Dofetilide: Difference between revisions
No edit summary |
No edit summary |
||
| Line 114: | Line 114: | ||
|useInNursing=There is no information on the presence of dofetilide in breast milk. Patients should be advised not to breast-feed an infant if they are taking TIKOSYN. | |useInNursing=There is no information on the presence of dofetilide in breast milk. Patients should be advised not to breast-feed an infant if they are taking TIKOSYN. | ||
|useInPed=The safety and effectiveness of TIKOSYN in children (<18 years old) has not been established. | |useInPed=The safety and effectiveness of TIKOSYN in children (<18 years old) has not been established. | ||
|useInGeri=Of the total number of patients in clinical studies of TIKOSYN, 46% were 65 to 89 years old. No overall differences in safety, effect on QTc, or effectiveness were observed between elderly and younger patients. Because elderly patients are more likely to have decreased renal function with a reduced creatinine clearance, care must be taken in dose selection (see DOSAGE AND ADMINISTRATION). | |useInGeri=Of the total number of patients in clinical studies of TIKOSYN, 46% were 65 to 89 years old. No overall differences in safety, effect on QTc, or effectiveness were observed between elderly and younger patients. Because elderly patients are more likely to have decreased renal function with a reduced creatinine clearance, care must be taken in dose selection (see DOSAGE AND ADMINISTRATION). | ||
|useInGender=Female patients constituted 32% of the patients in the placebo-controlled trials of TIKOSYN. As with other drugs that cause Torsade de Pointes, TIKOSYN was associated with a greater risk of Torsade de Pointes in female patients than in male patients. During the TIKOSYN clinical development program, the risk of Torsade de Pointes in females was approximately 3 times the risk in males. Unlike Torsade de Pointes, the incidence of other [[ventricular arrhythmias]] was similar in female patients receiving TIKOSYN and patients receiving placebo. Although no study specifically investigated this risk, in post-hoc analyses, no increased mortality was observed in females on TIKOSYN compared to females on placebo. | |useInGender=Female patients constituted 32% of the patients in the placebo-controlled trials of TIKOSYN. As with other drugs that cause Torsade de Pointes, TIKOSYN was associated with a greater risk of Torsade de Pointes in female patients than in male patients. During the TIKOSYN clinical development program, the risk of Torsade de Pointes in females was approximately 3 times the risk in males. Unlike Torsade de Pointes, the incidence of other [[ventricular arrhythmias]] was similar in female patients receiving TIKOSYN and patients receiving placebo. Although no study specifically investigated this risk, in post-hoc analyses, no increased mortality was observed in females on TIKOSYN compared to females on placebo. | ||
| Line 121: | Line 120: | ||
|othersTitle=Cardiac Conduction Disturbances | |othersTitle=Cardiac Conduction Disturbances | ||
|useInOthers=Animal and human studies have not shown any adverse effects of dofetilide on conduction velocity. No effect on AV nodal conduction following TIKOSYN treatment was noted in normal volunteers and in patients with 1st degree heart block. Patients with [[sick sinus syndrome]] or with 2nd or 3rd degree heart block were not included in the Phase 3 clinical trials unless a functioning pacemaker was present. TIKOSYN has been used safely in conjunction with [[pacemakers]] (53 patients in DIAMOND studies, 136 in trials in patients with ventricular and [[supraventricular arrhythmias]]). | |useInOthers=Animal and human studies have not shown any adverse effects of dofetilide on conduction velocity. No effect on AV nodal conduction following TIKOSYN treatment was noted in normal volunteers and in patients with 1st degree heart block. Patients with [[sick sinus syndrome]] or with 2nd or 3rd degree heart block were not included in the Phase 3 clinical trials unless a functioning pacemaker was present. TIKOSYN has been used safely in conjunction with [[pacemakers]] (53 patients in DIAMOND studies, 136 in trials in patients with ventricular and [[supraventricular arrhythmias]]). | ||
|administration=* Therapy with TIKOSYN must be initiated (and, if necessary, re-initiated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of three days. Additionally, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm. | |||
* The dose of TIKOSYN must be individualized according to calculated creatinine clearance and QTc. (QT interval should be used if the heart rate is <60 beats per minute. There are no data on use of TIKOSYN when the heart rate is <50 beats per minute.) The usual recommended dose of TIKOSYN is 500 mcg BID, as modified by the dosing algorithm described below. For consideration of a lower dose, see Special Considerations below. | |||
* Serum potassium should be maintained within the normal range before TIKOSYN treatment is initiated and should be maintained within the normal range while the patient remains on TIKOSYN therapy. (See WARNINGS, Hypokalemia and Potassium-Depleting Diuretics). In clinical trials, potassium levels were generally maintained above 3.6–4.0 mEq/L. | |||
* Patients with atrial fibrillation should be anticoagulated according to usual medical practice prior to electrical or pharmacological cardioversion. Anticoagulant therapy may be continued after cardioversion according to usual medical practice for the treatment of people with AF. Hypokalemia should be corrected before initiation of TIKOSYN therapy (see WARNINGS, Ventricular Arrhythmia). | |||
* Patients to be discharged on TIKOSYN therapy from an inpatient setting as described above must have an adequate supply of TIKOSYN, at the patient's individualized dose, to allow uninterrupted dosing until the patient receives the first outpatient supply. | |||
* TIKOSYN is distributed only to those hospitals and other appropriate institutions confirmed to have received applicable dosing and treatment initiation education programs. Inpatient and subsequent outpatient discharge and refill prescriptions are filled only upon confirmation that the prescribing physician has received applicable dosing and treatment initiation education programs. For this purpose, a list for use by pharmacists is maintained containing hospitals and physicians who have received one of the education programs. | |||
