Clobazam: Difference between revisions
No edit summary |
No edit summary |
||
| (8 intermediate revisions by the same user not shown) | |||
| Line 5: | Line 5: | ||
|drugClass=Benzodiazepine | |drugClass=Benzodiazepine | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=seizures associated with Lennox-Gastaut syndrome (LGS) in patients 2 years of age or older | |indication=seizures associated with [[Lennox-Gastaut syndrome]] (LGS) in patients 2 years of age or older | ||
|adverseReactions=[[constipation]], [[somnolence]] or [[sedation]], [[pyrexia]], [[lethargy]], and [[drooling]] | |adverseReactions=[[constipation]], [[somnolence]] or [[sedation]], [[pyrexia]], [[lethargy]], and [[drooling]] | ||
|blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | |blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | |blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | ||
|fdaLIADAdult=====Seizures associated with Lennox-Gastaut syndrome (LGS)==== | |fdaLIADAdult=====Seizures associated with Lennox-Gastaut syndrome (LGS)==== | ||
*A daily dose of | *A daily dose of clobazam greater than 5 mg should be administered in divided doses twice daily | ||
*5 mg daily dose can be administered as a single dose. | *5 mg daily dose can be administered as a single dose. | ||
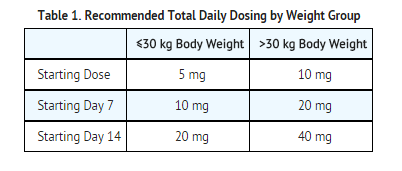
*Dose patients according to body weight. | *Dose patients according to body weight. | ||
| Line 20: | Line 20: | ||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Clobazam in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Clobazam in adult patients. | ||
|fdaLIADPed=====Seizures associated with Lennox-Gastaut syndrome (LGS) (2 years of age or older)==== | |fdaLIADPed=====Seizures associated with Lennox-Gastaut syndrome (LGS) (2 years of age or older)==== | ||
*A daily dose of | *A daily dose of clobazam greater than 5 mg should be administered in divided doses twice daily | ||
*5 mg daily dose can be administered as a single dose. | *5 mg daily dose can be administered as a single dose. | ||
*Dose patients according to body weight. | *Dose patients according to body weight. | ||
| Line 29: | Line 29: | ||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Clobazam in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Clobazam in pediatric patients. | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Clobazam in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Clobazam in pediatric patients. | ||
|contraindications=* | |contraindications=*Clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients. | ||
*Hypersensitivity reactions have included serious dermatological reactions. | *Hypersensitivity reactions have included serious dermatological reactions. | ||
|warnings=====Somnolence or Sedation==== | |warnings=====Somnolence or Sedation==== | ||
* | *Clobazam causes [[somnolence]] and [[sedation]]. | ||
*In clinical trials, somnolence or sedation was reported at all effective doses and was dose-related. | *In [[clinical trials]], [[somnolence]] or [[sedation]] was reported at all effective doses and was dose-related. | ||
*In general, somnolence and sedation begin within the first month of treatment and may diminish with continued treatment. | *In general, [[somnolence]] and [[sedation]] begin within the first month of treatment and may diminish with continued treatment. | ||
*Prescribers should monitor patients for somnolence and sedation, particularly with concomitant use of other central nervous system depressants. | *Prescribers should monitor patients for [[somnolence]] and [[sedation]], particularly with concomitant use of other central nervous system depressants. | ||
*Prescribers should caution patients against engaging in hazardous activities requiring mental alertness, such as operating dangerous machinery or motor vehicles, until the effect of | *Prescribers should caution patients against engaging in hazardous activities requiring mental alertness, such as operating dangerous machinery or motor vehicles, until the effect of clobazam is known. | ||
====Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants==== | ====Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants==== | ||
*Since | *Since clobazam has a [[central nervous system]] (CNS) depressant effect, patients or their caregivers should be cautioned against simultaneous use with other CNS depressant drugs or [[alcohol]], and cautioned that the effects of other CNS depressant drugs or [[alcohol]] may be potentiated. | ||
====Withdrawal Symptoms==== | ====Withdrawal Symptoms==== | ||
*Abrupt discontinuation of | *Abrupt discontinuation of clobazam should be avoided. | ||
* | *Clobazam should be tapered by decreasing the dose every week by 5-10 mg/day until discontinuation. | ||
*Withdrawal symptoms occurred following abrupt discontinuation of | *[[Withdrawal symptoms]] ([[Benzodiazepine withdrawal syndrome]]) occurred following abrupt discontinuation of clobazam; the risk of [[withdrawal symptoms]] is greater with higher doses. | ||
*As with all antiepileptic drugs, | *As with all [[antiepileptic]] drugs, clobazam should be withdrawn gradually to minimize the risk of precipitating [[seizures]], [[seizure]] exacerbation, or [[status epilepticus]]. | ||
*Withdrawal symptoms (e.g., convulsions, psychosis, hallucinations, behavioral disorder, tremor, and anxiety) have been reported following abrupt discontinuance of benzodiazepines. | *[[Withdrawal symptoms]] (e.g., [[convulsions]], [[psychosis]], [[hallucinations]], behavioral disorder, [[tremor]], and [[anxiety]]) have been reported following abrupt discontinuance of [[benzodiazepines]]. | ||
*The more severe withdrawal symptoms have usually been limited to patients who received excessive doses over an extended period of time, followed by an abrupt discontinuation. | *The more severe [[withdrawal symptoms]] have usually been limited to patients who received excessive doses over an extended period of time, followed by an abrupt discontinuation. | ||
*Generally milder withdrawal symptoms (e.g., dysphoria, anxiety, and insomnia) have been reported following abrupt discontinuance of benzodiazepines taken continuously at therapeutic doses for several months. | *Generally milder [[withdrawal symptoms]] (e.g., [[dysphoria]], [[anxiety]], and [[insomnia]]) have been reported following abrupt discontinuance of [[benzodiazepines]] taken continuously at therapeutic doses for several months. | ||
====Serious Dermatological Reactions==== | ====Serious Dermatological Reactions==== | ||
*Serious skin reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported with | *Serious skin reactions, including [[Stevens-Johnson syndrome]] ([[SJS]]) and [[toxic epidermal necrolysis]] ([[TEN]]), have been reported with clobazam in both children and adults during the post-marketing period. | ||
*Patients should be closely monitored for signs or symptoms of SJS/TEN, especially during the first 8 weeks of treatment initiation or when re-introducing therapy. | *Patients should be closely monitored for signs or symptoms of [[SJS]]/[[TEN]], especially during the first 8 weeks of treatment initiation or when re-introducing therapy. | ||
* | *Clobazam should be discontinued at the first sign of [[rash]], unless the [[rash]] is clearly not drug-related. | ||
*If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered. | *If signs or symptoms suggest [[SJS]]/[[TEN]], use of this drug should not be resumed and alternative therapy should be considered. | ||
====Physical and Psychological Dependence==== | ====Physical and Psychological Dependence==== | ||
*Patients with a history of substance abuse should be under careful surveillance when receiving | *Patients with a history of substance abuse should be under careful surveillance when receiving clobazam or other psychotropic agents because of the predisposition of such patients to habituation and dependence. | ||
====Suicidal Behavior and Ideation==== | ====Suicidal Behavior and Ideation==== | ||
*Antiepileptic drugs (AEDs), including | *[[Antiepileptic]] drugs (AEDs), including clobazam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. | ||
*Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted relative risk 1.8, 95% | *Patients treated with any AED for any indication should be monitored for the emergence or worsening of [[depression]], suicidal thoughts or behavior, and/or any unusual changes in mood or behavior. | ||
*Pooled analyses of 199 placebo-controlled [[clinical trials]] (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted relative risk 1.8, 95% cclobazamdence interval [CI]: 1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED treated patients was 0.43%, compared to 0.24% among 16,029 placebo treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. | |||
*There were four suicides in drug treated patients in the trials and none in placebo treated patients, but the number is too small to allow any conclusion about drug effect on suicide. | *There were four suicides in drug treated patients in the trials and none in placebo treated patients, but the number is too small to allow any conclusion about drug effect on suicide. | ||
*The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. | *The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. | ||
*Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed. | *Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed. | ||
*The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. | *The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. | ||
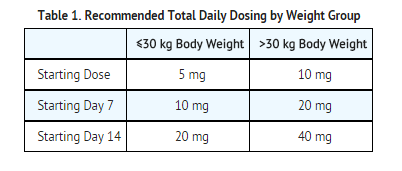
*The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs. | *The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the [[clinical trials]] analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs. | ||
[[File:Clobazam Warnings table.png|none|450px]] | [[File:Clobazam Warnings table.png|none|450px]] | ||
*The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications. | *The relative risk for suicidal thoughts or behavior was higher in [[clinical trials]] for [[epilepsy]] than in [[clinical trials]] for psychiatric or other conditions, but the absolute risk differences were similar for the [[epilepsy]] and psychiatric indications. | ||
*Anyone considering prescribing | *Anyone considering prescribing clobazam or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness. | ||
*Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. | *[[Epilepsy]] and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. | ||
*Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated. | *Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated. | ||
*Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. | *Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of [[depression]], any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. | ||
*Behaviors of concern should be reported immediately to healthcare providers. | *Behaviors of concern should be reported immediately to healthcare providers. | ||
|clinicalTrials=Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. | |clinicalTrials=Because [[clinical trials]] are conducted under widely varying conditions, adverse reaction rates observed in the [[clinical trials]] of a drug cannot be directly compared to rates in the [[clinical trials]] of another drug and may not reflect the rates observed in practice. | ||
*During its development for the adjunctive treatment of seizures associated with LGS, | *During its development for the adjunctive treatment of [[seizures]] associated with [[LGS]], clobazam was administered to 333 healthy volunteers and 300 patients with a current or prior diagnosis of [[LGS]], including 197 patients treated for 12 months or more. | ||
*The conditions and duration of exposure varied greatly and included single- and multiple-dose clinical pharmacology studies in healthy volunteers and two double-blind studies in patients with LGS (Study 1 and 2). Only Study 1 included a placebo group, allowing comparison of adverse reaction rates on | *The conditions and duration of exposure varied greatly and included single- and multiple-dose clinical pharmacology studies in healthy volunteers and two double-blind studies in patients with [[LGS]] (Study 1 and 2). Only Study 1 included a placebo group, allowing comparison of adverse reaction rates on clobazam at several doses to placebo. | ||
'''Adverse Reactions Leading to Discontinuation in an LGS Placebo Controlled Clinical Trial (Study 1)''' | '''Adverse Reactions Leading to Discontinuation in an LGS Placebo Controlled Clinical Trial (Study 1)''' | ||
*The adverse reactions associated with | *The adverse reactions associated with clobazam treatment discontinuation in ≥1% of patients in decreasing order of frequency included [[lethargy]], [[somnolence]], [[ataxia]], [[aggression]], [[fatigue]], and [[insomnia]]. | ||
'''Most Common Adverse Reactions in an LGS Placebo Controlled Clinical Trial (Study 1)''' | '''Most Common Adverse Reactions in an LGS Placebo Controlled Clinical Trial (Study 1)''' | ||
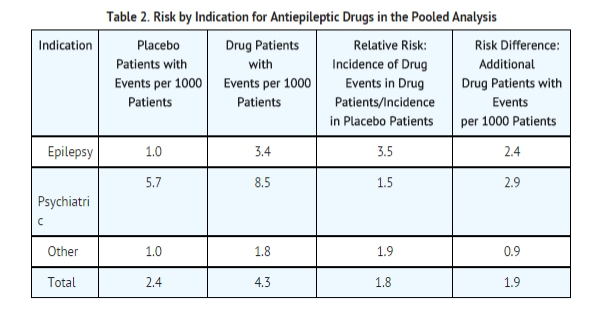
Table 3 lists the adverse reactions that occurred in ≥5% of | Table 3 lists the adverse reactions that occurred in ≥5% of clobazam treated patients (at any dose), and at a rate greater than placebo treated patients, in the randomized, double-blind, placebo-controlled, parallel group clinical study of adjunctive AED therapy for 15 weeks (Study 1). | ||
[[File:Clobazam side effect placebo vs.png|none|500px]] | [[File:Clobazam side effect placebo vs.png|none|500px]] | ||
| Line 90: | Line 91: | ||
====Blood Disorders==== | ====Blood Disorders==== | ||
