Dermatofibroma pathophysiology: Difference between revisions
Homa Najafi (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by 2 users not shown) | |||
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
The exact pathogenesis of | The exact pathogenesis of dermatofibroma is not fully understood. Although some mechanisms are suggested in the [[pathogenesis]] of this disease that include, reactive [[tissue]] changes, [[neoplastic]] [[proliferation]], the cell surface [[proteoglycan]], [[Syndecan 1|syndecan-1]], and [[fibroblast growth factor receptor 2]] may play a role in the [[growth]] of dermatofibromas, [[Transforming growth factor-β|transforming growth factor-beta]] ([[TGF-beta]]) [[Signaling pathway|signaling]] may be involved in the [[development]] of [[fibrosis]] in [[dermatofibroma]], and the presence of [[Factor XIII|factor XIIIa]] and [[CD]]168 suggests that dermatofibroma can originate from the [[dermal]] [[dendritic cell]]. On [[gross pathology]], firm yellowish [[papules]] which may have areas of [[hemorrhage]] and lipidization are characteristic findings of dermatofibroma. Microscopically dermatofibroma is characterized by localized [[nodular]] [[proliferation]] of [[spindle]]-shaped [[fibrous]] [[Cells (biology)|cells]] in a [[mixture]] of [[Histiocyte|histocytoid]] [[Cells (biology)|cells]] inside the [[dermis]], spiculated margin of cells, “Storiform” [[pattern]] which defines as whorls of elongated [[nuclei]], [[collagen]] bundles that usually seen inside and between the [[fascicles]] of [[Spindle|spindled]] [[fibrous]] [[cells]], "Grenz zone" which is an unaffected layer that separates the overlying [[epidermis]] from the [[dermis]], and [[epidermal]] [[hyperplasia]]. | ||
[ | |||
[ | |||
==Pathophysiology== | ==Pathophysiology== | ||
===Pathogenesis=== | ===Pathogenesis=== | ||
*The exact | *The exact [[pathogenesis]] of dermatofibroma is not completely understood. | ||
*The mechanisms which are suggested in the [[pathogenesis]] of dermatofibroma include:<ref name="pmid10660130">{{cite journal| author=Chen TC, Kuo T, Chan HL| title=Dermatofibroma is a clonal proliferative disease. | journal=J Cutan Pathol | year= 2000 | volume= 27 | issue= 1 | pages= 36-9 | pmid=10660130 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10660130 }} </ref><ref name="pmid14501288">{{cite journal| author=Sellheyer K, Smoller BR| title=Dermatofibroma: upregulation of syndecan-1 expression in mesenchymal tissue. | journal=Am J Dermatopathol | year= 2003 | volume= 25 | issue= 5 | pages= 392-8 | pmid=14501288 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14501288 }} </ref><ref name="SkrozaRotolo2008">{{cite journal|last1=Skroza|first1=Nevena|last2=Rotolo|first2=Sabrina|last3=Ceccarelli|first3=Simona|last4=Romano|first4=Ferdinando|last5=Innocenzi|first5=Daniele|last6=Frati|first6=Luigi|last7=Angeloni|first7=Antonio|last8=Marchese|first8=Cinzia|title=Modulation of the expression of the FGFR2-IIIb and FGFR2-IIIc molecules in dermatofibroma|journal=Journal of Dermatological Science|volume=51|issue=1|year=2008|pages=53–57|issn=09231811|doi=10.1016/j.jdermsci.2008.02.004}}</ref><ref name="KuboIhn2006">{{cite journal|last1=Kubo|first1=M.|last2=Ihn|first2=H.|last3=Yamane|first3=K.