===Instructions for Individualized Dose Initiation=== | |||
=====Initiation of TIKOSYN Therapy===== | |||
'''Step 1'''. Electrocardiographic assessment: Prior to administration of the first dose, the QTc must be determined using an average of 5–10 beats. If the QTc is greater than 440 msec (500 msec in patients with ventricular conduction abnormalities), TIKOSYN is contraindicated. If heart rate is less than 60 beats per minute, QT interval should be used. Patients with heart rates <50 beats per minute have not been studied. | |||
'''Step 2'''. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance must be calculated using the following formula: | |||
[[File:Dofetilide_administration_table_01.jpg|thumb|none|400px]] | |||
When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L). | |||
'''Step 3'''. Starting Dose: The starting dose of TIKOSYN is determined as follows: | |||
[[File:Dofetilide_administration_table_02.jpg|thumb|none|400px]] | |||
'''Step 4'''. Administer the adjusted TIKOSYN dose and begin continuous ECG monitoring. | |||
'''Step 5'''. At 2–3 hours after administering the first dose of TIKOSYN, determine the QTc. If the QTc has increased by greater than 15% compared to the baseline established in Step 1 OR if the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), subsequent dosing should be adjusted as follows: | |||
[[File:Dofetilide_administration_table_03.jpg|thumb|none|400px]] | |||
'''Step 6'''. At 2–3 hours after each subsequent dose of TIKOSYN, determine the QTc (for in-hospital doses 2–5). No further down titration of TIKOSYN based on QTc is recommended. | |||
NOTE: If at any time after the second dose of TIKOSYN is given the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), TIKOSYN should be discontinued. | |||
'''Step 7'''. Patients are to be continuously monitored by ECG for a minimum of three days, or for a minimum of 12 hours after electrical or pharmacological conversion to normal sinus rhythm, whichever is greater. | |||
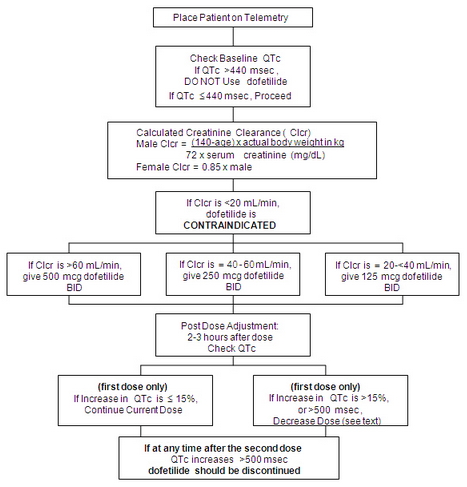
The steps described above are summarized in the following diagram: | |||
[[File:Dofetilide_administration_table_04.jpg|thumb|none|400px]] | |||
Maintenance of TIKOSYN Therapy | |||
Renal function and QTc should be re-evaluated every three months or as medically warranted. If QTc exceeds 500 milliseconds (550 msec in patients with ventricular conduction abnormalities), TIKOSYN therapy should be discontinued and patients should be carefully monitored until QTc returns to baseline levels. If renal function deteriorates, adjust dose as described in Initiation of TIKOSYN Therapy, Step 3. | |||
===Special Considerations=== | |||
Consideration of a Dose Lower than that Determined by the Algorithm | |||
The dosing algorithm shown above should be used to determine the individualized dose of TIKOSYN. In clinical trials (see CLINICAL STUDIES), the highest dose of 500 mcg BID of TIKOSYN as modified by the dosing algorithm led to greater effectiveness than lower doses of 125 or 250 mcg BID as modified by the dosing algorithm. The risk of Torsade de Pointes, however, is related to dose as well as to patient characteristics (see WARNINGS). Physicians, in consultation with their patients, may therefore in some cases choose doses lower than determined by the algorithm. It is critically important that if at any time this lower dose is increased, the patient needs to be rehospitalized for three days. Previous toleration of higher doses does not eliminate the need for rehospitalization. | |||
The maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 500 mcg BID; doses greater than 500 mcg BID have been associated with an increased incidence of Torsade de Pointes. | |||
A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time. | |||
Cardioversion | |||
If patients do not convert to normal sinus rhythm within 24 hours of initiation of TIKOSYN therapy, electrical conversion should be considered. Patients continuing on TIKOSYN after successful electrical cardioversion should continue to be monitored by electrocardiography for 12 hours post cardioversion, or a minimum of 3 days after initiation of TIKOSYN therapy, whichever is greater. | |||
'''Switch to TIKOSYN from Class I or other Class III Antiarrhythmic Therapy'''' | |||
Before initiating TIKOSYN therapy, previous antiarrhythmic therapy should be withdrawn under careful monitoring for a minimum of three (3) plasma half-lives. Because of the unpredictable pharmacokinetics of amiodarone, TIKOSYN should not be initiated following amiodarone therapy until amiodarone plasma levels are below 0.3 mcg/mL or until amiodarone has been withdrawn for at least three months. | |||
'''Stopping TIKOSYN Prior to Administration of Potentially Interacting Drugs''' | |||
If TIKOSYN needs to be discontinued to allow dosing of other potentially interacting drug(s), a washout period of at least two days should be followed before starting the other drug(s). | |||
}} | }} | ||
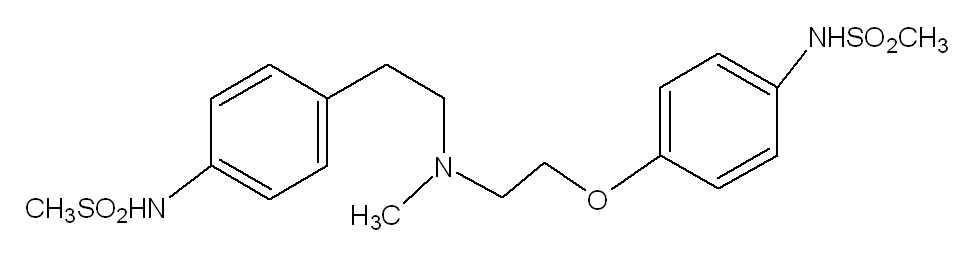
{{drugbox | IUPAC_name = N-[4-[2-[2-[4-(methanesulfonamido)phenoxy]ethyl-methyl-amino] ethyl]phenyl] methanesulfonamide | image = Dofetilide.png | CAS_number = 115256-11-6 | ATC_prefix = C01 | ATC_suffix = BD04 | ATC_supplemental = | PubChem = 71329 | DrugBank = APRD00367 | C=19 | H=27 | N=3 | O=5 | S=2 | molecular_weight = 441.567 g/mol | bioavailability = 96% (oral) | protein_bound = 60% -70% | metabolism = | elimination_half-life = 10 hours | pregnancy_category = | legal_status = | routes_of_administration = }} | {{drugbox | IUPAC_name = N-[4-[2-[2-[4-(methanesulfonamido)phenoxy]ethyl-methyl-amino] ethyl]phenyl] methanesulfonamide | image = Dofetilide.png | CAS_number = 115256-11-6 | ATC_prefix = C01 | ATC_suffix = BD04 | ATC_supplemental = | PubChem = 71329 | DrugBank = APRD00367 | C=19 | H=27 | N=3 | O=5 | S=2 | molecular_weight = 441.567 g/mol | bioavailability = 96% (oral) | protein_bound = 60% -70% | metabolism = | elimination_half-life = 10 hours | pregnancy_category = | legal_status = | routes_of_administration = }} | ||
Revision as of 19:02, 14 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
{{{blackBoxWarningTitle}}}
See full prescribing information for complete Boxed Warning.