*Anemia | *[[Anemia]] | ||
*Eosinophilia | *[[Eosinophilia]] | ||
*Leukopenia | *[[Leukopenia]] | ||
*Thrombocytopenia | *[[Thrombocytopenia]] | ||
====Eye Disorders==== | ====Eye Disorders==== | ||
*Diplopia | *[[Diplopia]] | ||
*Vision blurred | *[[Vision blurred]] | ||
====Gastrointestinal Disorders==== | ====Gastrointestinal Disorders==== | ||
| Line 103: | Line 104: | ||
====General Disorders and Administration Site Conditions==== | ====General Disorders and Administration Site Conditions==== | ||
*Hypothermia | *[[Hypothermia]] | ||
====Investigations==== | ====Investigations==== | ||
| Line 109: | Line 110: | ||
====Musculoskeletal==== | ====Musculoskeletal==== | ||
*Muscle spasms | *[[Muscle spasms]] | ||
====Psychiatric Disorders==== | ====Psychiatric Disorders==== | ||
*Agitation | *[[Agitation]] | ||
*Anxiety | *[[Anxiety]] | ||
*Apathy | *[[Apathy]] | ||
*Confusional state | *Confusional state | ||
*Depression | *[[Depression]] | ||
*Delirium | *[[Delirium]] | ||
*Delusion | *[[Delusion]] | ||
*Hallucination | *[[Hallucination]] | ||
====Renal and Urinary Disorders==== | ====Renal and Urinary Disorders==== | ||
*Urinary retention | *[[Urinary retention]] | ||
====Respiratory Disorders==== | ====Respiratory Disorders==== | ||
*Aspiration | *[[Aspiration]] | ||
*Respiratory depression | *[[Respiratory depression]] | ||
====Skin and Subcutaneous Tissue Disorders==== | ====Skin and Subcutaneous Tissue Disorders==== | ||
*Rash | *[[Rash]] | ||
*Urticaria | *[[Urticaria]] | ||
*Angioedema | *[[Angioedema]] | ||
*Facial and lip edema | *Facial and lip edema | ||
|drugInteractions=====Effect of | |drugInteractions=====Effect of clobazam on Other Drugs==== | ||
======Hormonal Contraceptives====== | ======Hormonal Contraceptives====== | ||
* | *Clobazam is a weak [[CYP3A4]] inducer. | ||
*As some hormonal contraceptives are metabolized by CYP3A4, their effectiveness may be diminished when given with | *As some hormonal contraceptives are metabolized by [[CYP3A4]], their effectiveness may be diminished when given with clobazam. | ||
*Additional non-hormonal forms of contraception are recommended when using | *Additional non-hormonal forms of contraception are recommended when using clobazam. | ||
======Drugs Metabolized by CYP2D6====== | ======Drugs Metabolized by CYP2D6====== | ||
* | *Clobazam inhibits [[CYP2D6]]. | ||
*Dose adjustment of drugs metabolized by CYP2D6 may be necessary. | *Dose adjustment of drugs metabolized by [[CYP2D6]] may be necessary. | ||
======Effect of Other Drugs on | ======Effect of Other Drugs on clobazam====== | ||
*Strong and moderate inhibitors of CYP2C19 | *Strong and moderate inhibitors of [[CYP2C19]] | ||
*Strong and moderate inhibitors of CYP2C19 may result in increased exposure to N-desmethylclobazam, the active metabolite of clobazam. | *Strong and moderate inhibitors of [[CYP2C19]] may result in increased exposure to N-desmethylclobazam, the active metabolite of clobazam. | ||
*This may increase the risk of dose-related adverse reactions. | *This may increase the risk of dose-related adverse reactions. | ||
*Dosage adjustment of | *Dosage adjustment of clobazam may be necessary when co-administered with strong [[CYP2C19]] inhibitors (e.g., [[fluconazole]], [[fluvoxamine]], [[ticlopidine]]) or moderate [[CYP2C19]] inhibitors (e.g., [[omeprazole]]). | ||
====CNS Depressants and Alcohol==== | ====CNS Depressants and Alcohol==== | ||
*Concomitant use of | *Concomitant use of clobazam with other CNS depressants may increase the risk of [[sedation]] and [[somnolence]]. | ||
*Alcohol, as a CNS depressant, will interact with | *[[Alcohol]], as a CNS depressant, will interact with clobazam in a similar way and also increases clobazam's maximum plasma exposure by approximately 50%. Therefore, caution patients or their caregivers against simultaneous use with other CNS depressant drugs or [[alcohol]], and caution that the effects of other CNS depressant drugs or [[alcohol]] may be potentiated. | ||
|FDAPregCat=C | |FDAPregCat=C | ||
|useInPregnancyFDA=*There are no adequate and well-controlled studies of | |useInPregnancyFDA=*There are no adequate and well-controlled studies of clobazam in pregnant women. | ||
*Available human data on the risk of teratogenicity associated with benzodiazepines are inconclusive. | *In animal studies, administration of clobazam during pregnancy resulted in developmental toxicity, including increased incidences of fetal malformations, at plasma exposures for clobazam and its major active metabolite, N-desmethylclobazam, below those expected at therapeutic doses in patients. Clobazam should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. | ||
*There is insufficient evidence in humans to assess the effect of benzodiazepine exposure during pregnancy on neurodevelopment. | *Available human data on the risk of teratogenicity associated with [[benzodiazepines]] are inconclusive. | ||
*Administration of benzodiazepines immediately prior to or during childbirth can result in a syndrome of hypothermia, hypotonia, respiratory depression, and difficulty feeding. | *There is insufficient evidence in humans to assess the effect of [[benzodiazepine]] exposure during pregnancy on neurodevelopment. | ||
*In addition, infants born to mothers who have taken benzodiazepines during the later stages of pregnancy can develop dependence, and subsequently withdrawal, during the postnatal period. | *Administration of [[benzodiazepines]] immediately prior to or during childbirth can result in a syndrome of [[hypothermia]], [[hypotonia]], [[respiratory depression]], and difficulty feeding. | ||
*Data for other benzodiazepines suggest the possibility of adverse developmental effects (including long-term effects on neurobehavioral and immunological function) in animals following prenatal exposure to benzodiazepines at clinically relevant doses. | *In addition, infants born to mothers who have taken [[benzodiazepines]] during the later stages of pregnancy can develop dependence, and subsequently withdrawal, during the postnatal period. | ||
*Data for other [[benzodiazepines]] suggest the possibility of adverse developmental effects (including long-term effects on neurobehavioral and immunological function) in animals following prenatal exposure to [[benzodiazepines]] at clinically relevant doses. | |||
*In a study in which clobazam (150, 450, or 750 mg/kg/day) was orally administered to pregnant rats throughout the period of organogenesis, embryofetal mortality and incidences of fetal skeletal variations were increased at all doses. | *In a study in which clobazam (150, 450, or 750 mg/kg/day) was orally administered to pregnant rats throughout the period of organogenesis, embryofetal mortality and incidences of fetal skeletal variations were increased at all doses. | ||
| Line 170: | Line 172: | ||
*Oral administration of clobazam (50, 350, or 750 mg/kg/day) to rats throughout pregnancy and lactation resulted in increased embryofetal mortality at the high dose, decreased pup survival at the mid and high doses and alterations in offspring behavior (locomotor activity) at all doses. The low effect dose for adverse effects on pre- and postnatal development in rats (50 mg/kg/day) was associated with plasma exposures for clobazam and N-desmethylclobazam lower than those in humans at the MRHD. | *Oral administration of clobazam (50, 350, or 750 mg/kg/day) to rats throughout pregnancy and lactation resulted in increased embryofetal mortality at the high dose, decreased pup survival at the mid and high doses and alterations in offspring behavior (locomotor activity) at all doses. The low effect dose for adverse effects on pre- and postnatal development in rats (50 mg/kg/day) was associated with plasma exposures for clobazam and N-desmethylclobazam lower than those in humans at the MRHD. | ||
|AUSPregCat=C | |AUSPregCat=C | ||
|useInNursing=* | |useInNursing=*Clobazam is excreted in human milk. | ||
*Because of the potential for serious adverse reactions in nursing infants from | *Because of the potential for serious adverse reactions in nursing infants from clobazam, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. | ||
|useInPed=*Safety and effectiveness in patients less than 2 years of age have not been established. | |useInPed=*Safety and effectiveness in patients less than 2 years of age have not been established. | ||
*In a study in which clobazam (4, 36, or 120 mg/kg/day) was orally administered to rats during the juvenile period of development (postnatal days 14 to 48), adverse effects on growth (decreased bone density and bone length) and behavior (altered motor activity and auditory startle response; learning deficit) were observed at the high dose. | *In a study in which clobazam (4, 36, or 120 mg/kg/day) was orally administered to rats during the juvenile period of development (postnatal days 14 to 48), adverse effects on growth (decreased bone density and bone length) and behavior (altered motor activity and auditory startle response; learning deficit) were observed at the high dose. | ||
*The effect on bone density, but not on behavior, was reversible when drug was discontinued. | *The effect on [[bone density]], but not on behavior, was reversible when drug was discontinued. | ||
*The no-effect level for juvenile toxicity (36 mg/kg/day) was associated with plasma exposures (AUC) to clobazam and its major active metabolite, N-desmethylclobazam, less than those expected at therapeutic doses in pediatric patients. | *The no-effect level for juvenile toxicity (36 mg/kg/day) was associated with plasma exposures (AUC) to clobazam and its major active metabolite, N-desmethylclobazam, less than those expected at therapeutic doses in pediatric patients. | ||
|useInGeri=*Plasma concentrations at any given dose are generally higher in the elderly: proceed slowly with dose escalation. | |useInGeri=*Plasma concentrations at any given dose are generally higher in the elderly: proceed slowly with dose escalation. | ||
| Line 180: | Line 182: | ||
*Then titrate elderly patients according to weight, but to half the dose presented in Table 1, as tolerated. | *Then titrate elderly patients according to weight, but to half the dose presented in Table 1, as tolerated. | ||
*If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on weight) may be started on day 21. | *If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on weight) may be started on day 21. | ||
*Clinical studies of | *Clinical studies of clobazam did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. However, elderly subjects appear to eliminate clobazam more slowly than younger subjects based on population pharmacokinetic analysis. For these reasons, the initial dose in elderly patients should be 5 mg/day. | ||
|useInRenalImpair=*No dose adjustment is required for patients with mild and moderate renal impairment. | |useInGender=*Population pharmacokinetic analyses showed no difference in the clearance of clobazam between women and men. | ||
*There is no experience with | |useInRace=*Population pharmacokinetic analyses including Caucasian (75%), African American (15%), and Asian (9%) subjects showed that there is no evidence of clinically significant effect of race on the clearance of clobazam. | ||
|useInRenalImpair=*No dose adjustment is required for patients with mild and moderate [[renal impairment]]. | |||
*There is no experience with clobazam in patients with severe [[renal impairment]] or [[end stage renal disease]] (ESRD). | |||
*It is not known if clobazam or its active metabolite, N-desmethylclobazam, is dialyzable. | *It is not known if clobazam or its active metabolite, N-desmethylclobazam, is dialyzable. | ||
|useInHepaticImpair=* | |useInHepaticImpair=*Clobazam is hepatically metabolized; however, there are limited data to characterize the effect of [[hepatic impairment]] on the pharmacokinetics of clobazam. *For this reason, proceed slowly with dosing escalations. | ||
*For patients with mild to moderate hepatic impairment (Child-Pugh score 5-9), the starting dose should be 5 mg/day in both weight groups. | *For patients with mild to moderate hepatic impairment ([[Child-Pugh]] score 5-9), the starting dose should be 5 mg/day in both weight groups. | ||
*Then titrate patients according to weight, but to half the dose presented in Table 1, as tolerated. | *Then titrate patients according to weight, but to half the dose presented in Table 1, as tolerated. | ||
*If necessary and based upon clinical response, start an additional titration on day 21 to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group). | *If necessary and based upon clinical response, start an additional titration on day 21 to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group). | ||
*There is inadequate information about metabolism of | *There is inadequate information about metabolism of clobazam in patients with severe hepatic impairment. | ||
*Therefore no dosing recommendation in those patients can be given. | *Therefore no dosing recommendation in those patients can be given. | ||
|othersTitle=Dosage Adjustments in CYP2C19 Poor Metabolizers | |othersTitle=Dosage Adjustments in CYP2C19 Poor Metabolizers | ||
|useInOthers=*In CYP2C19 poor metabolizers, levels of N-desmethylclobazam, clobazam's active metabolite, will be increased. Therefore, in patients known to be CYP2C19 poor metabolizers, the starting dose should be 5 mg/day and dose titration should proceed slowly according to weight, but to half the dose presented in Table 1, as tolerated. | |useInOthers=*In [[CYP2C19]] poor metabolizers, levels of N-desmethylclobazam, clobazam's active metabolite, will be increased. Therefore, in patients known to be [[CYP2C19]] poor metabolizers, the starting dose should be 5 mg/day and dose titration should proceed slowly according to weight, but to half the dose presented in Table 1, as tolerated. | ||