|last4=Tamaki|first4=K.|title=The expression levels and the differential expression of transforming growth factor-beta receptors in dermatofibroma and dermatofibrosarcoma protuberans|journal=British Journal of Dermatology|volume=154|issue=5|year=2006|pages=919–925|issn=0007-0963|doi=10.1111/j.1365-2133.2005.06904.x}}</ref><ref name="CerioSpaull2006">{{cite journal|last1=Cerio|first1=R.|last2=Spaull|first2=J.|last3=Jones|first3=E.Wilson|title=Histiocytoma cutis: a tumour of dermal dendrocytes (dermal dendrocytoma)|journal=British Journal of Dermatology|volume=120|issue=2|year=2006|pages=197–206|issn=00070963|doi=10.1111/j.1365-2133.1989.tb07783.x}}</ref><ref name="TörőcsikBárdos2005">{{cite journal|last1=Törőcsik|first1=D.|last2=Bárdos|first2=H.|last3=Nagy|first3=L.|last4=Ádány|first4=R.|title=Identification of factor XIII-A as a marker of alternative macrophage activation|journal=Cellular and Molecular Life Sciences|volume=62|issue=18|year=2005|pages=2132–2139|issn=1420-682X|doi=10.1007/s00018-005-5242-9}}</ref><ref name="pmid1972317">{{cite journal| author=Cerio R, Spaull J, Oliver GF, Jones WE| title=A study of factor XIIIa and MAC 387 immunolabeling in normal and pathological skin. | journal=Am J Dermatopathol | year= 1990 | volume= 12 | issue= 3 | pages= 221-33 | pmid=1972317 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1972317 }} </ref> | |||
**Reactive [[tissue]] changes | |||
**[[Neoplastic]] [[proliferation]] because of the [[clonality]] | |||
**The cell surface [[proteoglycan]], [[Syndecan 1|syndecan-1]], and [[fibroblast growth factor receptor 2]] may play a role in the [[growth]] of dermatofibromas. | |||
**[[Transforming growth factor-β|Transforming growth factor-beta]] ([[TGF-beta]]) [[Signaling pathway|signaling]] may be involved in the [[development]] of [[fibrosis]] in [[dermatofibroma]] | |||
**The presence of [[Factor XIII|factor XIIIa]] and [[CD]]168 suggests that dermatofibroma can originate from the [[dermal]] [[dendritic cell]]. | |||
the | |||
and | |||
of | |||
of | |||
of the | |||
in the | |||
the | |||
==Genetics== | ==Genetics== | ||
| Line 272: | Line 30: | ||
| pages = 901–903 | | pages = 901–903 | ||
| year = 1995 | | year = 1995 | ||
| doi = 10.1016/0190-9622(95)91558-3 | | doi = 10.1016/0190-9622(95)91558-3 | ||
| pmid = 7722054 | | pmid = 7722054 | ||
| Line 283: | Line 40: | ||
| pages = 266–270 | | pages = 266–270 | ||
| year = 1991 | | year = 1991 | ||
| pmid = 2050454 | | pmid = 2050454 | ||
}}</ref><ref>{{Cite journal | }}</ref><ref>{{Cite journal | ||
| Line 293: | Line 49: | ||
| pages = 1074–1076 | | pages = 1074–1076 | ||
| year = 2017 | | year = 2017 | ||
| doi = 10.1111/1346-8138.13625 | | doi = 10.1111/1346-8138.13625 | ||
| pmid = 27665731 | | pmid = 27665731 | ||
| Line 304: | Line 59: | ||
| pages = 59–60 | | pages = 59–60 | ||
| year = 1994 | | year = 1994 | ||
| pmid = 8313640 | | pmid = 8313640 | ||
}}</ref><ref>{{Cite journal | }}</ref><ref>{{Cite journal | ||
| Line 314: | Line 68: | ||
| pages = 319–321 | | pages = 319–321 | ||
| year = 2003 | | year = 2003 | ||
| doi = 10.1159/000073098 | | doi = 10.1159/000073098 | ||
| pmid = 14571078 | | pmid = 14571078 | ||
| Line 325: | Line 78: | ||
| pages = 351–352 | | pages = 351–352 | ||