To minimize the risk of induced arrhythmia, patients initiated or re-initiated on TIKOSYN should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous electrocardiographic monitoring, and cardiac resuscitation. For detailed instructions regarding dose selection, see DOSAGE AND ADMINISTRATION. TIKOSYN is available only to hospitals and prescribers who have received appropriate TIKOSYN dosing and treatment initiation education; see DOSAGE AND ADMINISTRATION.
|
Overview
Dofetilide is {{{aOrAn}}} Antiarrhythmic that is FDA approved for the {{{indicationType}}} of Maintenance of Normal Sinus Rhythm (Delay in AF/AFl Recurrence), Conversion of Atrial Fibrillation/Flutter. There is a Black Box Warning for this drug as shown here. Common adverse reactions include chest pain, dizziness , headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
<h4>Condition 1</h4>
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Adult)
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Dofetilide FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Contraindications
TIKOSYN is contraindicated in patients with congenital or acquired long QT syndromes. TIKOSYN should not be used in patients with a baseline QT interval or QTc >440 msec (500 msec in patients with ventricular conduction abnormalities). TIKOSYN is also contraindicated in patients with severe renal impairment (calculated creatinine clearance <20 mL/min). The concomitant use of verapamil or the cation transport system inhibitors cimetidine, trimethoprim (alone or in combination with sulfamethoxazole), or ketoconazole with TIKOSYN is contraindicated (see WARNINGS and PRECAUTIONS, Drug-Drug Interactions), as each of these drugs cause a substantial increase in dofetilide plasma concentrations. In addition, other known inhibitors of the renal cation transport system such as prochlorperazine, dolutegravir and megestrol should not be used in patients on TIKOSYN. The concomitant use of hydrochlorothiazide (alone or in combinations such as with triamterene) with TIKOSYN is contraindicated (see PRECAUTIONS, Drug-Drug Interactions) because this has been shown to significantly increase dofetilide plasma concentrations and QT interval prolongation. TIKOSYN is also contraindicated in patients with a known hypersensitivity to the drug.
Warnings
|
{{{blackBoxWarningTitle}}}
See full prescribing information for complete Boxed Warning.
To minimize the risk of induced arrhythmia, patients initiated or re-initiated on TIKOSYN should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous electrocardiographic monitoring, and cardiac resuscitation. For detailed instructions regarding dose selection, see DOSAGE AND ADMINISTRATION. TIKOSYN is available only to hospitals and prescribers who have received appropriate TIKOSYN dosing and treatment initiation education; see DOSAGE AND ADMINISTRATION.
|
Ventricular Arrhythmia TIKOSYN (dofetilide) can cause serious ventricular arrhythmias, primarily Torsade de Pointes (TdP) type ventricular tachycardia, a polymorphic ventricular tachycardia associated with QT interval prolongation. QT interval prolongation is directly related to dofetilide plasma concentration. Factors such as reduced creatinine clearance or certain dofetilide drug interactions will increase dofetilide plasma concentration. The risk of TdP can be reduced by controlling the plasma concentration through adjustment of the initial dofetilide dose according to creatinine clearance and by monitoring the ECG for excessive increases in the QT interval. Treatment with dofetilide must therefore be started only in patients placed for a minimum of three days in a facility that can provide electrocardiographic monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Calculation of the creatinine clearance for all patients must precede administration of the first dose of dofetilide. For detailed instructions regarding dose selection, see DOSAGE AND ADMINISTRATION. The risk of dofetilide induced ventricular arrhythmia was assessed in three ways in clinical studies: 1) by description of the QT interval and its relation to the dose and plasma concentration of dofetilide; 2) by observing the frequency of TdP in TIKOSYN-treated patients according to dose; 3) by observing the overall mortality rate in patients with atrial fibrillation and in patients with structural heart disease. Relation of QT Interval to Dose The QT interval increases linearly with increasing TIKOSYN dose (see Figures 1 and 2 in CLINICAL PHARMACOLOGY and Dose-Response and Concentration Response for Increase in QT Interval). Frequency of Torsade de Pointes In the supraventricular arrhythmia population (patients with AF and other supraventricular arrhythmias), the overall incidence of Torsade de Pointes was 0.8%. The frequency of TdP by dose is shown in Table 4. There were no cases of TdP on placebo.
As shown in Table 5, the rate of TdP was reduced when patients were dosed according to their renal function (see CLINICAL PHARMACOLOGY, Pharmacokinetics in Special Populations, Renal Impairment and DOSAGE AND ADMINISTRATION).