*If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group) may be started on day 21. | *If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group) may be started on day 21. | ||
|administration=*Oral | |administration=*Oral | ||
=====Important Administration Instructions===== | =====Important Administration Instructions===== | ||
*Instruct patients to read the "Instructions for Use" carefully for complete directions on how to properly dose and administer | *Instruct patients to read the "Instructions for Use" carefully for complete directions on how to properly dose and administer clobazam oral suspension. | ||
==== | ====clobazam Tablet Oral Administration==== | ||
* | *Clobazam tablets can be taken with or without food. | ||
* | *Clobazam tablets can be administered whole, broken in half along the score, or crushed and mixed in applesauce. | ||
==== | ====Clobazam Oral Suspension Oral Administration==== | ||
* | *Clobazam oral suspension can be taken with or without food. | ||
*Shake | *Shake clobazam Oral Suspension well before every administration. | ||
*When administering the oral suspension, use only the oral dosing syringe provided with the product. | *When administering the oral suspension, use only the oral dosing syringe provided with the product. | ||
*Each carton includes two syringes, but only one syringe should be used for dosing. | *Each carton includes two syringes, but only one syringe should be used for dosing. | ||
*The second oral syringe is reserved as a replacement in case the first syringe is damaged or lost. | *The second oral syringe is reserved as a replacement in case the first syringe is damaged or lost. | ||
*Insert the provided adapter firmly into the neck of the bottle before first use and keep the adapter in place for the duration of the usage of the bottle. *To withdraw the dose, insert the dosing syringe into the adapter and invert the bottle then slowly pull back the plunger to prescribed dose. | *Insert the provided adapter firmly into the neck of the bottle before first use and keep the adapter in place for the duration of the usage of the bottle. *To withdraw the dose, insert the dosing syringe into the adapter and invert the bottle then slowly pull back the plunger to prescribed dose. | ||
*After removing the syringe from the bottle adapter, slowly squirt | *After removing the syringe from the bottle adapter, slowly squirt clobazam Oral Suspension into the corner of the patient's mouth. | ||
*Replace the cap after each use. | *Replace the cap after each use. | ||
*The cap fits over the adapter when the adapter is properly placed. | *The cap fits over the adapter when the adapter is properly placed. | ||
|monitoring=*Monitor for central nervous system (CNS) depression. | |monitoring=*Monitor for [[central nervous system]] (CNS) depression. | ||
* Monitor patients with a history of substance abuse for signs of habituation and dependence. | * Monitor patients with a history of substance abuse for signs of habituation and dependence. | ||
*Monitor for suicidal thoughts or behaviors. | *Monitor for suicidal thoughts or behaviors. | ||
*Monitored for signs or symptoms of SJS/TEN, especially during the first 8 weeks of treatment initiation or when re-introducing therapy. | *Monitored for signs or symptoms of [[SJS]]/[[TEN]], especially during the first 8 weeks of treatment initiation or when re-introducing therapy. | ||
|overdose=====Signs and Symptoms of Overdosage==== | |overdose=====Signs and Symptoms of Overdosage==== | ||
*Overdose and intoxication with benzodiazepines, including | *Overdose and intoxication with [[benzodiazepines]], including clobazam, may lead to CNS depression, associated with [[drowsiness]], [[confusion]] and [[lethargy]], possibly progressing to [[ataxia]], [[respiratory depression]], [[hypotension]], and, rarely, coma or death. | ||
*The risk of a fatal outcome is increased in cases of combined poisoning with other CNS depressants, including alcohol. | *The risk of a fatal outcome is increased in cases of combined poisoning with other CNS depressants, including [[alcohol]]. | ||
====Management of Overdosage==== | ====Management of Overdosage==== | ||
*The management of | *The management of clobazam overdose may include [[gastric lavage]] and/or administration of activated charcoal, intravenous fluid replenishment, early control of airway and general supportive measures, in addition to monitoring level of consciousness and vital signs. | ||
*Hypotension can be treated by replenishment with plasma substitutes and, if necessary, with sympathomimetic agents. | *[[Hypotension]] can be treated by replenishment with plasma substitutes and, if necessary, with sympathomimetic agents. | ||
*The efficacy of supplementary administration of physostigmine (a cholinergic agent) or of flumazenil (a benzodiazepine antagonist) in | *The efficacy of supplementary administration of [[physostigmine]] (a cholinergic agent) or of [[flumazenil]] (a [[benzodiazepine]] antagonist) in clobazam overdose has not been assessed. | ||
*The administration of flumazenil in cases of benzodiazepine overdose can lead to withdrawal and adverse reactions. Its use in patients with epilepsy is typically not recommended. | *The administration of [[flumazenil]] in cases of [[benzodiazepine]] overdose can lead to withdrawal and adverse reactions. Its use in patients with [[epilepsy]] is typically not recommended. | ||
|drugBox={{Drugbox | |drugBox={{Drugbox | ||
| Watchedfields = changed | | Watchedfields = changed | ||
| Line 232: | Line 236: | ||
<!--Clinical data--> | <!--Clinical data--> | ||
| licence_US = Clobazam | | licence_US = Clobazam | ||
| tradename = Frisium, Urbanol, | | tradename = Frisium, Urbanol, clobazam | ||
| Drugs.com = {{drugs.com|CONS|clobazam}} | | Drugs.com = {{drugs.com|CONS|clobazam}} | ||
| pregnancy_US = C | | pregnancy_US = C | ||
| Line 277: | Line 281: | ||
| StdInChIKey = CXOXHMZGEKVPMT-UHFFFAOYSA-N | | StdInChIKey = CXOXHMZGEKVPMT-UHFFFAOYSA-N | ||
}} | }} | ||
|mechAction=*The exact mechanism of action for clobazam, a 1,5-benzodiazepine, is not fully understood but is thought to involve potentiation of GABAergic neurotransmission resulting from binding at the benzodiazepine site of the GABAA receptor. | |mechAction=*The exact mechanism of action for clobazam, a 1,5-[[benzodiazepine]], is not fully understood but is thought to involve potentiation of [[GABAergic]] neurotransmission resulting from binding at the benzodiazepine site of the GABAA receptor. | ||
|structure=*Clobazam is a white or almost white, crystalline powder with a slightly bitter taste; is slightly soluble in water, sparingly soluble in ethanol, and freely soluble in methylene chloride. | |structure=*Clobazam is a white or almost white, crystalline powder with a slightly bitter taste; is slightly soluble in water, sparingly soluble in ethanol, and freely soluble in methylene chloride. | ||
*The melting range of clobazam is from 182ºC to 185ºC. | *The melting range of clobazam is from 182ºC to 185ºC. | ||
| Line 284: | Line 288: | ||
[[File:Clobazam chemical structure.png|none|250px]] | [[File:Clobazam chemical structure.png|none|250px]] | ||
|PD=====Effects on Electrocardiogram==== | |PD=====Effects on Electrocardiogram==== | ||
*The effect of | *The effect of clobazam 20 mg and 80 mg administered twice daily on QTc interval was evaluated in a randomized, evaluator blinded, placebo-, and active-controlled (moxifloxacin 400 mg) parallel thorough QT study in 280 healthy subjects. | ||
*In a study with demonstrated ability to detect small effects, the upper bound of the one-sided 95% | *In a study with demonstrated ability to detect small effects, the upper bound of the one-sided 95% cclobazamdence interval for the largest placebo adjusted, baseline-corrected [[QTc]] based on the Fridericia correction method was below 10 ms, the threshold for regulatory concern. | ||
*Thus, at a dose two times the maximum recommended dose, | *Thus, at a dose two times the maximum recommended dose, clobazam did not prolong the [[QTc interval]] to any clinically relevant extent. | ||
|PK=*The peak plasma levels (Cmax) and the area under the curve (AUC) of clobazam are dose-proportional over the dose range of 10-80 mg following single- or multiple-dose administration of | |PK=*The peak plasma levels (Cmax) and the area under the curve (AUC) of clobazam are dose-proportional over the dose range of 10-80 mg following single- or multiple-dose administration of clobazam. | ||
*Based on a population pharmacokinetic analysis, the pharmacokinetics of clobazam are linear from 5-160 mg/day. | *Based on a population pharmacokinetic analysis, the pharmacokinetics of clobazam are linear from 5-160 mg/day. | ||
*Clobazam is converted to N-desmethylclobazam which has about 1/5 the activity of clobazam. | *Clobazam is converted to N-desmethylclobazam which has about 1/5 the activity of clobazam. | ||
| Line 296: | Line 300: | ||
*The relative bioavailability of clobazam tablets compared to an oral solution is approximately 100%. | *The relative bioavailability of clobazam tablets compared to an oral solution is approximately 100%. | ||
*After single dose administration of the oral suspension under fasted conditions, the Tmax ranged from 0.5 to 2 hours. | *After single dose administration of the oral suspension under fasted conditions, the Tmax ranged from 0.5 to 2 hours. | ||
*Based on exposure (Cmax and AUC) of clobazam, | *Based on exposure (Cmax and AUC) of clobazam, clobazam tablets and suspension were shown to have similar bioavailability under fasted conditions. | ||
*The administration of | *The administration of clobazam tablets with food or when crushed in applesauce does not affect absorption. | ||
*Although not studied, the oral bioavailability of the oral suspension is unlikely to be affected under fed conditions. | *Although not studied, the oral bioavailability of the oral suspension is unlikely to be affected under fed conditions. | ||
| Line 306: | Line 310: | ||
====Metabolism and Excretion==== | ====Metabolism and Excretion==== | ||
*Clobazam is extensively metabolized in the liver, with approximately 2% of the dose recovered in urine and 1% in feces as unchanged drug. | *Clobazam is extensively metabolized in the liver, with approximately 2% of the dose recovered in urine and 1% in feces as unchanged drug. | ||
*The major metabolic pathway of clobazam involves N-demethylation, primarily by CYP3A4 and to a lesser extent by CYP2C19 and CYP2B6. | *The major metabolic pathway of clobazam involves N-demethylation, primarily by [[CYP3A4]] and to a lesser extent by [[CYP2C19]] and [[CYP2B6]]. | ||
*N-desmethylclobazam, an active metabolite, is the major circulating metabolite in humans, and at therapeutic doses, plasma concentrations are 3-5 times higher than those of the parent compound. | *N-desmethylclobazam, an active metabolite, is the major circulating metabolite in humans, and at therapeutic doses, plasma concentrations are 3-5 times higher than those of the parent compound. | ||
*Based on animal and in vitro receptor binding data, estimates of the relative potency of N-desmethylclobazam compared to parent compound range from 1/5 to equal potency. | *Based on animal and [[in vitro]] receptor binding data, estimates of the relative potency of N-desmethylclobazam compared to parent compound range from 1/5 to equal potency. | ||
*N-desmethylclobazam is extensively metabolized, mainly by CYP2C19. | *N-desmethylclobazam is extensively metabolized, mainly by [[CYP2C19]]. | ||
*N-desmethylclobazam and its metabolites comprise ~94% of the total drug-related components in urine. | *N-desmethylclobazam and its metabolites comprise ~94% of the total drug-related components in urine. | ||
*Following a single oral dose of radiolabeled drug, approximately 11% of the dose was excreted in the feces and approximately 82% was excreted in the urine. | *Following a single oral dose of radiolabeled drug, approximately 11% of the dose was excreted in the feces and approximately 82% was excreted in the urine. | ||
*The polymorphic CYP2C19 is the major contributor to the metabolism of the pharmacologically active N-desmethylclobazam. | *The polymorphic [[CYP2C19]] is the major contributor to the metabolism of the pharmacologically active N-desmethylclobazam. | ||
*In CYP2C19 poor metabolizers, levels of N-desmethylclobazam were 5-fold higher in plasma and 2- to 3-fold higher in the urine than in CYP2C19 extensive metabolizers. | *In [[CYP2C19]] poor metabolizers, levels of N-desmethylclobazam were 5-fold higher in plasma and 2- to 3-fold higher in the urine than in [[CYP2C19]] extensive metabolizers. | ||
====Pharmacokinetics in Specific Populations==== | ====Pharmacokinetics in Specific Populations==== | ||
| Line 328: | Line 332: | ||
======Renal Impairment====== | ======Renal Impairment====== | ||
*The effect of renal impairment on the pharmacokinetics of clobazam was evaluated in patients with mild (creatinine clearance [CLCR] >50 to 80 mL/min; N=6) and moderate (CLCR=30 to 50 mL/min; N=6) renal dysfunction, with matching healthy controls (N=6), following administration of multiple doses of | *The effect of renal impairment on the pharmacokinetics of clobazam was evaluated in patients with mild ([[creatinine clearance]] [CLCR] >50 to 80 mL/min; N=6) and moderate (CLCR=30 to 50 mL/min; N=6) renal dysfunction, with matching healthy controls (N=6), following administration of multiple doses of clobazam 20 mg/day. | ||
