for comparison
- Patients preference
- History of a risk factor for malignancy regardless of the lesion having a benign appearance on ultrasonography. Examples include a prior chest irradiation, known concurrent cancer not involving the breast, family history of breast cancer.
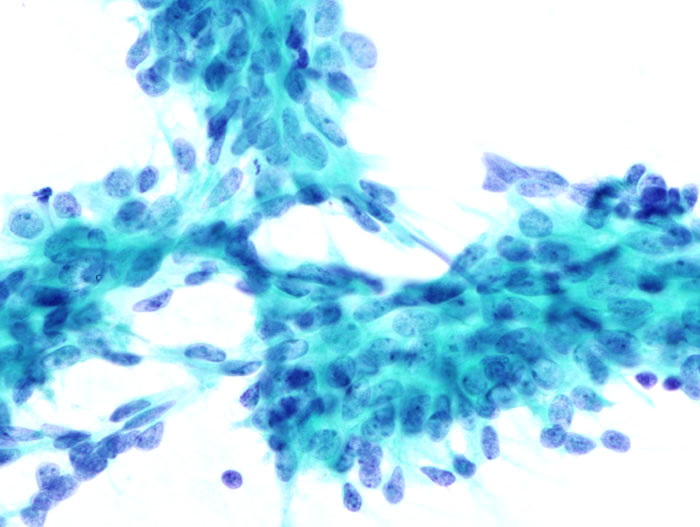
- The characteristic cytologic features of fibroadenomas include:[2]
- Clusters of spindle cells without inflammatory or fat cells. This is found in 96% of all fibroadenomas.
- Aggregates of cells with a papillary configuration resembling elk antler (antler horn clusters). Found in about 93%.
- Uniform cells with well-defined cytoplasm lying in rows and columns (honeycomb sheets). Found in about 95%
- A "triple assessment approach" refers to the combination of clinical breast examination, imaging and percutaneous tissue study. This approach allows a 95% accurate differentiation between a benign and malignant lesion.[4]

Vacuum-Assisted Ultrasound Guided Biopsy
- It involves usage of a hollow bore needle to make multiple percutaneous passes (under ultrasound or stereotactic guidance) with subsequent aspiration of the breast tissue via vacuum suction.[5]
- The procedure is said to be complete when the mass appears to be radiographically removed completely (judging via radiographic guidance).[5]
- Most patients that undergo this procedure are more satisfied with the cosmetic outcome when compared to patients that undergo conventional open excision.[6]
- Hemorrhage and hematoma are the most commmon complications associated with this procedure (due to serial core biopsies), occurring at a rate of 0-13%.
References
- ↑ 1.0 1.1 Fibroadenoma. Radiopaedia (2015) http://radiopaedia.org/articles/fibroadenoma-of-the-breast-1 Accessed on January, 29 2016
- ↑ 2.0 2.1 2.2 Greenberg R, Skornick Y, Kaplan O (September 1998). "Management of breast fibroadenomas". J Gen Intern Med. 13 (9): 640–5. PMC 1497021. PMID 9754521.
- ↑ Lee EJ, Chang YW, Oh JH, Hwang J, Hong SS, Kim HJ (2018). "Breast Lesions in Children and Adolescents: Diagnosis and Management". Korean J Radiol. 19 (5): 978–991. doi:10.3348/kjr.2018.19.5.978. PMC 6082765. PMID 30174488.
- ↑ Sperber F, Blank A, Metser U, Flusser G, Klausner JM, Lev-Chelouche D (2003). "Diagnosis and treatment of breast fibroadenomas by ultrasound-guided vacuum-assisted biopsy". Arch Surg. 138 (7): 796–800. doi:10.1001/archsurg.138.7.796. PMID 12860764.
- ↑ 5.0 5.1 Lee M, Soltanian HT (2015). "Breast fibroadenomas in adolescents: current perspectives". Adolesc Health Med Ther. 6: 159–63. doi:10.2147/AHMT.S55833. PMC 4562655. PMID 26366109.
- ↑ Lakoma A, Kim ES (2014). "Minimally invasive surgical management of benign breast lesions". Gland Surg. 3 (2): 142–8. doi:10.3978/j.issn.2227-684X.2014.04.01. PMC 4115760. PMID 25083508.