The majority of the episodes of TdP occurred within the first three days of TIKOSYN therapy (10/11 events in the studies of patients with supraventricular arrhythmias; 19/25 and 4/7 events in DIAMOND CHF and DIAMOND MI, respectively; 2/4 events in the DIAMOND AF subpopulation).
Mortality
In a pooled survival analysis of patients in the supraventricular arrhythmia population (low prevalence of structural heart disease), deaths occurred in 0.9% (12/1346) of patients receiving TIKOSYN and 0.4% (3/677) in the placebo group. Adjusted for duration of therapy, primary diagnosis, age, gender, and prevalence of structural heart disease, the point estimate of the hazard ratio for the pooled studies (TIKOSYN/placebo) was 1.1 (95% CI: 0.3, 4.3). The DIAMOND CHF and MI trials examined mortality in patients with structural heart disease (ejection fraction ≤35%). In these large, double-blind studies, deaths occurred in 36% (541/1511) of TIKOSYN patients and 37% (560/1517) of placebo patients. In an analysis of 506 DIAMOND patients with atrial fibrillation/flutter at baseline, one year mortality on TIKOSYN was 31% vs. 32% on placebo (see CLINICAL STUDIES). Because of the small number of events, an excess mortality due to TIKOSYN cannot be ruled out with confidence in the pooled survival analysis of placebo-controlled trials in patients with supraventricular arrhythmias. However, it is reassuring that in two large placebo-controlled mortality studies in patients with significant heart disease (DIAMOND CHF/MI), there were no more deaths in TIKOSYN-treated patients than in patients given placebo (see CLINICAL STUDIES).
Drug-Drug Interactions
(see CONTRAINDICATIONS) Because there is a linear relationship between dofetilide plasma concentration and QTc, concomitant drugs that interfere with the metabolism or renal elimination of dofetilide may increase the risk of arrhythmia(Torsade de Pointes). TIKOSYN is metabolized to a small degree by the CYP3A4 isoenzyme of the cytochrome P450 system and an inhibitor of this system could increase systemic dofetilide exposure. More important, dofetilide is eliminated by cationic renal secretion, and three inhibitors of this process have been shown to increase systemic dofetilide exposure. The magnitude of the effect on renal elimination by cimetidine, trimethoprim, and ketoconazole (all contraindicated concomitant uses with dofetilide) suggests that all renal cation transport inhibitors should be contraindicated.
Hypokalemia and Potassium-Depleting Diuretics
Hypokalemia or hypomagnesemia may occur with administration of potassium-depleting diuretics, increasing the potential for Torsade de Pointes. Potassium levels should be within the normal range prior to administration of TIKOSYN and maintained in the normal range during administration of TIKOSYN (see DOSAGE AND ADMINISTRATION).
Use with Drugs that Prolong QT Interval and Antiarrhythmic Agents
The use of TIKOSYN in conjunction with other drugs that prolong the QT interval has not been studied and is not recommended. Such drugs include phenothiazines, cisapride, bepridil, tricyclic antidepressants, certain oral macrolides, and certain fluoroquinolones. Class I or Class III antiarrhythmic agents should be withheld for at least three half-lives prior to dosing with TIKOSYN. In clinical trials, TIKOSYN was administered to patients previously treated with oral amiodarone only if serum amiodarone levels were below 0.3 mg/L or amiodarone had been withdrawn for at least three months.
Adverse Reactions
Clinical Trials Experience
The TIKOSYN clinical program involved approximately 8,600 patients in 130 clinical studies of normal volunteers and patients with supraventricular and ventricular arrhythmias. TIKOSYN was administered to 5,194 patients, including two large, placebo-controlled mortality trials (DIAMOND CHF and DIAMOND MI) in which 1,511 patients received TIKOSYN for up to three years. In the following section, adverse reaction data for cardiac arrhythmias and non-cardiac adverse reactions are presented separately for patients included in the supraventricular arrhythmia development program and for patients included in the DIAMOND CHF and MI mortality trials (see CLINICAL STUDIES, Safety in Patients with Structural Heart Disease, DIAMOND Studies, for a description of these trials). In studies of patients with supraventricular arrhythmias, a total of 1,346 and 677 patients were exposed to TIKOSYN and placebo for 551 and 207 patient years, respectively. A total of 8.7% of patients in the dofetilide groups were discontinued from clinical trials due to adverse events compared to 8.0% in the placebo groups. The most frequent reason for discontinuation (>1%) was ventricular tachycardia (2.0% on dofetilide vs. 1.3% on placebo). The most frequent adverse events were headache, chest pain, and dizziness .
Serious Arrhythmias and Conduction Disturbances
Torsade de Pointes is the only arrhythmia that showed a dose-response relationship to TIKOSYN treatment. It did not occur in placebo treated patients. The incidence of Torsade de Pointes in patients with supraventricular arrhythmias was 0.8% (11/1346) (see WARNINGS). The incidence of Torsade de Pointes in patients who were dosed according to the recommended dosing regimen (see DOSAGE AND ADMINISTRATION) was 0.8% (4/525). Table 6 shows the frequency by randomized dose of serious arrhythmias and conduction disturbances reported as adverse events in patients with supraventricular arrhythmias.

In the DIAMOND trials, a total of 1,511 patients were exposed to TIKOSYN for 1757 patient years. The incidence of Torsade de Pointes was 3.3% in CHF patients and 0.9% in patients with a recent MI. Table 7 shows the incidence of serious arrhythmias and conduction disturbances reported as adverse events in the DIAMOND subpopulation that had AF at entry to these trials.

Other Adverse Reactions
Table 8 presents other adverse events reported with a frequency of >2% on TIKOSYN and reported numerically more frequently on TIKOSYN than on placebo in the studies of patients with supraventricular arrhythmias.