| year = 1986 | | year = 1986 | ||
| doi = 10.1016/s0190-9622(86)70041-8 | | doi = 10.1016/s0190-9622(86)70041-8 | ||
| pmid = 3950136 | | pmid = 3950136 | ||
| Line 336: | Line 88: | ||
| pages = 1062–1063 | | pages = 1062–1063 | ||
| year = 2000 | | year = 2000 | ||
| doi = 10.1046/j.1365-2133.2000.03508.x | | doi = 10.1046/j.1365-2133.2000.03508.x | ||
| pmid = 10809884 | | pmid = 10809884 | ||
| Line 346: | Line 97: | ||
*[[Hematologic]] [[malignancies]] | *[[Hematologic]] [[malignancies]] | ||
*[[Immunodeficiency|Immunodeficient]] [[Disease|diseases]] ([[HIV]]) | *[[Immunodeficiency|Immunodeficient]] [[Disease|diseases]] ([[HIV]]) | ||
*[[Autoimmune diseases]] ([[myasthenia gravis]], [[ | *[[Autoimmune diseases]] ([[myasthenia gravis]], [[pemphigus vulgaris]], and [[systemic lupus erythematosus]]) | ||
==Gross Pathology== | ==Gross Pathology== | ||
| Line 352: | Line 103: | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
Microscopically dermatofibroma is characterized by: <ref name="LeeLee2015">{{cite journal|last1=Lee|first1=MiWoo|last2=Lee|first2=WooJin|last3=Jung|first3=JoonMin|last4=Won|first4=ChongHyun|last5=Chang|first5=SungEun|last6=Choi|first6=JeeHo|last7=Moon|first7=KeeChan|title=Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma|journal=Indian Journal of Dermatology, Venereology, and Leprology|volume=81|issue=3|year=2015|pages=263|issn=0378-6323|doi=10.4103/0378-6323.154795}}</ref><ref name="MentzelWiesner2012">{{cite journal|last1=Mentzel|first1=Thomas|last2=Wiesner|first2=Thomas|last3=Cerroni|first3=Lorenzo|last4=Hantschke|first4=Markus|last5=Kutzner|first5=Heinz|last6=Rütten|first6=Arno|last7=Häberle|first7=Michael|last8=Bisceglia|first8=Michele|last9=Chibon|first9=Frederic|last10=Coindre|first10=Jean-Michel|title=Malignant dermatofibroma: clinicopathological, immunohistochemical, and molecular analysis of seven cases|journal=Modern Pathology|volume=26|issue=2|year=2012|pages=256–267|issn=0893-3952|doi=10.1038/modpathol.2012.157}}</ref> | Microscopically dermatofibroma is characterized by: <ref name="LeeLee2015">{{cite journal|last1=Lee|first1=MiWoo|last2=Lee|first2=WooJin|last3=Jung|first3=JoonMin|last4=Won|first4=ChongHyun|last5=Chang|first5=SungEun|last6=Choi|first6=JeeHo|last7=Moon|first7=KeeChan|title=Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma|journal=Indian Journal of Dermatology, Venereology, and Leprology|volume=81|issue=3|year=2015|pages=263|issn=0378-6323|doi=10.4103/0378-6323.154795}}</ref><ref name="MentzelWiesner2012">{{cite journal|last1=Mentzel|first1=Thomas|last2=Wiesner|first2=Thomas|last3=Cerroni|first3=Lorenzo|last4=Hantschke|first4=Markus|last5=Kutzner|first5=Heinz|last6=Rütten|first6=Arno|last7=Häberle|first7=Michael|last8=Bisceglia|first8=Michele|last9=Chibon|first9=Frederic|last10=Coindre|first10=Jean-Michel|title=Malignant dermatofibroma: clinicopathological, immunohistochemical, and molecular analysis of seven cases|journal=Modern Pathology|volume=26|issue=2|year=2012|pages=256–267|issn=0893-3952|doi=10.1038/modpathol.2012.157}}</ref><ref name="Victor2003">{{cite journal|last1=Victor|first1=Thomas A.|title=Neoplasms With Follicular Differentiation, 2nd ed. A. BERNARD ACKERMAN, VIJAYA B. REDDY, AND H. PETER SOYER, eds.|journal=Dermatologic Surgery|volume=29|issue=6|year=2003|pages=641–641|issn=1076-0512|doi=10.1046/j.1524-4725.2003.29153.x}}</ref> | ||