*There were insignificant changes in Cmax (3-24%) and AUC (≤13%) for clobazam or N-desmethylclobazam in patients with mild or moderate renal impairment compared to patients with normal renal function. | *There were insignificant changes in Cmax (3-24%) and AUC (≤13%) for clobazam or N-desmethylclobazam in patients with mild or moderate [[renal impairment]] compared to patients with normal renal function. | ||
*Patients with severe renal impairment or ESRD were not included in this study. | *Patients with severe [[renal impairment]] or ESRD were not included in this study. | ||
======Hepatic Impairment====== | ======Hepatic Impairment====== | ||
*There are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam. | *There are limited data to characterize the effect of [[hepatic impairment]] on the pharmacokinetics of clobazam. | ||
*In a small study, the pharmacokinetics of a 20 mg single oral dose of | *In a small study, the pharmacokinetics of a 20 mg single oral dose of clobazam in 9 patients with liver impairment were compared to healthy controls (N=6). | ||
*The Cmax and the mean plasma clearance of clobazam, as well as the Cmax of N-desmethylclobazam, showed no significant change compared to the healthy controls. | *The Cmax and the mean plasma clearance of clobazam, as well as the Cmax of N-desmethylclobazam, showed no significant change compared to the healthy controls. | ||
*The AUC values of N-desmethylclobazam in these patients were not available. Adjust dosage in patients with hepatic impairment. | *The AUC values of N-desmethylclobazam in these patients were not available. Adjust dosage in patients with hepatic impairment. | ||
| Line 341: | Line 345: | ||
======In vitro studies====== | ======In vitro studies====== | ||
*Clobazam did not inhibit: CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, UGT1A1, UGT1A4, UGT1A6, or UGT2B4 in vitro. | *Clobazam did not inhibit: [[CYP1A2]], [[CYP2C8]], [[CYP2C9]], [[CYP2C19]], [[CYP2D6]], [[CYP3A4]], [[UGT1A1]], [[UGT1A4]], [[UGT1A6]], or [[UGT2B4]] [[in vitro]]. | ||
*N-desmethylclobazam showed weak inhibition of: CYP2C9, UGT1A4, UGT1A6 and UGT2B4. | *N-desmethylclobazam showed weak inhibition of: [[CYP2C9]], [[UGT1A4]], [[UGT1A6]] and [[UGT2B4]]. | ||
*Clobazam and N-desmethylclobazam did not significantly increase CYP1A2 or CYP2C19 activities, but did induce CYP3A4 activity in a concentration-dependent manner. | *Clobazam and N-desmethylclobazam did not significantly increase [[CYP1A2]] or [[CYP2C19]] activities, but did induce [[CYP3A4]] activity in a concentration-dependent manner. | ||
*Clobazam and N-desmethylclobazam also increased UGT1A1 mRNA but at concentrations much higher than therapeutic levels. | *Clobazam and N-desmethylclobazam also increased [[UGT1A1]] [[mRNA]] but at concentrations much higher than therapeutic levels. | ||
*The potential for clobazam or N-desmethylclobazam to induce CYP2B6 and CYP2C8 has not been evaluated. | *The potential for clobazam or N-desmethylclobazam to induce [[CYP2B6]]and [[CYP2C8]] has not been evaluated. | ||
*Clobazam and N-desmethylclobazam do not inhibit P-glycoprotein (P-gp), but are P-gp substrates. | *Clobazam and N-desmethylclobazam do not inhibit P-glycoprotein (P-gp), but are P-gp substrates. | ||
======In vivo studies====== | ======In vivo studies====== | ||
'''Potential for | '''Potential for clobazam to Affect Other Drugs''' | ||
*The effect of repeated 40 mg once-daily doses of | *The effect of repeated 40 mg once-daily doses of clobazam on the pharmacokinetic profiles of single-dose dextromethorphan ([[CYP2D6]] substrate), midazolam (CYP3A4 substrate), caffeine (CYP1A2 substrate), and [[tolbutamide]] ([[CYP2C9]] substrate), was studied when these probe substrates were given as a drug cocktail (N=18). | ||
*Clobazam increased AUC and Cmax of dextromethorphan by 90% and 59%, respectively, reflecting its inhibition of CYP2D6 in vivo. | *Clobazam increased AUC and Cmax of dextromethorphan by 90% and 59%, respectively, reflecting its inhibition of [[CYP2D6]] [[in vivo]]. | ||
*Drugs metabolized by CYP2D6 may require dose adjustment when used with | *Drugs metabolized by [[CYP2D6]] may require dose adjustment when used with clobazam. | ||
*Clobazam decreased the AUC and Cmax of midazolam by 27% and 24%, respectively, and increased the AUC and Cmax of the metabolite 1-hydroxymidazolam by 4-fold and 2-fold, respectively. | *Clobazam decreased the AUC and Cmax of [[midazolam]] by 27% and 24%, respectively, and increased the AUC and Cmax of the metabolite 1-hydroxymidazolam by 4-fold and 2-fold, respectively. | ||
*This level of induction does not call for dosage adjustment of drugs that are primarily metabolized by CYP3A4 when used concomitantly with | *This level of induction does not call for dosage adjustment of drugs that are primarily metabolized by [[CYP3A4]] when used concomitantly with clobazam. | ||
*Some hormonal contraceptives are metabolized by CYP3A4 and their effectiveness may be diminished when given with | *Some hormonal contraceptives are metabolized by [[CYP3A4]] and their effectiveness may be diminished when given with clobazam. Repeated clobazam doses had no effect on [[caffeine]] and [[tolbutamide]]. | ||
*A population pharmacokinetic analysis indicated clobazam did not affect the exposure of valproic acid (a CYP2C9/2C19 substrate) or lamotrigine (a UGT substrate). | *A population pharmacokinetic analysis indicated clobazam did not affect the exposure of [[valproic acid]] (a [[CYP2C9]]/2C19 substrate) or [[lamotrigine]] (a UGT substrate). | ||
'''Potential for Other Drugs to Affect | '''Potential for Other Drugs to Affect clobazam''' | ||
*Co-administration of ketoconazole (a strong CYP3A4 inhibitor) 400 mg once-daily for 5 days increased clobazam AUC by 54%, with an insignificant effect on clobazam Cmax. | *Co-administration of [[ketoconazole]] (a strong [[CYP3A4]] inhibitor) 400 mg once-daily for 5 days increased clobazam AUC by 54%, with an insignificant effect on clobazam Cmax. | ||
*There was no significant change in AUC and Cmax of N-desmethylclobazam (N=18). | *There was no significant change in AUC and Cmax of N-desmethylclobazam (N=18). | ||
*Strong (e.g., fluconazole, fluvoxamine, ticlopidine) and moderate (e.g., omeprazole) inhibitors of CYP2C19 may result in up to a 5-fold increase in exposure to N-desmethylclobazam, the active metabolite of clobazam, based on extrapolation from pharmacogenomic data. | *Strong (e.g., [[fluconazole]], [[fluvoxamine]], [[ticlopidine]]) and moderate (e.g., [[omeprazole]]) inhibitors of [[CYP2C19]] may result in up to a 5-fold increase in exposure to N-desmethylclobazam, the active metabolite of clobazam, based on extrapolation from pharmacogenomic data. | ||
*Dosage adjustment of | *Dosage adjustment of clobazam may be necessary when co-administered with strong or moderate [[CYP2C19]] inhibitors. | ||
*The effects of concomitant antiepileptic drugs that are CYP3A4 inducers (phenobarbital, phenytoin, and carbamazepine), CYP2C9 inducers (valproic acid, phenobarbital, phenytoin, and carbamazepine), and CYP2C9 inhibitors (felbamate and oxcarbazepine) were evaluated using data from clinical trials. | *The effects of concomitant antiepileptic drugs that are [[CYP3A4]] inducers ([[phenobarbital]], [[phenytoin]], and [[carbamazepine]]), [[CYP2C9]] inducers ([[valproic acid]], [[phenobarbital]], [[phenytoin]], and [[carbamazepine]]), and [[CYP2C9]] inhibitors ([[felbamate]] and [[oxcarbazepine]]) were evaluated using data from [[clinical trials]]. | ||
*Results of population pharmacokinetic analysis show that these concomitant antiepileptic drugs did not significantly alter the pharmacokinetics of clobazam or N-desmethylclobazam at steady-state. | *Results of population pharmacokinetic analysis show that these concomitant antiepileptic drugs did not significantly alter the pharmacokinetics of clobazam or N-desmethylclobazam at steady-state. | ||
*Alcohol has been reported to increase the maximum plasma exposure of clobazam by approximately 50%. Alcohol may have additive CNS depressant effects when taken with | *[[Alcohol]] has been reported to increase the maximum plasma exposure of clobazam by approximately 50%. [[Alcohol]] may have additive CNS depressant effects when taken with clobazam. | ||
|nonClinToxic=====Carcinogenesis, Mutagenesis, Impairment of Fertility==== | |nonClinToxic=====Carcinogenesis, Mutagenesis, Impairment of Fertility==== | ||
======Carcinogenesis====== | ======Carcinogenesis====== | ||
*The carcinogenic potential of clobazam has not been adequately assessed. | *The [[carcinogenic]] potential of clobazam has not been adequately assessed. | ||
*In a limited study in rats, oral administration of clobazam (4, 20, and 100 mg/kg/day) for 2 years resulted in an increased incidence of thyroid follicular cell adenomas in males at the high dose. | *In a limited study in rats, oral administration of clobazam (4, 20, and 100 mg/kg/day) for 2 years resulted in an increased incidence of thyroid follicular cell adenomas in males at the high dose. | ||
======Mutagenesis====== | ======Mutagenesis====== | ||
*Clobazam and the major active metabolite, N-desmethylclobazam, were negative for genotoxicity, based on data from a battery of in vitro (bacteria reverse mutation, mammalian clastogenicity) and in vivo (mouse micronucleus) assays. | *Clobazam and the major active metabolite, N-desmethylclobazam, were negative for genotoxicity, based on data from a battery of [[in vitro]] (bacteria reverse mutation, mammalian clastogenicity) and [[in vivo]] (mouse micronucleus) assays. | ||
======Impairment of Fertility====== | ======Impairment of Fertility====== | ||
*In a study in which clobazam (50, 350, or 750 mg/kg/day) was orally administered to male and female rats prior to and during mating and continuing in females to gestation day 6, increases in abnormal sperm and pre-implantation loss were observed at the highest dose tested. | *In a study in which clobazam (50, 350, or 750 mg/kg/day) was orally administered to male and female rats prior to and during mating and continuing in females to gestation day 6, increases in abnormal sperm and pre-implantation loss were observed at the highest dose tested. | ||
*The no effect level for fertility and early embryonic development in rats was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, less than those in humans at the maximum recommended human dose of 40 mg/day. | *The no effect level for fertility and early embryonic development in rats was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, less than those in humans at the maximum recommended human dose of 40 mg/day. | ||
|clinicalStudies=The effectiveness of | |clinicalStudies=The effectiveness of clobazam for the adjunctive treatment of seizures associated with [[Lennox-Gastaut syndrome]] was established in two multicenter controlled studies (Study 1 and Study 2). Both studies were similar in terms of disease characteristics and concomitant AED treatments. The most common concomitant AED treatments at baseline included: [[valproate]], [[lamotrigine]], [[levetiracetam]], and [[topiramate]]. | ||
====Study 1==== | ====Study 1==== | ||
Study 1 (N=238) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and 12-week maintenance period. Patients age 2-54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of | Study 1 (N=238) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and 12-week maintenance period. Patients age 2-54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of clobazam according to Table 5. | ||
[[File:Clobazam study 1.png|none|400px]] | [[File:Clobazam study 1.png|none|400px]] | ||
| Line 386: | Line 390: | ||
Doses above 5 mg/day were administered in two divided doses. | Doses above 5 mg/day were administered in two divided doses. | ||
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to 12-week maintenance period. | The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to 12-week maintenance period. | ||
The pre-dosing baseline mean weekly drop seizure frequency was 98, 100, 61, and 105 for the placebo, low-, medium-, and high-dose groups, respectively. Figure 1 presents the mean percent reduction in weekly drop seizures from this baseline. All dose groups of | The pre-dosing baseline mean weekly drop seizure frequency was 98, 100, 61, and 105 for the placebo, low-, medium-, and high-dose groups, respectively. Figure 1 presents the mean percent reduction in weekly drop seizures from this baseline. All dose groups of clobazam were statistically superior (p≤0.05) to the placebo group. This effect appeared to be dose dependent. | ||
[[File:Clobazam Study 1 part 3.png|none| | [[File:Clobazam Study 1 part 3.png|none|550px]] | ||
Figure 2 shows changes from baseline in weekly drop seizure frequency by category for patients treated with | Figure 2 shows changes from baseline in weekly drop [[seizure]] frequency by category for patients treated with clobazam and placebo in Study 1. Patients in whom the [[seizure]] frequency increased are shown at left as "worse." Patients in whom the [[seizure]] frequency decreased are shown in five categories. | ||
There was no evidence that tolerance to the therapeutic effect of | There was no evidence that tolerance to the therapeutic effect of clobazam developed during the 3-month maintenance period. | ||
====Study 2==== | ====Study 2==== | ||
Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose | Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose clobazam, consisting of a 4-week baseline period followed by a 3-week titration period and 4-week maintenance period. Patients age 2-25 years with a current or prior diagnosis of LGS were stratified by weight, then randomized to either a low or high dose of clobazam, and then entered a 3-week titration period. | ||
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to the 4-week maintenance period. | The primary efficacy measure was the percent reduction in the weekly frequency of drop [[seizures]] (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to the 4-week maintenance period. | ||
A statistically significantly greater reduction in seizure frequency was observed in the high-dose group compared to the low-dose group (median percent reduction of 93% vs 29%; p<0.05). | A statistically significantly greater reduction in seizure frequency was observed in the high-dose group compared to the low-dose group (median percent reduction of 93% vs 29%; p<0.05). | ||
| Line 407: | Line 411: | ||
====Clobazam- Oral suspension==== | ====Clobazam- Oral suspension==== | ||
* | *Clobazam oral suspension is a berry flavored off-white liquid supplied in a bottle with child-resistant closure. | ||
*The oral suspension is packaged with a dispenser set which contains two calibrated oral dosing syringes and a bottle adapter. | *The oral suspension is packaged with a dispenser set which contains two calibrated oral dosing syringes and a bottle adapter. | ||
**NDC 67386-313-21: 2.5 mg/mL supplied in a bottle containing 120 mL of suspension. | **NDC 67386-313-21: 2.5 mg/mL supplied in a bottle containing 120 mL of suspension. | ||
| Line 413: | Line 417: | ||
*Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature. | *Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature. | ||
====Clobazam Oral suspension==== | ====Clobazam Oral suspension==== | ||
*Store and dispense | *Store and dispense clobazam oral suspension in its original bottle in an upright position. | ||
*Use within 90 days of first opening the bottle, then discard any remainder | *Use within 90 days of first opening the bottle, then discard any remainder | ||
*Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature. | *Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature. | ||
|packLabel=[[File:Clobazam FDA label 1.png|none|450px]] | |||
[[File:Clobazam FDA label 2.png|none|450px]] | |||
[[File:Clobazam FDA label 3.png|none|450px]] | |||
[[File:Clobaza FDA label 4.png|none|450px]] | |||
[[File:Clobazam FDA label 5.png|none|450px]] | |||
[[File:Clobazam FDA label 6.png|none|450px]] | |||
|fdaPatientInfo=====Hypersensitivity==== | |fdaPatientInfo=====Hypersensitivity==== | ||
Inform patients or caregivers that | Inform patients or caregivers that clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients. | ||
====Somnolence or Sedation==== | ====Somnolence or Sedation==== | ||
Advise patients or caregivers to check with their healthcare provider before | Advise patients or caregivers to check with their healthcare provider before clobazam is taken with other CNS depressants such as other [[benzodiazepines]], [[opioids]], [[tricyclic antidepressants]], sedating antihistamines, or [[alcohol]]. | ||
If applicable, caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that | If applicable, caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that clobazam does not affect them adversely (e.g., impair judgment, thinking or motor skills). | ||
====Increasing or Decreasing the | ====Increasing or Decreasing the clobazam Dose==== | ||
Inform patients or caregivers to consult their healthcare provider before increasing the | Inform patients or caregivers to consult their healthcare provider before increasing the clobazam dose or abruptly discontinuing clobazam. Advise patients or caregivers that abrupt withdrawal of AEDs may increase their risk of [[seizure]]. | ||
====Interactions with Hormonal Contraceptives==== | ====Interactions with Hormonal Contraceptives==== | ||
Counsel women to also use non-hormonal methods of contraception when | Counsel women to also use non-hormonal methods of contraception when clobazam is used with hormonal contraceptives and to continue these alternative methods for 28 days after discontinuing clobazam to ensure contraceptive reliability. | ||
====Serious Dermatological Reactions==== | ====Serious Dermatological Reactions==== | ||
Advise patients or caregivers that serious skin reactions have been reported in patients taking | Advise patients or caregivers that serious skin reactions have been reported in patients taking clobazam. Serious skin reactions, including [[SJS]]/[[TEN]], may need to be treated in a hospital and may be life-threatening. If a skin reaction occurs while taking clobazam, patients or caregivers should consult with healthcare providers immediately. | ||
====Suicidal Thinking and Behavior==== | ====Suicidal Thinking and Behavior==== | ||
Counsel patients, their caregivers, and their families that AEDs, including | Counsel patients, their caregivers, and their families that AEDs, including clobazam, may increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts of self-harm. Patients should report behaviors of concern immediately to healthcare providers. | ||
====Use in Pregnancy==== | ====Use in Pregnancy==== | ||
| Line 441: | Line 456: | ||
====Use in Nursing==== | ====Use in Nursing==== | ||
Instruct patients to notify their physician if they are breast feeding or intend to breast feed during therapy. | Instruct patients to notify their physician if they are breast feeding or intend to breast feed during therapy. | ||
|alcohol=*Since | |alcohol=*Since clobazam has a [[central nervous system]] (CNS) depressant effect, patients or their caregivers should be cautioned against simultaneous use with other CNS depressant drugs or [[alcohol]], and cautioned that the effects of other CNS depressant drugs or alcohol may be potentiated. | ||
|brandNames=* | |brandNames=*ONFI<ref>{{cite web|url=http://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=de03bd69-2dca-459c-93b4-541fd3e9571c|title= clobazam- clobazam tablet | ||
clobazam- clobazam suspension}} </ref> | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 1.png | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 2.png | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 3.png | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 4.png | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 5.png | |||
}} | |||
{{LabelImage | |||
|fileName=Clobazam pack 6.png | |||
}} | }} | ||
Latest revision as of 14:37, 22 January 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Stefano Giannoni [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Clobazam is a Benzodiazepine that is FDA approved for the treatment of seizures associated with Lennox-Gastaut syndrome (LGS) in patients 2 years of age or older. Common adverse reactions include constipation, somnolence or sedation, pyrexia, lethargy, and drooling.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Seizures associated with Lennox-Gastaut syndrome (LGS)
- A daily dose of clobazam greater than 5 mg should be administered in divided doses twice daily
- 5 mg daily dose can be administered as a single dose.
- Dose patients according to body weight.
- Do not proceed with dose escalation more rapidly than weekly, because serum concentrations of clobazam and its active metabolite require 5 and 9 days, respectively, to reach steady-state.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Clobazam in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Clobazam in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Seizures associated with Lennox-Gastaut syndrome (LGS) (2 years of age or older)
- A daily dose of clobazam greater than 5 mg should be administered in divided doses twice daily
- 5 mg daily dose can be administered as a single dose.
- Dose patients according to body weight.
- Do not proceed with dose escalation more rapidly than weekly, because serum concentrations of clobazam and its active metabolite require 5 and 9 days, respectively, to reach steady-state.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Clobazam in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Clobazam in pediatric patients.
Contraindications
- Clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients.
- Hypersensitivity reactions have included serious dermatological reactions.
Warnings
Somnolence or Sedation
- Clobazam causes somnolence and sedation.
- In clinical trials, somnolence or sedation was reported at all effective doses and was dose-related.
- In general, somnolence and sedation begin within the first month of treatment and may diminish with continued treatment.
- Prescribers should monitor patients for somnolence and sedation, particularly with concomitant use of other central nervous system depressants.
- Prescribers should caution patients against engaging in hazardous activities requiring mental alertness, such as operating dangerous machinery or motor vehicles, until the effect of clobazam is known.
Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants
- Since clobazam has a central nervous system (CNS) depressant effect, patients or their caregivers should be cautioned against simultaneous use with other CNS depressant drugs or alcohol, and cautioned that the effects of other CNS depressant drugs or alcohol may be potentiated.
Withdrawal Symptoms
- Abrupt discontinuation of clobazam should be avoided.
- Clobazam should be tapered by decreasing the dose every week by 5-10 mg/day until discontinuation.
- Withdrawal symptoms (Benzodiazepine withdrawal syndrome) occurred following abrupt discontinuation of clobazam; the risk of withdrawal symptoms is greater with higher doses.
- As with all antiepileptic drugs, clobazam should be withdrawn gradually to minimize the risk of precipitating seizures, seizure exacerbation, or status epilepticus.
- Withdrawal symptoms (e.g., convulsions, psychosis, hallucinations, behavioral disorder, tremor, and anxiety) have been reported following abrupt discontinuance of benzodiazepines.
- The more severe withdrawal symptoms have usually been limited to patients who received excessive doses over an extended period of time, followed by an abrupt discontinuation.
- Generally milder withdrawal symptoms (e.g., dysphoria, anxiety, and insomnia) have been reported following abrupt discontinuance of benzodiazepines taken continuously at therapeutic doses for several months.
Serious Dermatological Reactions
- Serious skin reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported with clobazam in both children and adults during the post-marketing period.
- Patients should be closely monitored for signs or symptoms of SJS/TEN, especially during the first 8 weeks of treatment initiation or when re-introducing therapy.
- Clobazam should be discontinued at the first sign of rash, unless the rash is clearly not drug-related.
- If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered.
Physical and Psychological Dependence
- Patients with a history of substance abuse should be under careful surveillance when receiving clobazam or other psychotropic agents because of the predisposition of such patients to habituation and dependence.
Suicidal Behavior and Ideation
- Antiepileptic drugs (AEDs), including clobazam, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication.
- Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
- Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted relative risk 1.8, 95% cclobazamdence interval [CI]: 1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED treated patients was 0.43%, compared to 0.24% among 16,029 placebo treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated.
- There were four suicides in drug treated patients in the trials and none in placebo treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
- The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed.
- Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
- The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed.
- The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
- The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
- Anyone considering prescribing clobazam or any other AED must balance the risk of suicidal thoughts or behavior with the risk of untreated illness.
- Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior.
- Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
- Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm.
- Behaviors of concern should be reported immediately to healthcare providers.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- During its development for the adjunctive treatment of seizures associated with LGS, clobazam was administered to 333 healthy volunteers and 300 patients with a current or prior diagnosis of LGS, including 197 patients treated for 12 months or more.
- The conditions and duration of exposure varied greatly and included single- and multiple-dose clinical pharmacology studies in healthy volunteers and two double-blind studies in patients with LGS (Study 1 and 2). Only Study 1 included a placebo group, allowing comparison of adverse reaction rates on clobazam at several doses to placebo.
Adverse Reactions Leading to Discontinuation in an LGS Placebo Controlled Clinical Trial (Study 1)
- The adverse reactions associated with clobazam treatment discontinuation in ≥1% of patients in decreasing order of frequency included lethargy, somnolence, ataxia, aggression, fatigue, and insomnia.
