Chronic cholecystitis surgery: Difference between revisions
No edit summary |
Usama Talib (talk | contribs) |
||
| (19 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Cholecystitis}} | {{Cholecystitis}} | ||
{{CMG}}; {{AE}} {{MMF}} | |||
==Overview== | ==Overview== | ||
Gallbladder removal, [[cholecystectomy]], can be accomplished by the open surgery or a [[laparoscopic]] procedure. Laparoscopic cholecystectomy is the operation of choice in uncomplicated calculous cholecystitis. Open cholecystectomy may be performed in complicated cases or when trained/skilled personal for laparoscopic procedure is not available. Supportive measures are instituted in the meantime to prepare the patient for surgery. These measures include fluid resuscitation and [[antibiotic]]s. Antibiotic regimens usually consist of a broad spectrum [[cephalosporin]] such as [[ceftriaxone]] and an antibacterial with good cover against [[anaerobic organism|anaerobic bacteria]], such as [[metronidazole]]. | |||
==Surgery== | ==Surgery== | ||
Removal of the gallbladder may be done by open surgery or a [[laparoscopic]] approach. Laparoscopic cholecystectomy is the procedure of choice in uncomplicated calculous cholecystitis. Open cholecystectomy may be performed in complicated cases or when trained or skilled personal for laparoscopic procedure is not available. Supportive measures such as fluid resuscitation and [[antibiotic]]s are instituted in the meantime to prepare the patient for surgery. Antibiotic regimens usually consist of a broad spectrum [[cephalosporin]] such as [[ceftriaxone]] and an antibacterial with good cover against [[anaerobic organism|anaerobic bacteria]], such as [[metronidazole]].<ref name="pmid9511287">{{cite journal |vauthors=Movchun AA, Koloss OE, Oppel' TA, Abdullaeva UA |title=[Surgical treatment of chronic calculous cholecystitis and its complications] |language=Russian |journal=Khirurgiia (Mosk) |volume= |issue=1 |pages=8–10 |year=1998 |pmid=9511287 |doi= |url=}}</ref><ref name="pmid11432016">{{cite journal |vauthors=Fletcher DR |title=Gallstones. Modern management |journal=Aust Fam Physician |volume=30 |issue=5 |pages=441–5 |year=2001 |pmid=11432016 |doi= |url=}}</ref> | |||
===Laparoscopic cholecystectomy=== | |||
Laparoscopic cholecystectomy is a minimally invasive surgical procedure and has various indications in addition to the chronic cholecystitis. There are two main types of procedures used for the laparoscopic [[cholecystectomy]] ; Single-incision laparoscopic [[cholecystectomy]] (SILC) and conventional multiport laparoscopic [[cholecystectomy]] (CMLC).<ref name="pmid23557447">{{cite journal |vauthors=Sato N, Yabuki K, Shibao K, Mori Y, Tamura T, Higure A, Yamaguchi K |title=Risk factors for a prolonged operative time in a single-incision laparoscopic cholecystectomy |journal=HPB (Oxford) |volume=16 |issue=2 |pages=177–82 |year=2014 |pmid=23557447 |pmc=3921014 |doi=10.1111/hpb.12100 |url=}}</ref><ref name="pmid20607556">{{cite journal |vauthors=Antoniou SA, Pointner R, Granderath FA |title=Single-incision laparoscopic cholecystectomy: a systematic review |journal=Surg Endosc |volume=25 |issue=2 |pages=367–77 |year=2011 |pmid=20607556 |doi=10.1007/s00464-010-1217-5 |url=}}</ref><ref name="pmid22819642">{{cite journal |vauthors=Leung D, Yetasook AK, Carbray J, Butt Z, Hoeger Y, Denham W, Barrera E, Ujiki MB |title=Single-incision surgery has higher cost with equivalent pain and quality-of-life scores compared with multiple-incision laparoscopic cholecystectomy: a prospective randomized blinded comparison |journal=J. Am. Coll. Surg. |volume=215 |issue=5 |pages=702–8 |year=2012 |pmid=22819642 |doi=10.1016/j.jamcollsurg.2012.05.038 |url=}}</ref><ref name="pmid22767084">{{cite journal |vauthors=Pisanu A, Reccia I, Porceddu G, Uccheddu A |title=Meta-analysis of prospective randomized studies comparing single-incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC) |journal=J. Gastrointest. Surg. |volume=16 |issue=9 |pages=1790–801 |year=2012 |pmid=22767084 |doi=10.1007/s11605-012-1956-9 |url=}}</ref> | |||
*Single-incision [[laparoscopic cholecystectomy]] (SILC) | |||
**As compared to CMLC, SILC has the following features: | |||
***Improved cosmetic results | |||
***Decreased postoperative pain | |||
***Increased operative time | |||
***Increased intraoperative blood loss | |||
*Conventional multiport laparoscopic [[cholecystectomy]] (CMLC) | |||