* Localized [[nodular]] [[proliferation]] of [[spindle]]-shaped [[fibrous]] [[Cells (biology)|cells]] in a [[mixture]] of [[Histiocyte|histocytoid]] [[Cells (biology)|cells]] inside the [[dermis]] | * Localized [[nodular]] [[proliferation]] of [[spindle]]-shaped [[fibrous]] [[Cells (biology)|cells]] in a [[mixture]] of [[Histiocyte|histocytoid]] [[Cells (biology)|cells]] inside the [[dermis]] | ||
* Spiculated margin of cells | * Spiculated margin of cells | ||
| Line 358: | Line 109: | ||
*[[Collagen]] bundles that usually seen inside and between the [[fascicles]] of [[Spindle|spindled]] [[fibrous]] [[cells]] | *[[Collagen]] bundles that usually seen inside and between the [[fascicles]] of [[Spindle|spindled]] [[fibrous]] [[cells]] | ||
* "Grenz zone" which is an unaffected layer that separates the overlying [[epidermis]] from the [[dermis]] | * "Grenz zone" which is an unaffected layer that separates the overlying [[epidermis]] from the [[dermis]] | ||
*[[Epidermal]] [[hyperplasia]] | |||
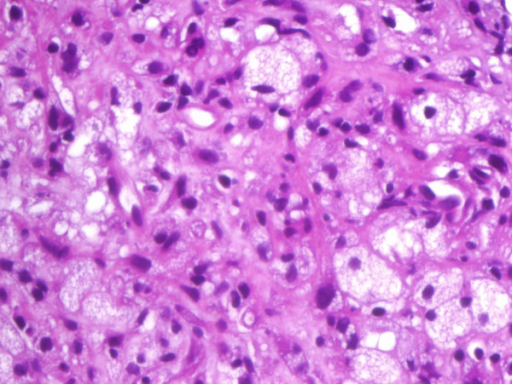
[[File:Proliferating histiocytic cells with foamy, granular cytoplasm.png|350px|thumb|https://openi.nlm.nih.gov/detailedresult?img=PMC3213176_1746-160X-7-20-3&query=&req=4|center]] | |||
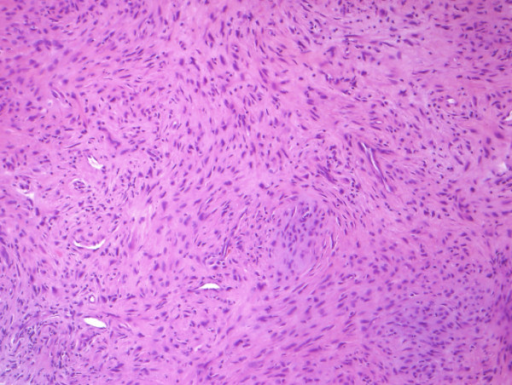
[[File:Spindle-shaped fibroblasts, arranged in a storiform pattern.png|350px|thumb|https://openi.nlm.nih.gov/detailedresult?img=PMC3213176_1746-160X-7-20-3&query=&req=4|center]] | |||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
Latest revision as of 21:18, 29 July 2020
|
Dermatofibroma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dermatofibroma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Dermatofibroma pathophysiology |
|
Risk calculators and risk factors for Dermatofibroma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Associate Editor(s)-in-Chief: Homa Najafi, M.D.[2]Faizan Sheraz, M.D. [3]
Overview
The exact pathogenesis of dermatofibroma is not fully understood. Although some mechanisms are suggested in the pathogenesis of this disease that include, reactive tissue changes, neoplastic proliferation, the cell surface proteoglycan, syndecan-1, and fibroblast growth factor receptor 2 may play a role in the growth of dermatofibromas, transforming growth factor-beta (TGF-beta) signaling may be involved in the development of fibrosis in dermatofibroma, and the presence of factor XIIIa and CD168 suggests that dermatofibroma can originate from the dermal dendritic cell. On gross pathology, firm yellowish papules which may have areas of hemorrhage and lipidization are characteristic findings of dermatofibroma. Microscopically dermatofibroma is characterized by localized nodular proliferation of spindle-shaped fibrous cells in a mixture of histocytoid cells inside the dermis, spiculated margin of cells, “Storiform” pattern which defines as whorls of elongated nuclei, collagen bundles that usually seen inside and between the fascicles of spindled fibrous cells, "Grenz zone" which is an unaffected layer that separates the overlying epidermis from the dermis, and epidermal hyperplasia.