Adverse events reported at a rate >2% but no more frequently on TIKOSYN than on placebo were: angina pectoris, anxiety, arthralgia, asthenia, atrial fibrillation, complications (application, injection, incision, insertion, or device), hypertension, pain, palpitation, peripheral edema, supraventricular tachycardia, sweating, urinary tract infection, ventricular tachycardia. The following adverse events have been reported with a frequency of ≤2% and numerically more frequently with TIKOSYN than placebo in patients with supraventricular arrhythmias: angioedema, bradycardia, cerebral ischemia, cerebrovascular accident, edema, facial paralysis, flaccid paralysis, heart arrest, increased cough, liver damage, migraine, myocardial infarct, paralysis, paresthesia, sudden death, and syncope. The incidences of clinically significant laboratory test abnormalities in patients with supraventricular arrhythmias were similar for patients on TIKOSYN and those on placebo. No clinically relevant effects were noted in serum alkaline phosphatase, serum GGT, LDH, AST, ALT, total bilirubin, total protein, blood urea nitrogen, creatinine, serum electrolytes (calcium, chloride, glucose, magnesium, potassium, sodium), or creatine kinase. Similarly, no clinically relevant effects were observed in hematologic parameters. In the DIAMOND population, adverse events other than those related to the post-infarction and heart failure patient population were generally similar to those seen in the supraventricular arrhythmia groups.
Postmarketing Experience
There is limited information regarding Dofetilide Postmarketing Experience in the drug label.
Drug Interactions
Cimetidine
(see WARNINGS, CONTRAINDICATIONS) Concomitant use of cimetidine is contraindicated. cimetidine at 400 mg BID (the usual prescription dose) co-administered with TIKOSYN (500 mcg BID) for 7 days has been shown to increase dofetilide plasma levels by 58%. cimetidine at doses of 100 mg BID (OTC dose) resulted in a 13% increase in dofetilide plasma levels (500 mcg single dose). No studies have been conducted at intermediate doses of cimetidine. If a patient requires TIKOSYN and anti-ulcer therapy, it is suggested that omeprazole, ranitidine, or antacids (aluminum and magnesium hydroxides) be used as alternatives to cimetidine, as these agents have no effect on the pharmacokinetic profile of TIKOSYN.
Verapamil
(see CONTRAINDICATIONS) Concomitant use of verapamil is contraindicated. Co-administration of TIKOSYN with verapamil resulted in increases in dofetilide peak plasma levels of 42%, although overall exposure to dofetilide was not significantly increased. In an analysis of the supraventricular arrhythmia and DIAMOND patient populations, the concomitant administration of verapamil with dofetilide was associated with a higher occurrence of Torsade de Pointes.
Ketoconazole
(see WARNINGS, CONTRAINDICATIONS) Concomitant use of ketoconazoleis contraindicated. ketoconazoleat 400 mg daily (the maximum approved prescription dose) co-administered with TIKOSYN (500 mcg BID) for 7 days has been shown to increase dofetilide Cmax by 53% in males and 97% in females, and AUC by 41% in males and 69% in females.
trimethoprimAlone or in Combination with Sulfamethoxazole
(see WARNINGS, CONTRAINDICATIONS) Concomitant use of trimethoprimalone or in combination with sulfamethoxazole is contraindicated. trimethoprim160 mg in combination with 800 mg sulfamethoxazole co-administered BID with TIKOSYN (500 mcg BID) for 4 days has been shown to increase dofetilide AUC by 103% and Cmax by 93%.
Hydrochlorothiazide (HCTZ) Alone or in Combination with Triamterene
(see CONTRAINDICATIONS) Concomitant use of HCTZ alone or in combination with triamtereneis contraindicated. HCTZ 50 mg QD or HCTZ/triamterene50/100 mg QD was co-administered with TIKOSYN (500 mcg BID) for 5 days (following 2 days of diuretic use at half dose). In patients receiving HCTZ alone, dofetilide AUC increased by 27% and Cmax by 21%. However, the pharmacodynamic effect increased by 197% (QTc increase over time) and by 95% (maximum QTc increase). In patients receiving HCTZ in combination with triamterene, dofetilide AUC increased by 30% and Cmax by 16%. However, the pharmacodynamic effect increased by 190% (QTc increase over time) and by 84% (maximum QTc increase). The pharmacodynamic effects can be explained by a combination of the increase in dofetilide exposure and the reductions in serum potassium. In the DIAMOND trials, 1252 patients were treated with TIKOSYN and diuretics concomitantly, of whom 493 died compared to 508 deaths among the 1248 patients receiving placebo and diuretics. Of the 229 patients who had potassium depleting diuretics added to their concomitant medications in the DIAMOND trials, the patients on TIKOSYN had a non-significantly reduced relative risk for death of 0.68 (95% CI: 0.376, 1.230).
Potential Drug Interactions
Dofetilide is eliminated in the kidney by cationic secretion. Inhibitors of renal cationic secretion are contraindicated with TIKOSYN. In addition, drugs that are actively secreted via this route (e.g., triamterene, metformin, and amiloride) should be co-administered with care as they might increase dofetilide levels. Dofetilide is metabolized to a small extent by the CYP3A4 isoenzyme of the cytochromeP450 system. Inhibitors of the CYP3A4 isoenzyme could increase systemic dofetilide exposure. Inhibitors of this isoenzyme (e.g., macrolide antibiotics, azole antifungal agents, protease inhibitors, serotonin reuptake inhibitors, amiodarone, cannabinoids, diltiazem, grapefruit juice, nefazadone, norfloxacin, quinine, zafirlukast) should be cautiously co-administered with TIKOSYN as they can potentially increase dofetilide levels. Dofetilide is not an inhibitor of CYP3A4 nor of other cytochromeP450 isoenzymes (e.g., CYP2C9, CYP2D6) and is not expected to increase levels of drugs metabolized by CYP3A4.
Other Drug Interaction Information
Digoxin
Studies in healthy volunteers have shown that TIKOSYN does not affect the pharmacokinetics of digoxin. In patients, the concomitant administration of digoxin with dofetilide was associated with a higher occurrence of Torsade de Pointes. It is not clear whether this represents an interaction with TIKOSYN or the presence of more severe structural heart disease in patients on digoxin; structural heart disease is a known risk factor for arrhythmia. No increase in mortality was observed in patients taking digoxin as concomitant medication.