Most Common Adverse Reactions in an LGS Placebo Controlled Clinical Trial (Study 1) Table 3 lists the adverse reactions that occurred in ≥5% of clobazam treated patients (at any dose), and at a rate greater than placebo treated patients, in the randomized, double-blind, placebo-controlled, parallel group clinical study of adjunctive AED therapy for 15 weeks (Study 1).
Postmarketing Experience
These reactions are reported voluntarily from a population of uncertain size; therefore, it is not possible to estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions are categorized by system organ class.
Blood Disorders
Eye Disorders
Gastrointestinal Disorders
- Abdominal distention
General Disorders and Administration Site Conditions
Investigations
- Hepatic enzyme increased
Musculoskeletal
Psychiatric Disorders
- Agitation
- Anxiety
- Apathy
- Confusional state
- Depression
- Delirium
- Delusion
- Hallucination
Renal and Urinary Disorders
Respiratory Disorders
Skin and Subcutaneous Tissue Disorders
- Rash
- Urticaria
- Angioedema
- Facial and lip edema
Drug Interactions
Effect of clobazam on Other Drugs
Hormonal Contraceptives
- Clobazam is a weak CYP3A4 inducer.
- As some hormonal contraceptives are metabolized by CYP3A4, their effectiveness may be diminished when given with clobazam.
- Additional non-hormonal forms of contraception are recommended when using clobazam.
Drugs Metabolized by CYP2D6
Effect of Other Drugs on clobazam
- Strong and moderate inhibitors of CYP2C19
- Strong and moderate inhibitors of CYP2C19 may result in increased exposure to N-desmethylclobazam, the active metabolite of clobazam.
- This may increase the risk of dose-related adverse reactions.
- Dosage adjustment of clobazam may be necessary when co-administered with strong CYP2C19 inhibitors (e.g., fluconazole, fluvoxamine, ticlopidine) or moderate CYP2C19 inhibitors (e.g., omeprazole).
CNS Depressants and Alcohol
- Concomitant use of clobazam with other CNS depressants may increase the risk of sedation and somnolence.
- Alcohol, as a CNS depressant, will interact with clobazam in a similar way and also increases clobazam's maximum plasma exposure by approximately 50%. Therefore, caution patients or their caregivers against simultaneous use with other CNS depressant drugs or alcohol, and caution that the effects of other CNS depressant drugs or alcohol may be potentiated.
Use in Specific Populations
Pregnancy
- There are no adequate and well-controlled studies of clobazam in pregnant women.
- In animal studies, administration of clobazam during pregnancy resulted in developmental toxicity, including increased incidences of fetal malformations, at plasma exposures for clobazam and its major active metabolite, N-desmethylclobazam, below those expected at therapeutic doses in patients. Clobazam should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Available human data on the risk of teratogenicity associated with benzodiazepines are inconclusive.
- There is insufficient evidence in humans to assess the effect of benzodiazepine exposure during pregnancy on neurodevelopment.
- Administration of benzodiazepines immediately prior to or during childbirth can result in a syndrome of hypothermia, hypotonia, respiratory depression, and difficulty feeding.
- In addition, infants born to mothers who have taken benzodiazepines during the later stages of pregnancy can develop dependence, and subsequently withdrawal, during the postnatal period.
- Data for other benzodiazepines suggest the possibility of adverse developmental effects (including long-term effects on neurobehavioral and immunological function) in animals following prenatal exposure to benzodiazepines at clinically relevant doses.
- In a study in which clobazam (150, 450, or 750 mg/kg/day) was orally administered to pregnant rats throughout the period of organogenesis, embryofetal mortality and incidences of fetal skeletal variations were increased at all doses.
- The low effect dose for embryofetal developmental toxicity in rats (150 mg/kg/day) was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, lower than those in humans at the maximum recommended human dose (MRHD) of 40 mg/day.
- Oral administration of clobazam (10, 30, or 75 mg/kg/day) to pregnant rabbits throughout the period of organogenesis resulted in decreased fetal body weights, and increased incidences of fetal malformations (visceral and skeletal) at the mid and high doses, and an increase in embryofetal mortality at the high dose.
- Incidences of fetal variations were increased at all doses.
- The highest dose tested was associated with maternal toxicity (ataxia and decreased activity).
- The low effect dose for embryofetal developmental toxicity in rabbits (10 mg/kg/day) was associated with plasma exposures for clobazam and N-desmethylclobazam lower than those in humans at the MRHD.
- Oral administration of clobazam (50, 350, or 750 mg/kg/day) to rats throughout pregnancy and lactation resulted in increased embryofetal mortality at the high dose, decreased pup survival at the mid and high doses and alterations in offspring behavior (locomotor activity) at all doses. The low effect dose for adverse effects on pre- and postnatal development in rats (50 mg/kg/day) was associated with plasma exposures for clobazam and N-desmethylclobazam lower than those in humans at the MRHD.
Pregnancy Category (AUS): C
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Clobazam in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Clobazam during labor and delivery.
Nursing Mothers
- Clobazam is excreted in human milk.
- Because of the potential for serious adverse reactions in nursing infants from clobazam, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness in patients less than 2 years of age have not been established.
- In a study in which clobazam (4, 36, or 120 mg/kg/day) was orally administered to rats during the juvenile period of development (postnatal days 14 to 48), adverse effects on growth (decreased bone density and bone length) and behavior (altered motor activity and auditory startle response; learning deficit) were observed at the high dose.
- The effect on bone density, but not on behavior, was reversible when drug was discontinued.
- The no-effect level for juvenile toxicity (36 mg/kg/day) was associated with plasma exposures (AUC) to clobazam and its major active metabolite, N-desmethylclobazam, less than those expected at therapeutic doses in pediatric patients.
Geriatic Use
- Plasma concentrations at any given dose are generally higher in the elderly: proceed slowly with dose escalation.
- The starting dose should be 5 mg/day for all elderly patients.
- Then titrate elderly patients according to weight, but to half the dose presented in Table 1, as tolerated.
- If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on weight) may be started on day 21.
- Clinical studies of clobazam did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. However, elderly subjects appear to eliminate clobazam more slowly than younger subjects based on population pharmacokinetic analysis. For these reasons, the initial dose in elderly patients should be 5 mg/day.
Gender
- Population pharmacokinetic analyses showed no difference in the clearance of clobazam between women and men.
Race
- Population pharmacokinetic analyses including Caucasian (75%), African American (15%), and Asian (9%) subjects showed that there is no evidence of clinically significant effect of race on the clearance of clobazam.
Renal Impairment
- No dose adjustment is required for patients with mild and moderate renal impairment.
- There is no experience with clobazam in patients with severe renal impairment or end stage renal disease (ESRD).
- It is not known if clobazam or its active metabolite, N-desmethylclobazam, is dialyzable.
Hepatic Impairment
- Clobazam is hepatically metabolized; however, there are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam. *For this reason, proceed slowly with dosing escalations.
- For patients with mild to moderate hepatic impairment (Child-Pugh score 5-9), the starting dose should be 5 mg/day in both weight groups.
- Then titrate patients according to weight, but to half the dose presented in Table 1, as tolerated.
- If necessary and based upon clinical response, start an additional titration on day 21 to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group).
- There is inadequate information about metabolism of clobazam in patients with severe hepatic impairment.
- Therefore no dosing recommendation in those patients can be given.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Clobazam in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Clobazam in patients who are immunocompromised.
Dosage Adjustments in CYP2C19 Poor Metabolizers
- In CYP2C19 poor metabolizers, levels of N-desmethylclobazam, clobazam's active metabolite, will be increased. Therefore, in patients known to be CYP2C19 poor metabolizers, the starting dose should be 5 mg/day and dose titration should proceed slowly according to weight, but to half the dose presented in Table 1, as tolerated.
- If necessary and based upon clinical response, an additional titration to the maximum dose (20 mg/day or 40 mg/day, depending on the weight group) may be started on day 21.
Administration and Monitoring
Administration
- Oral
Important Administration Instructions
- Instruct patients to read the "Instructions for Use" carefully for complete directions on how to properly dose and administer clobazam oral suspension.
clobazam Tablet Oral Administration
- Clobazam tablets can be taken with or without food.
- Clobazam tablets can be administered whole, broken in half along the score, or crushed and mixed in applesauce.
Clobazam Oral Suspension Oral Administration
- Clobazam oral suspension can be taken with or without food.
- Shake clobazam Oral Suspension well before every administration.
- When administering the oral suspension, use only the oral dosing syringe provided with the product.
- Each carton includes two syringes, but only one syringe should be used for dosing.
- The second oral syringe is reserved as a replacement in case the first syringe is damaged or lost.
- Insert the provided adapter firmly into the neck of the bottle before first use and keep the adapter in place for the duration of the usage of the bottle. *To withdraw the dose, insert the dosing syringe into the adapter and invert the bottle then slowly pull back the plunger to prescribed dose.
- After removing the syringe from the bottle adapter, slowly squirt clobazam Oral Suspension into the corner of the patient's mouth.
- Replace the cap after each use.
- The cap fits over the adapter when the adapter is properly placed.
Monitoring
- Monitor for central nervous system (CNS) depression.
- Monitor patients with a history of substance abuse for signs of habituation and dependence.
- Monitor for suicidal thoughts or behaviors.
- Monitored for signs or symptoms of SJS/TEN, especially during the first 8 weeks of treatment initiation or when re-introducing therapy.
IV Compatibility
There is limited information regarding the compatibility of Clobazam and IV administrations.
Overdosage
Signs and Symptoms of Overdosage
- Overdose and intoxication with benzodiazepines, including clobazam, may lead to CNS depression, associated with drowsiness, confusion and lethargy, possibly progressing to ataxia, respiratory depression, hypotension, and, rarely, coma or death.
- The risk of a fatal outcome is increased in cases of combined poisoning with other CNS depressants, including alcohol.
Management of Overdosage
- The management of clobazam overdose may include gastric lavage and/or administration of activated charcoal, intravenous fluid replenishment, early control of airway and general supportive measures, in addition to monitoring level of consciousness and vital signs.
- Hypotension can be treated by replenishment with plasma substitutes and, if necessary, with sympathomimetic agents.
- The efficacy of supplementary administration of physostigmine (a cholinergic agent) or of flumazenil (a benzodiazepine antagonist) in clobazam overdose has not been assessed.
- The administration of flumazenil in cases of benzodiazepine overdose can lead to withdrawal and adverse reactions. Its use in patients with epilepsy is typically not recommended.
Pharmacology
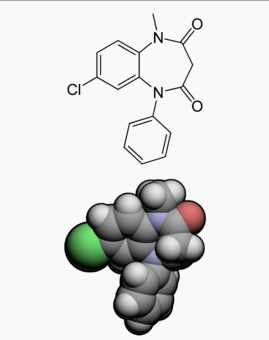 | |
| Clinical data | |
|---|---|
| Trade names | Frisium, Urbanol, clobazam |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| [[Regulation of therapeutic goods |Template:Engvar data]] | |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 90% |
| Protein binding | 83% |
| Metabolism | Hepatic |
| Elimination half-life | 18 h |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C16H13ClN2O2 |
| Molar mass | 300.74 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Mechanism of Action
- The exact mechanism of action for clobazam, a 1,5-benzodiazepine, is not fully understood but is thought to involve potentiation of GABAergic neurotransmission resulting from binding at the benzodiazepine site of the GABAA receptor.
Structure
- Clobazam is a white or almost white, crystalline powder with a slightly bitter taste; is slightly soluble in water, sparingly soluble in ethanol, and freely soluble in methylene chloride.
- The melting range of clobazam is from 182ºC to 185ºC.
- The molecular formula is C16H13O2N2Cl and the molecular weight is 300.7.
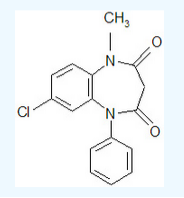
Pharmacodynamics
Effects on Electrocardiogram
- The effect of clobazam 20 mg and 80 mg administered twice daily on QTc interval was evaluated in a randomized, evaluator blinded, placebo-, and active-controlled (moxifloxacin 400 mg) parallel thorough QT study in 280 healthy subjects.
- In a study with demonstrated ability to detect small effects, the upper bound of the one-sided 95% cclobazamdence interval for the largest placebo adjusted, baseline-corrected QTc based on the Fridericia correction method was below 10 ms, the threshold for regulatory concern.
- Thus, at a dose two times the maximum recommended dose, clobazam did not prolong the QTc interval to any clinically relevant extent.