Pathophysiology
Pathogenesis
- The exact pathogenesis of dermatofibroma is not completely understood.
- The mechanisms which are suggested in the pathogenesis of dermatofibroma include:[1][2][3][4][5][6][7]
- Reactive tissue changes
- Neoplastic proliferation because of the clonality
- The cell surface proteoglycan, syndecan-1, and fibroblast growth factor receptor 2 may play a role in the growth of dermatofibromas.
- Transforming growth factor-beta (TGF-beta) signaling may be involved in the development of fibrosis in dermatofibroma
- The presence of factor XIIIa and CD168 suggests that dermatofibroma can originate from the dermal dendritic cell.
Genetics
- There is no genetic alteration involved with pathogenesis of dermatofibroma.
Associated Conditions
Conditions associated with multiple dermatofibromas include:[8][9][10][11][12][13][14][15]
- Pregnancy
- Chromosomal alterations (Down syndrome)
- Metabolic disorders (hypertriglyceridemia)
- Hematologic malignancies
- Immunodeficient diseases (HIV)
- Autoimmune diseases (myasthenia gravis, pemphigus vulgaris, and systemic lupus erythematosus)
Gross Pathology
On gross pathology, firm yellowish papules which may have areas of hemorrhage and lipidization are characteristic findings of dermatofibroma.[16]
Microscopic Pathology
Microscopically dermatofibroma is characterized by: [17][18][19]
- Localized nodular proliferation of spindle-shaped fibrous cells in a mixture of histocytoid cells inside the dermis
- Spiculated margin of cells
- “Storiform” pattern which defines as whorls of elongated nuclei
- Collagen bundles that usually seen inside and between the fascicles of spindled fibrous cells
- "Grenz zone" which is an unaffected layer that separates the overlying epidermis from the dermis
- Epidermal hyperplasia
References
- ↑ Chen TC, Kuo T, Chan HL (2000). "Dermatofibroma is a clonal proliferative disease". J Cutan Pathol. 27 (1): 36–9. PMID 10660130.
- ↑ Sellheyer K, Smoller BR (2003). "Dermatofibroma: upregulation of syndecan-1 expression in mesenchymal tissue". Am J Dermatopathol. 25 (5): 392–8. PMID 14501288.
- ↑ Skroza, Nevena; Rotolo, Sabrina; Ceccarelli, Simona; Romano, Ferdinando; Innocenzi, Daniele; Frati, Luigi; Angeloni, Antonio; Marchese, Cinzia (2008). "Modulation of the expression of the FGFR2-IIIb and FGFR2-IIIc molecules in dermatofibroma". Journal of Dermatological Science. 51 (1): 53–57. doi:10.1016/j.jdermsci.2008.02.004. ISSN 0923-1811.
- ↑ Kubo, M.; Ihn, H.; Yamane, K.; Tamaki, K. (2006). "The expression levels and the differential expression of transforming growth factor-beta receptors in dermatofibroma and dermatofibrosarcoma protuberans". British Journal of Dermatology. 154 (5): 919–925. doi:10.1111/j.1365-2133.2005.06904.x. ISSN 0007-0963.
- ↑ Cerio, R.; Spaull, J.; Jones, E.Wilson (2006). "Histiocytoma cutis: a tumour of dermal dendrocytes (dermal dendrocytoma)". British Journal of Dermatology. 120 (2): 197–206. doi:10.1111/j.1365-2133.1989.tb07783.x. ISSN 0007-0963.
- ↑ Törőcsik, D.; Bárdos, H.; Nagy, L.; Ádány, R. (2005). "Identification of factor XIII-A as a marker of alternative macrophage activation". Cellular and Molecular Life Sciences. 62 (18): 2132–2139. doi:10.1007/s00018-005-5242-9. ISSN 1420-682X.
- ↑ Cerio R, Spaull J, Oliver GF, Jones WE (1990). "A study of factor XIIIa and MAC 387 immunolabeling in normal and pathological skin". Am J Dermatopathol. 12 (3): 221–33. PMID 1972317.