Other Drugs
In healthy volunteers, amlodipine, phenytoin, glyburide, ranitidine, omeprazole, hormone replacement therapy (a combination of conjugated estrogens and medroxyprogesterone), antacid (aluminum and magnesium hydroxides), and theophylline did not affect the pharmacokinetics of TIKOSYN. In addition, studies in healthy volunteers have shown that TIKOSYN does not affect the pharmacokinetics or pharmacodynamics of warfarin, or the pharmacokinetics of propranolol (40 mg twice daily), phenytoin, theophylline, or oral contraceptives. Population pharmacokinetic analyses were conducted on plasma concentration data from 1445 patients in clinical trials to examine the effects of concomitant medications on clearance or volume of distribution of dofetilide. Concomitant medications were grouped as ACE inhibitors, oral anticoagulants, calcium channel blockers, beta blockers, cardiac glycosides, inducers of CYP3A4, substrates and inhibitors of CYP3A4, substrates and inhibitors of P-glycoprotein, nitrates, sulphonylureas, loop diuretics, potassium sparing diuretics, thiazide diuretics, substrates and inhibitors of tubular organic cation transport, and QTc-prolonging drugs. Differences in clearance between patients on these medications (at any occasion in the study) and those off medications varied between -16% and +3%. The mean clearances of dofetilide were 16% and 15% lower in patients on thiazide diuretics and inhibitors of tubular organic cation transport, respectively.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
Dofetilide had no genotoxic effects, with or without metabolic activation, based on the bacterial mutation assay and tests of cytogenetic aberrations in vivo in mouse bone marrow and in vitro in human lymphocytes. Rats and mice treated with dofetilide in the diet for two years showed no evidence of an increased incidence of tumors compared to controls. The highest dofetilide dose administered for 24 months was 10 mg/kg/day to rats and 20 mg/kg/day to mice. Mean dofetilide AUCs(0–24hr) at these doses were about 26 and 10 times, respectively, the maximum likely human AUC.
There was no effect on mating or fertility when dofetilide was administered to male and female rats at doses as high as 1.0 mg/kg/day, a dose that would be expected to provide a mean dofetilide AUC(0–24hr) about 3 times the maximum likely human AUC. Increased incidences of testicular atrophy and epididymal oligospermia and a reduction in testicular weight were, however, observed in other studies in rats. Reduced testicular weight and increased incidence of testicular atrophy were also consistent findings in dogs and mice. The no effect doses for these findings in chronic administration studies in these 3 species (3, 0.1, and 6 mg/kg/day) were associated with mean dofetilide AUCs that were about 4, 1.3, and 3 times the maximum likely human AUC, respectively.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Dofetilide in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Dofetilide during labor and delivery.
Nursing Mothers
There is no information on the presence of dofetilide in breast milk. Patients should be advised not to breast-feed an infant if they are taking TIKOSYN.
Pediatric Use
The safety and effectiveness of TIKOSYN in children (<18 years old) has not been established.
Geriatic Use
Of the total number of patients in clinical studies of TIKOSYN, 46% were 65 to 89 years old. No overall differences in safety, effect on QTc, or effectiveness were observed between elderly and younger patients. Because elderly patients are more likely to have decreased renal function with a reduced creatinine clearance, care must be taken in dose selection (see DOSAGE AND ADMINISTRATION).
Gender
Female patients constituted 32% of the patients in the placebo-controlled trials of TIKOSYN. As with other drugs that cause Torsade de Pointes, TIKOSYN was associated with a greater risk of Torsade de Pointes in female patients than in male patients. During the TIKOSYN clinical development program, the risk of Torsade de Pointes in females was approximately 3 times the risk in males. Unlike Torsade de Pointes, the incidence of other ventricular arrhythmias was similar in female patients receiving TIKOSYN and patients receiving placebo. Although no study specifically investigated this risk, in post-hoc analyses, no increased mortality was observed in females on TIKOSYN compared to females on placebo.
Race
There is no FDA guidance on the use of Dofetilide with respect to specific racial populations.
Renal Impairment
The overall systemic clearance of dofetilide is decreased and plasma concentration increased with decreasing creatinine clearance. The dose of TIKOSYN must be adjusted based on creatinine clearance (see DOSAGE AND ADMINISTRATION). Patients undergoing dialysis were not included in clinical studies, and appropriate dosing recommendations for these patients are unknown. There is no information about the effectiveness of hemodialysis in removing dofetilide from plasma.
Hepatic Impairment
After adjustment for creatinine clearance, no additional dose adjustment is required for patients with mild or moderate hepatic impairment. Patients with severe hepatic impairment have not been studied. TIKOSYN should be used with particular caution in these patients.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Dofetilide in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Dofetilide in patients who are immunocompromised.
Cardiac Conduction Disturbances
Animal and human studies have not shown any adverse effects of dofetilide on conduction velocity. No effect on AV nodal conduction following TIKOSYN treatment was noted in normal volunteers and in patients with 1st degree heart block. Patients with sick sinus syndrome or with 2nd or 3rd degree heart block were not included in the Phase 3 clinical trials unless a functioning pacemaker was present. TIKOSYN has been used safely in conjunction with pacemakers (53 patients in DIAMOND studies, 136 in trials in patients with ventricular and supraventricular arrhythmias).
Administration and Monitoring
Administration
- Therapy with TIKOSYN must be initiated (and, if necessary, re-initiated) in a setting that provides continuous electrocardiographic (ECG) monitoring and in the presence of personnel trained in the management of serious ventricular arrhythmias. Patients should continue to be monitored in this way for a minimum of three days. Additionally, patients should not be discharged within 12 hours of electrical or pharmacological conversion to normal sinus rhythm.