Pharmacokinetics
- The peak plasma levels (Cmax) and the area under the curve (AUC) of clobazam are dose-proportional over the dose range of 10-80 mg following single- or multiple-dose administration of clobazam.
- Based on a population pharmacokinetic analysis, the pharmacokinetics of clobazam are linear from 5-160 mg/day.
- Clobazam is converted to N-desmethylclobazam which has about 1/5 the activity of clobazam.
- The estimated mean elimination half-lives (t1/2) of clobazam and N-desmethylclobazam were 36-42 hours and 71-82 hours, respectively.
Absorption
- Clobazam is rapidly and extensively absorbed following oral administration. *The time to peak concentrations (Tmax) of clobazam tablets under fasted conditions ranged from 0.5 to 4 hours after single- or multiple-dose administrations.
- The relative bioavailability of clobazam tablets compared to an oral solution is approximately 100%.
- After single dose administration of the oral suspension under fasted conditions, the Tmax ranged from 0.5 to 2 hours.
- Based on exposure (Cmax and AUC) of clobazam, clobazam tablets and suspension were shown to have similar bioavailability under fasted conditions.
- The administration of clobazam tablets with food or when crushed in applesauce does not affect absorption.
- Although not studied, the oral bioavailability of the oral suspension is unlikely to be affected under fed conditions.
Distribution
- Clobazam is lipophilic and distributes rapidly throughout the body.
- The apparent volume of distribution at steady state was approximately 100 L. *The in vitro plasma protein binding of clobazam and N-desmethylclobazam is approximately 80-90% and 70%, respectively.
Metabolism and Excretion
- Clobazam is extensively metabolized in the liver, with approximately 2% of the dose recovered in urine and 1% in feces as unchanged drug.
- The major metabolic pathway of clobazam involves N-demethylation, primarily by CYP3A4 and to a lesser extent by CYP2C19 and CYP2B6.
- N-desmethylclobazam, an active metabolite, is the major circulating metabolite in humans, and at therapeutic doses, plasma concentrations are 3-5 times higher than those of the parent compound.
- Based on animal and in vitro receptor binding data, estimates of the relative potency of N-desmethylclobazam compared to parent compound range from 1/5 to equal potency.
- N-desmethylclobazam is extensively metabolized, mainly by CYP2C19.
- N-desmethylclobazam and its metabolites comprise ~94% of the total drug-related components in urine.
- Following a single oral dose of radiolabeled drug, approximately 11% of the dose was excreted in the feces and approximately 82% was excreted in the urine.
- The polymorphic CYP2C19 is the major contributor to the metabolism of the pharmacologically active N-desmethylclobazam.
- In CYP2C19 poor metabolizers, levels of N-desmethylclobazam were 5-fold higher in plasma and 2- to 3-fold higher in the urine than in CYP2C19 extensive metabolizers.
Pharmacokinetics in Specific Populations
Age
- Population pharmacokinetic analyses showed that the clearance of clobazam is lower in elderly subjects compared to other age groups (ages 2 to 64).
- Dosing should be adjusted in the elderly.
Sex
- Population pharmacokinetic analyses showed no difference in the clearance of clobazam between women and men.
Race
- Population pharmacokinetic analyses including Caucasian (75%), African American (15%), and Asian (9%) subjects showed that there is no evidence of clinically significant effect of race on the clearance of clobazam.
Renal Impairment
- The effect of renal impairment on the pharmacokinetics of clobazam was evaluated in patients with mild (creatinine clearance [CLCR] >50 to 80 mL/min; N=6) and moderate (CLCR=30 to 50 mL/min; N=6) renal dysfunction, with matching healthy controls (N=6), following administration of multiple doses of clobazam 20 mg/day.
- There were insignificant changes in Cmax (3-24%) and AUC (≤13%) for clobazam or N-desmethylclobazam in patients with mild or moderate renal impairment compared to patients with normal renal function.
- Patients with severe renal impairment or ESRD were not included in this study.
Hepatic Impairment
- There are limited data to characterize the effect of hepatic impairment on the pharmacokinetics of clobazam.
- In a small study, the pharmacokinetics of a 20 mg single oral dose of clobazam in 9 patients with liver impairment were compared to healthy controls (N=6).
- The Cmax and the mean plasma clearance of clobazam, as well as the Cmax of N-desmethylclobazam, showed no significant change compared to the healthy controls.
- The AUC values of N-desmethylclobazam in these patients were not available. Adjust dosage in patients with hepatic impairment.
Drug Interaction Studies
In vitro studies
- Clobazam did not inhibit: CYP1A2, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, UGT1A1, UGT1A4, UGT1A6, or UGT2B4 in vitro.
- N-desmethylclobazam showed weak inhibition of: CYP2C9, UGT1A4, UGT1A6 and UGT2B4.
- Clobazam and N-desmethylclobazam did not significantly increase CYP1A2 or CYP2C19 activities, but did induce CYP3A4 activity in a concentration-dependent manner.
- Clobazam and N-desmethylclobazam also increased UGT1A1 mRNA but at concentrations much higher than therapeutic levels.
- The potential for clobazam or N-desmethylclobazam to induce CYP2B6and CYP2C8 has not been evaluated.
- Clobazam and N-desmethylclobazam do not inhibit P-glycoprotein (P-gp), but are P-gp substrates.
In vivo studies
Potential for clobazam to Affect Other Drugs
- The effect of repeated 40 mg once-daily doses of clobazam on the pharmacokinetic profiles of single-dose dextromethorphan (CYP2D6 substrate), midazolam (CYP3A4 substrate), caffeine (CYP1A2 substrate), and tolbutamide (CYP2C9 substrate), was studied when these probe substrates were given as a drug cocktail (N=18).
- Clobazam increased AUC and Cmax of dextromethorphan by 90% and 59%, respectively, reflecting its inhibition of CYP2D6 in vivo.
- Drugs metabolized by CYP2D6 may require dose adjustment when used with clobazam.
- Clobazam decreased the AUC and Cmax of midazolam by 27% and 24%, respectively, and increased the AUC and Cmax of the metabolite 1-hydroxymidazolam by 4-fold and 2-fold, respectively.
- This level of induction does not call for dosage adjustment of drugs that are primarily metabolized by CYP3A4 when used concomitantly with clobazam.
- Some hormonal contraceptives are metabolized by CYP3A4 and their effectiveness may be diminished when given with clobazam. Repeated clobazam doses had no effect on caffeine and tolbutamide.
- A population pharmacokinetic analysis indicated clobazam did not affect the exposure of valproic acid (a CYP2C9/2C19 substrate) or lamotrigine (a UGT substrate).
Potential for Other Drugs to Affect clobazam
- Co-administration of ketoconazole (a strong CYP3A4 inhibitor) 400 mg once-daily for 5 days increased clobazam AUC by 54%, with an insignificant effect on clobazam Cmax.
- There was no significant change in AUC and Cmax of N-desmethylclobazam (N=18).
- Strong (e.g., fluconazole, fluvoxamine, ticlopidine) and moderate (e.g., omeprazole) inhibitors of CYP2C19 may result in up to a 5-fold increase in exposure to N-desmethylclobazam, the active metabolite of clobazam, based on extrapolation from pharmacogenomic data.
- Dosage adjustment of clobazam may be necessary when co-administered with strong or moderate CYP2C19 inhibitors.
- The effects of concomitant antiepileptic drugs that are CYP3A4 inducers (phenobarbital, phenytoin, and carbamazepine), CYP2C9 inducers (valproic acid, phenobarbital, phenytoin, and carbamazepine), and CYP2C9 inhibitors (felbamate and oxcarbazepine) were evaluated using data from clinical trials.
- Results of population pharmacokinetic analysis show that these concomitant antiepileptic drugs did not significantly alter the pharmacokinetics of clobazam or N-desmethylclobazam at steady-state.
- Alcohol has been reported to increase the maximum plasma exposure of clobazam by approximately 50%. Alcohol may have additive CNS depressant effects when taken with clobazam.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
- The carcinogenic potential of clobazam has not been adequately assessed.
- In a limited study in rats, oral administration of clobazam (4, 20, and 100 mg/kg/day) for 2 years resulted in an increased incidence of thyroid follicular cell adenomas in males at the high dose.
Mutagenesis
- Clobazam and the major active metabolite, N-desmethylclobazam, were negative for genotoxicity, based on data from a battery of in vitro (bacteria reverse mutation, mammalian clastogenicity) and in vivo (mouse micronucleus) assays.
Impairment of Fertility
- In a study in which clobazam (50, 350, or 750 mg/kg/day) was orally administered to male and female rats prior to and during mating and continuing in females to gestation day 6, increases in abnormal sperm and pre-implantation loss were observed at the highest dose tested.
- The no effect level for fertility and early embryonic development in rats was associated with plasma exposures (AUC) for clobazam and its major active metabolite, N-desmethylclobazam, less than those in humans at the maximum recommended human dose of 40 mg/day.
Clinical Studies
The effectiveness of clobazam for the adjunctive treatment of seizures associated with Lennox-Gastaut syndrome was established in two multicenter controlled studies (Study 1 and Study 2). Both studies were similar in terms of disease characteristics and concomitant AED treatments. The most common concomitant AED treatments at baseline included: valproate, lamotrigine, levetiracetam, and topiramate.
Study 1
Study 1 (N=238) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and 12-week maintenance period. Patients age 2-54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of clobazam according to Table 5.
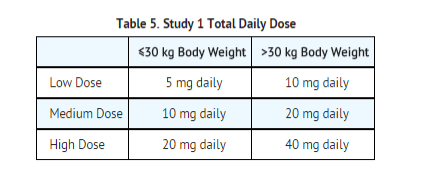
Doses above 5 mg/day were administered in two divided doses. The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to 12-week maintenance period. The pre-dosing baseline mean weekly drop seizure frequency was 98, 100, 61, and 105 for the placebo, low-, medium-, and high-dose groups, respectively. Figure 1 presents the mean percent reduction in weekly drop seizures from this baseline. All dose groups of clobazam were statistically superior (p≤0.05) to the placebo group. This effect appeared to be dose dependent.
Figure 2 shows changes from baseline in weekly drop seizure frequency by category for patients treated with clobazam and placebo in Study 1. Patients in whom the seizure frequency increased are shown at left as "worse." Patients in whom the seizure frequency decreased are shown in five categories.
There was no evidence that tolerance to the therapeutic effect of clobazam developed during the 3-month maintenance period.
Study 2
Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose clobazam, consisting of a 4-week baseline period followed by a 3-week titration period and 4-week maintenance period. Patients age 2-25 years with a current or prior diagnosis of LGS were stratified by weight, then randomized to either a low or high dose of clobazam, and then entered a 3-week titration period.
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to the 4-week maintenance period.
A statistically significantly greater reduction in seizure frequency was observed in the high-dose group compared to the low-dose group (median percent reduction of 93% vs 29%; p<0.05).
How Supplied
Clobazam- Tablets
Each clobazam tablet contains 10 mg or 20 mg of clobazam.
- It is a white to off-white, oval tablet with a functional score on one side and either a "1" and "0" or a "2" and "0" debossed on the other side.
- NDC 67386-314-01: 10 mg scored tablet, Bottles of 100
- NDC 67386-315-01: 20 mg scored tablet, Bottles of 100
Clobazam- Oral suspension
- Clobazam oral suspension is a berry flavored off-white liquid supplied in a bottle with child-resistant closure.
- The oral suspension is packaged with a dispenser set which contains two calibrated oral dosing syringes and a bottle adapter.
- NDC 67386-313-21: 2.5 mg/mL supplied in a bottle containing 120 mL of suspension.
Storage
Clobazam Tablets
- Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature.
Clobazam Oral suspension
- Store and dispense clobazam oral suspension in its original bottle in an upright position.
- Use within 90 days of first opening the bottle, then discard any remainder
- Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature.