- ↑ Bhattacharjee, Pradip; Umar, Saleem; Fatteh, Shokat (2005). "Multiple Eruptive Dermatofibromas Occurring in a Patient with Myelodysplastic Syndrome". Acta Dermato-Venereologica. -1 (1): 1–1. doi:10.1080/00015550410024517. ISSN 0001-5555.
- ↑ I. Lu, P. R. Cohen & M. E. Grossman (1995). "Multiple dermatofibromas in a woman with HIV infection and systemic lupus erythematosus". Journal of the American Academy of Dermatology. 32 (5 Pt 2): 901–903. doi:10.1016/0190-9622(95)91558-3. PMID 7722054.
- ↑ P. R. Cohen (1991). "Multiple dermatofibromas in patients with autoimmune disorders receiving immunosuppressive therapy". International journal of dermatology. 30 (4): 266–270. PMID 2050454.
- ↑ Mayuri Tanaka, Toshihiko Hoashi, Naotaka Serizawa, Kyochika Okabe, Susumu Ichiyama, Rie Shinohara, Yoko Funasaka & Hidehisa Saeki (2017). "Multiple unilaterally localized dermatofibromas in a patient with Down syndrome". The Journal of dermatology. 44 (9): 1074–1076. doi:10.1111/1346-8138.13625. PMID 27665731.
- ↑ J. Stainforth & M. J. Goodfield (1994). "Multiple dermatofibromata developing during pregnancy". Clinical and experimental dermatology. 19 (1): 59–60. PMID 8313640.
- ↑ Yuichiro Tsunemi, Hironobu Ihn, Naoko Hattori, Hidehisa Saeki & Kunihiko Tamaki (2003). "Multiple eruptive dermatofibromas with CD34+ cells in a patient with hypertriglyceridemia". Dermatology (Basel, Switzerland). 207 (3): 319–321. doi:10.1159/000073098. PMID 14571078.
- ↑ H. B. Bargman & I. Fefferman (1986). "Multiple dermatofibromas in a patient with myasthenia gravis treated with prednisone and cyclophosphamide". Journal of the American Academy of Dermatology. 14 (2 Pt 2): 351–352. doi:10.1016/s0190-9622(86)70041-8. PMID 3950136.
- ↑ S. E. Chang, J. H. Choi, K. J. Sung, K. C. Moon & J. K. Koh (2000). "Multiple eruptive dermatofibromas occurring in a patient with acute myeloid leukaemia". The British journal of dermatology. 142 (5): 1062–1063. doi:10.1046/j.1365-2133.2000.03508.x. PMID 10809884.
- ↑ LeBoit, P. E. (2006). Pathology and genetics of skin tumours. Lyon: IARC Press. ISBN 9283224140.
- ↑ Lee, MiWoo; Lee, WooJin; Jung, JoonMin; Won, ChongHyun; Chang, SungEun; Choi, JeeHo; Moon, KeeChan (2015). "Clinical and histological patterns of dermatofibroma without gross skin surface change: A comparative study with conventional dermatofibroma". Indian Journal of Dermatology, Venereology, and Leprology. 81 (3): 263. doi:10.4103/0378-6323.154795. ISSN 0378-6323.
- ↑ Mentzel, Thomas; Wiesner, Thomas; Cerroni, Lorenzo; Hantschke, Markus; Kutzner, Heinz; Rütten, Arno; Häberle, Michael; Bisceglia, Michele; Chibon, Frederic; Coindre, Jean-Michel (2012). "Malignant dermatofibroma: clinicopathological, immunohistochemical, and molecular analysis of seven cases". Modern Pathology. 26 (2): 256–267. doi:10.1038/modpathol.2012.157. ISSN 0893-3952.
- ↑ Victor, Thomas A. (2003). "Neoplasms With Follicular Differentiation, 2nd ed. A. BERNARD ACKERMAN, VIJAYA B. REDDY, AND H. PETER SOYER, eds". Dermatologic Surgery. 29 (6): 641–641. doi:10.1046/j.1524-4725.2003.29153.x. ISSN 1076-0512.