- The dose of TIKOSYN must be individualized according to calculated creatinine clearance and QTc. (QT interval should be used if the heart rate is <60 beats per minute. There are no data on use of TIKOSYN when the heart rate is <50 beats per minute.) The usual recommended dose of TIKOSYN is 500 mcg BID, as modified by the dosing algorithm described below. For consideration of a lower dose, see Special Considerations below.
- Serum potassium should be maintained within the normal range before TIKOSYN treatment is initiated and should be maintained within the normal range while the patient remains on TIKOSYN therapy. (See WARNINGS, Hypokalemia and Potassium-Depleting Diuretics). In clinical trials, potassium levels were generally maintained above 3.6–4.0 mEq/L.
- Patients with atrial fibrillation should be anticoagulated according to usual medical practice prior to electrical or pharmacological cardioversion. Anticoagulant therapy may be continued after cardioversion according to usual medical practice for the treatment of people with AF. Hypokalemia should be corrected before initiation of TIKOSYN therapy (see WARNINGS, Ventricular Arrhythmia).
- Patients to be discharged on TIKOSYN therapy from an inpatient setting as described above must have an adequate supply of TIKOSYN, at the patient's individualized dose, to allow uninterrupted dosing until the patient receives the first outpatient supply.
- TIKOSYN is distributed only to those hospitals and other appropriate institutions confirmed to have received applicable dosing and treatment initiation education programs. Inpatient and subsequent outpatient discharge and refill prescriptions are filled only upon confirmation that the prescribing physician has received applicable dosing and treatment initiation education programs. For this purpose, a list for use by pharmacists is maintained containing hospitals and physicians who have received one of the education programs.
Instructions for Individualized Dose Initiation
Initiation of TIKOSYN Therapy
Step 1. Electrocardiographic assessment: Prior to administration of the first dose, the QTc must be determined using an average of 5–10 beats. If the QTc is greater than 440 msec (500 msec in patients with ventricular conduction abnormalities), TIKOSYN is contraindicated. If heart rate is less than 60 beats per minute, QT interval should be used. Patients with heart rates <50 beats per minute have not been studied. Step 2. Calculation of creatinine clearance: Prior to the administration of the first dose, the patient's creatinine clearance must be calculated using the following formula:

When serum creatinine is given in µmol/L, divide the value by 88.4 (1 mg/dL = 88.4 µmol/L). Step 3. Starting Dose: The starting dose of TIKOSYN is determined as follows:

Step 4. Administer the adjusted TIKOSYN dose and begin continuous ECG monitoring. Step 5. At 2–3 hours after administering the first dose of TIKOSYN, determine the QTc. If the QTc has increased by greater than 15% compared to the baseline established in Step 1 OR if the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), subsequent dosing should be adjusted as follows:

Step 6. At 2–3 hours after each subsequent dose of TIKOSYN, determine the QTc (for in-hospital doses 2–5). No further down titration of TIKOSYN based on QTc is recommended. NOTE: If at any time after the second dose of TIKOSYN is given the QTc is greater than 500 msec (550 msec in patients with ventricular conduction abnormalities), TIKOSYN should be discontinued. Step 7. Patients are to be continuously monitored by ECG for a minimum of three days, or for a minimum of 12 hours after electrical or pharmacological conversion to normal sinus rhythm, whichever is greater. The steps described above are summarized in the following diagram:
Maintenance of TIKOSYN Therapy
Renal function and QTc should be re-evaluated every three months or as medically warranted. If QTc exceeds 500 milliseconds (550 msec in patients with ventricular conduction abnormalities), TIKOSYN therapy should be discontinued and patients should be carefully monitored until QTc returns to baseline levels. If renal function deteriorates, adjust dose as described in Initiation of TIKOSYN Therapy, Step 3.
Special Considerations
Consideration of a Dose Lower than that Determined by the Algorithm The dosing algorithm shown above should be used to determine the individualized dose of TIKOSYN. In clinical trials (see CLINICAL STUDIES), the highest dose of 500 mcg BID of TIKOSYN as modified by the dosing algorithm led to greater effectiveness than lower doses of 125 or 250 mcg BID as modified by the dosing algorithm. The risk of Torsade de Pointes, however, is related to dose as well as to patient characteristics (see WARNINGS). Physicians, in consultation with their patients, may therefore in some cases choose doses lower than determined by the algorithm. It is critically important that if at any time this lower dose is increased, the patient needs to be rehospitalized for three days. Previous toleration of higher doses does not eliminate the need for rehospitalization. The maximum recommended dose in patients with a calculated creatinine clearance greater than 60 mL/min is 500 mcg BID; doses greater than 500 mcg BID have been associated with an increased incidence of Torsade de Pointes. A patient who misses a dose should NOT double the next dose. The next dose should be taken at the usual time.
Cardioversion
If patients do not convert to normal sinus rhythm within 24 hours of initiation of TIKOSYN therapy, electrical conversion should be considered. Patients continuing on TIKOSYN after successful electrical cardioversion should continue to be monitored by electrocardiography for 12 hours post cardioversion, or a minimum of 3 days after initiation of TIKOSYN therapy, whichever is greater.
Switch to TIKOSYN from Class I or other Class III Antiarrhythmic Therapy' Before initiating TIKOSYN therapy, previous antiarrhythmic therapy should be withdrawn under careful monitoring for a minimum of three (3) plasma half-lives. Because of the unpredictable pharmacokinetics of amiodarone, TIKOSYN should not be initiated following amiodarone therapy until amiodarone plasma levels are below 0.3 mcg/mL or until amiodarone has been withdrawn for at least three months. Stopping TIKOSYN Prior to Administration of Potentially Interacting Drugs If TIKOSYN needs to be discontinued to allow dosing of other potentially interacting drug(s), a washout period of at least two days should be followed before starting the other drug(s).
Monitoring
There is limited information regarding Dofetilide Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Dofetilide and IV administrations.
Overdosage
There is limited information regarding Dofetilide overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
There is limited information regarding Dofetilide Pharmacology in the drug label.