Images
Drug Images
{{#ask: Page Name::Clobazam |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
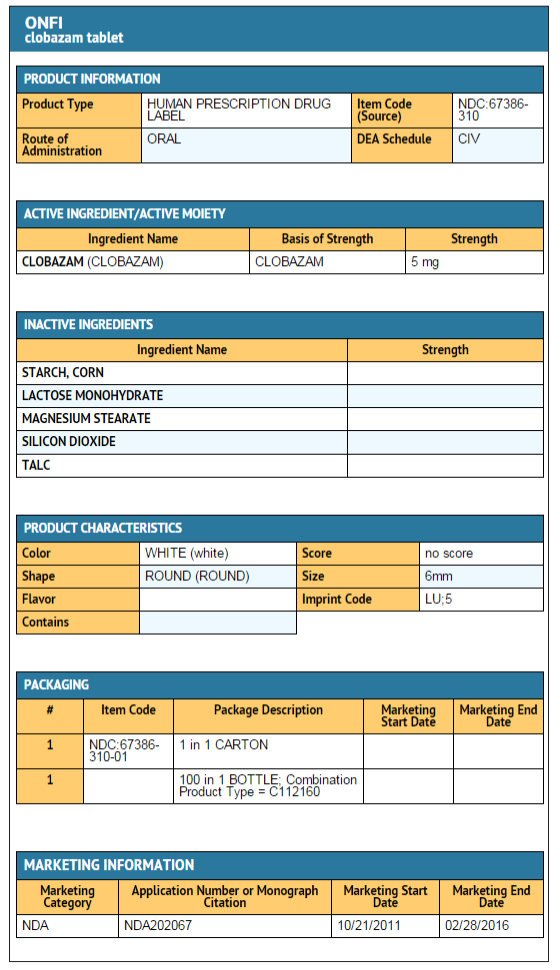
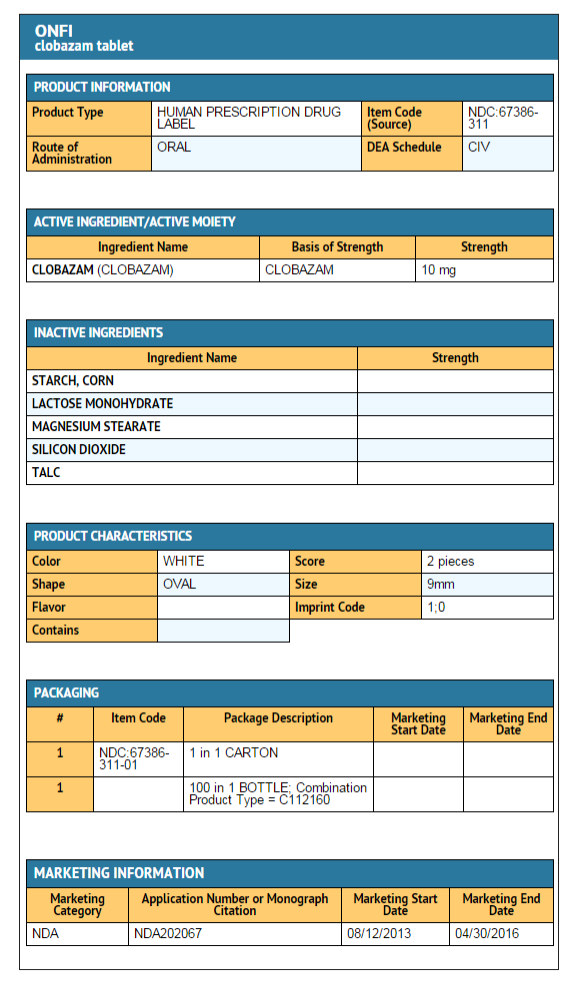
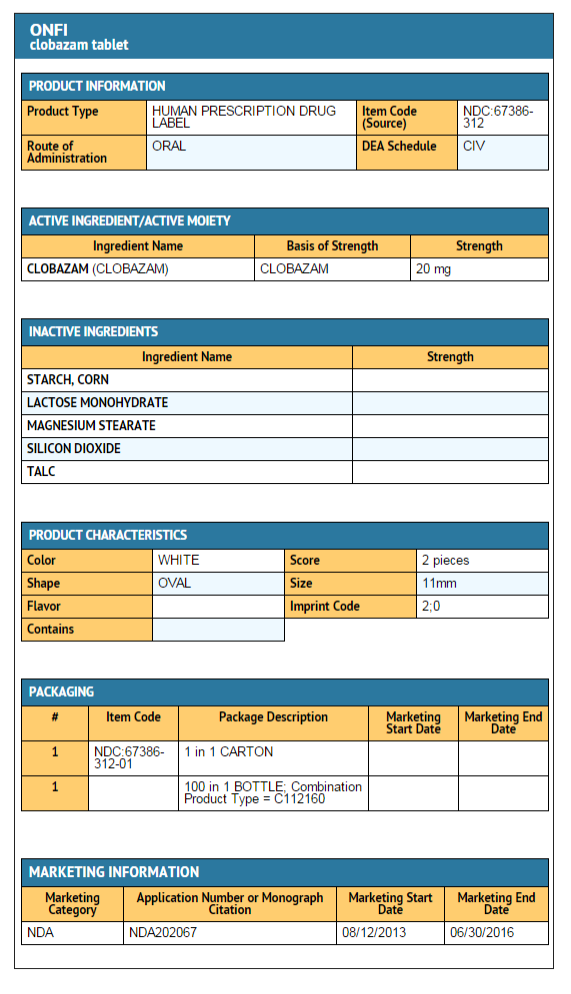
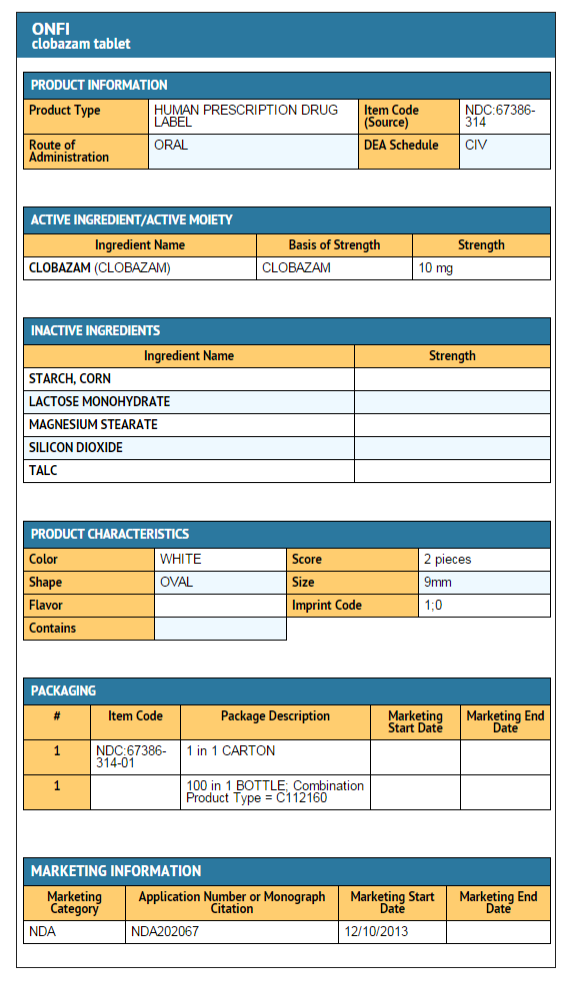
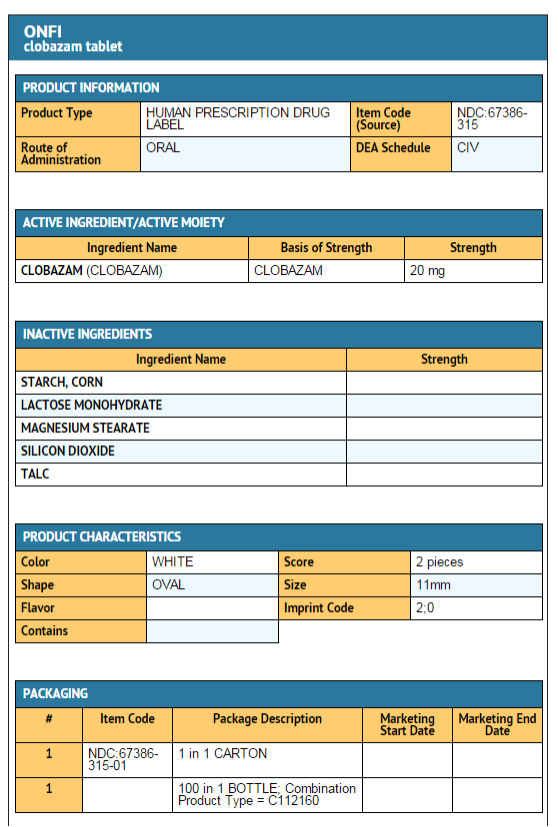
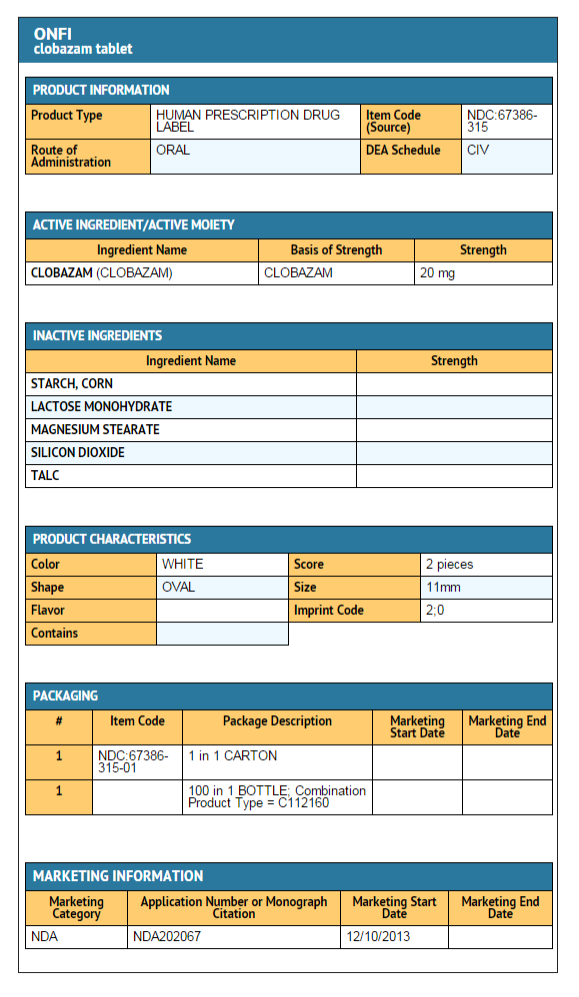
{{#ask: Label Page::Clobazam |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Hypersensitivity
Inform patients or caregivers that clobazam is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients.
Somnolence or Sedation
Advise patients or caregivers to check with their healthcare provider before clobazam is taken with other CNS depressants such as other benzodiazepines, opioids, tricyclic antidepressants, sedating antihistamines, or alcohol.
If applicable, caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that clobazam does not affect them adversely (e.g., impair judgment, thinking or motor skills).
Increasing or Decreasing the clobazam Dose
Inform patients or caregivers to consult their healthcare provider before increasing the clobazam dose or abruptly discontinuing clobazam. Advise patients or caregivers that abrupt withdrawal of AEDs may increase their risk of seizure.
Interactions with Hormonal Contraceptives
Counsel women to also use non-hormonal methods of contraception when clobazam is used with hormonal contraceptives and to continue these alternative methods for 28 days after discontinuing clobazam to ensure contraceptive reliability.
Serious Dermatological Reactions
Advise patients or caregivers that serious skin reactions have been reported in patients taking clobazam. Serious skin reactions, including SJS/TEN, may need to be treated in a hospital and may be life-threatening. If a skin reaction occurs while taking clobazam, patients or caregivers should consult with healthcare providers immediately.
Suicidal Thinking and Behavior
Counsel patients, their caregivers, and their families that AEDs, including clobazam, may increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts of self-harm. Patients should report behaviors of concern immediately to healthcare providers.
Use in Pregnancy
Instruct patients to notify their healthcare provider if they become pregnant or intend to become pregnant during therapy.
Use in Nursing
Instruct patients to notify their physician if they are breast feeding or intend to breast feed during therapy.
Precautions with Alcohol
- Since clobazam has a central nervous system (CNS) depressant effect, patients or their caregivers should be cautioned against simultaneous use with other CNS depressant drugs or alcohol, and cautioned that the effects of other CNS depressant drugs or alcohol may be potentiated.
Brand Names
- ONFI[1]
Look-Alike Drug Names
There is limited information regarding Clobazam Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "clobazam- clobazam tablet clobazam- clobazam suspension". line feed character in
|title=at position 27 (help)
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 1.png
}}
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 2.png
}}
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 3.png
}}
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 4.png
}}
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 5.png
}}
{{#subobject:
|Label Page=Clobazam |Label Name=Clobazam pack 6.png
}}