Mechanism of Action
There is limited information regarding Dofetilide Mechanism of Action in the drug label.
Structure
There is limited information regarding Dofetilide Structure in the drug label.
Pharmacodynamics
There is limited information regarding Dofetilide Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Dofetilide Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Dofetilide Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Dofetilide Clinical Studies in the drug label.
How Supplied
There is limited information regarding Dofetilide How Supplied in the drug label.
Storage
There is limited information regarding Dofetilide Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Dofetilide |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Dofetilide |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Dofetilide Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Dofetilide interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Dofetilide Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Dofetilide Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
 | |
| Clinical data | |
|---|---|
| ATC code | |
| Pharmacokinetic data | |
| Bioavailability | 96% (oral) |
| Protein binding | 60% -70% |
| Elimination half-life | 10 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C19H27N3O5S2 |
| Molar mass | 441.567 g/mol |
|
WikiDoc Resources for Dofetilide |
|
Articles |
|---|
|
Most recent articles on Dofetilide |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Dofetilide at Clinical Trials.gov Clinical Trials on Dofetilide at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Dofetilide
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Dofetilide Discussion groups on Dofetilide Patient Handouts on Dofetilide Directions to Hospitals Treating Dofetilide Risk calculators and risk factors for Dofetilide
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Dofetilide |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]
For patient information, click here
Dofetilide is a class III antiarrhythmic agent that is approved by the Food and Drug Administration (FDA) for the maintenance of sinus rhythm in individuals prone to the formation of atrial fibrillation and flutter, and for the chemical cardioversion to sinus rhythm from atrial fibrillation and flutter.
The chemical name for dofetilide is N-[4-(2-{2-[4-(methanesulphonamido) phenoxyl]-N-methylethylamino}ethyl)phenyl]- methanesulphonamide. It is marketed under the trade name Tikosyn® by Pfizer, and is available in the United States in capsules containing 125, 250, and 500 µg of dofetilide. Due to the pro-arrhythmic potential of dofetilide, it is only available by prescription by physicians who have undergone specific training in the risks of treatment with dofetilide. In addition, it is only available by mail order or through specially trained local pharmacies to individuals who are prescribed dofetilide by a physician who is registered as being able to prescribe the pharmaceutical.
The elimination half-life of dofetilide is roughly 10 hours, however this is variable based on many physiologic factors (most significantly creatinine clearance), and ranges from 4.8 to 13.5 hours.
Mechanism of action
Dofetilide works by selectively blocking the rapid component of the delayed rectifier outward potassium current (IKr).
This causes prolongation of the effective refractory period of accessory pathways (both anterograde and retrograde conduction in the accessory pathway). It is this selective action on accessory pathways that makes dofetilide effective in the treatment of atrial fibrillation and flutter.
Dofetilide does not effect Vmax (The slope of the upstroke of phase 0 depolarization), conduction velocity, or the resting membrane potential.
There is a dose-dependent increase in the QT interval and the corrected QT interval (QTc). Because of this, many practitioners will initiate dofetilide therapy only on individuals under telemetry monitoring or if serial EKG measurements of QT and QTc can be performed.
Metabolism
A steady-state plasma level of dofetilide is achieved in 2-3 days.
80% of dofetilide is excreted by the kidneys, so the dose of dofetilide should be adjusted in individuals with renal insufficiency, based on creatinine clearance.
In the kidneys, dofetilide is eliminated via cation exchange (secretion). Agents that interfere with the renal cation exchange system, such as verapamil, cimetidine, hydrochlorothiazide, itraconazole, ketoconazole, prochlorperazine, and trimethoprim should not be administered to individuals taking dofetilide.
About 20 percent of dofetilide is metabolized in the liver via the CYP3A4 isoenzyme of the cytochrome P450 enzyme system. Drugs that interfere with the activity of the CYP3A4 isoenzyme can increase serum dofetilide levels. If the renal cation exchange system is interfered with (as with the medications listed above), a larger percentage of dofetilide is cleared via the CYP3A4 isoenzyme system.
Side effects
Torsades de pointes is the most serious side effect of dofetilide therapy. The incidence of torsades de pointes is dose-related, and is 0.3-10.5%. The risk appears to be dose-dependent, with an increased incidence of torsades de pointes associated with higher doses of dofetilide administered.
The risk of inducing torsades de pointes can be decreased by taking precautions when initiating therapy, such as hospitalizing individuals for a minimum of three days for serial creatinine measurement, continuous telemetry monitoring and availability of cardiac resuscitation.
Clinical use
Based on the results of the Danish Investigations of Arrhythmias and Mortality on Dofetilide (DIAMOND) study, dofetilide does not affect mortality in the treatment of patients post-myocardial infarction with left ventricular dysfunction.3 Because of the results of the DIAMOND study, many physicians use dofetilide in the suppression of atrial fibrillation in individuals with LV dysfunction.
See also
References
- Thomas L. Lenz, Pharm.D., and Daniel E. Hilleman, Pharm.D., Department of Cardiology, Creighton University, Omaha, Nebraska. Dofetilide, a New Class III Antiarrhythmic Agent. Pharmacotherapy 20(7):776-786, 2000. (Medline abstract)
- Lenz TL, Hilleman DE. Dofetilide: A new antiarrhythmic agent approved for conversion and/or maintenance of atrial fibrillation/atrial flutter. Drugs Today (Barc). 2000 Nov;36(11):759-71. (Medline abstract)
- Torp-Pedersen C, Moller M, Bloch-Thomsen PE, Kober L, Sandoe E, Egstrup K, Agner E, Carlsen J, Videbaek J, Marchant B, Camm AJ. Dofetilide in patients with congestive heart failure and left ventricular dysfunction. Danish Investigations of Arrhythmia and Mortality on Dofetilide Study Group. N Engl J Med. 1999 Sep 16;341(12):857-65. (Medline abstract)
- Pages with script errors
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs with no legal status
- Articles containing unverified chemical infoboxes
- Antiarrhythmic agents
- Drugs