**As compared to SILC, CMLC has the following features: | |||
***Decreased operative time | |||
***Decreased intra-operative blood loss | |||
====Indications==== | |||
*Indications of laparoscopic cholecystitis are:<ref name="pmid9511287">{{cite journal |vauthors=Movchun AA, Koloss OE, Oppel' TA, Abdullaeva UA |title=[Surgical treatment of chronic calculous cholecystitis and its complications] |language=Russian |journal=Khirurgiia (Mosk) |volume= |issue=1 |pages=8–10 |year=1998 |pmid=9511287 |doi= |url=}}</ref><ref name="pmid11432016">{{cite journal |vauthors=Fletcher DR |title=Gallstones. Modern management |journal=Aust Fam Physician |volume=30 |issue=5 |pages=441–5 |year=2001 |pmid=11432016 |doi= |url=}}</ref> | |||
**Cholecystitis (acute/chronic) | |||
**Symptomatic [[cholelithiasis]] | |||
**Biliary [[dyskinesia]] | |||
**Acalculous cholecystitis | |||
**Gallstone [[pancreatitis]] | |||
**Gallbladder mass or polyps | |||
====Contraindications==== | |||
The contraindications of laparoscopic cholecystitis include:<ref name="pmid9511287">{{cite journal |vauthors=Movchun AA, Koloss OE, Oppel' TA, Abdullaeva UA |title=[Surgical treatment of chronic calculous cholecystitis and its complications] |language=Russian |journal=Khirurgiia (Mosk) |volume= |issue=1 |pages=8–10 |year=1998 |pmid=9511287 |doi= |url=}}</ref><ref name="pmid11432016">{{cite journal |vauthors=Fletcher DR |title=Gallstones. Modern management |journal=Aust Fam Physician |volume=30 |issue=5 |pages=441–5 |year=2001 |pmid=11432016 |doi= |url=}}</ref> | |||
*Inability to tolerate [[pneumoperitoneum]] or general [[anesthesia]] | |||
*Uncorrectable [[coagulopathy]] | |||
*Metastatic disease | |||
====Major Complications of cholecystectomy==== | |||
The major complications associated with the cholecystectomy are:<ref name="urlwww.ncbi.nlm.nih.gov">{{cite web |url=http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1358029/pdf/annsurg00170-0061.pdf |title=www.ncbi.nlm.nih.gov |format= |work= |accessdate=2012-08-20}}</ref> | |||
*[[Abscess]] | |||
*[[Ascending cholangitis]] | |||
*Bile duct injury | |||
*[[Bleeding]] (liver surface and cystic artery most common sites) | |||
*[[Hernia]] | |||
*[[Pancreatitis]] | |||
*[[Perforation]] or [[rupture]] | |||
*[[Wound]] [[infection]] | |||
*Organ injury (intestine and liver at highest risk, especially if [[gallbladder]] through inflammation has become scarred or adherent to other organs (e.g. [[transverse colon]])) | |||
*[[Deep vein thrombosis]]/[[pulmonary embolism]] (unusual- risk can be decreased through use of sequential compression devices on legs during surgery) | |||
===Percutaneous cholecystostomy=== | |||
Percutaneous cholecystostomy (PC) is an alternative to emergency [[cholecystectomy]] in complicated cases of high-risk patients.<ref name="pmid24679431">{{cite journal |vauthors=Knab LM, Boller AM, Mahvi DM |title=Cholecystitis |journal=Surg. Clin. North Am. |volume=94 |issue=2 |pages=455–70 |year=2014 |pmid=24679431 |doi=10.1016/j.suc.2014.01.005 |url=}}</ref><ref name="pmid28603584">{{cite journal |vauthors=Gomes CA, Junior CS, Di Saverio S, Sartelli M, Kelly MD, Gomes CC, Gomes FC, Corrêa LD, Alves CB, Guimarães SF |title=Acute calculous cholecystitis: Review of current best practices |journal=World J Gastrointest Surg |volume=9 |issue=5 |pages=118–126 |year=2017 |pmid=28603584 |pmc=5442405 |doi=10.4240/wjgs.v9.i5.118 |url=}}</ref><ref name="pmid26580708">{{cite journal |vauthors=Yeo CS, Tay VW, Low JK, Woon WW, Punamiya SJ, Shelat VG |title=Outcomes of percutaneous cholecystostomy and predictors of eventual cholecystectomy |journal=J Hepatobiliary Pancreat Sci |volume=23 |issue=1 |pages=65–73 |year=2016 |pmid=26580708 |doi=10.1002/jhbp.304 |url=}}</ref> | |||
*The results showed that the mortality, morbidity and conversion rate were the same in PC and [[laparoscopic cholecystectomy]]. | |||
*Older patients with increased comorbidities usually undergo [[cholecystectomy]]. | |||
*If a patient is not a good surgical candidate at the time of presentation, [[cholecystectomy]] is preferred. Patients usually have [[biliary]] complications and [[cholecystectomy]] is required ultimately. | |||
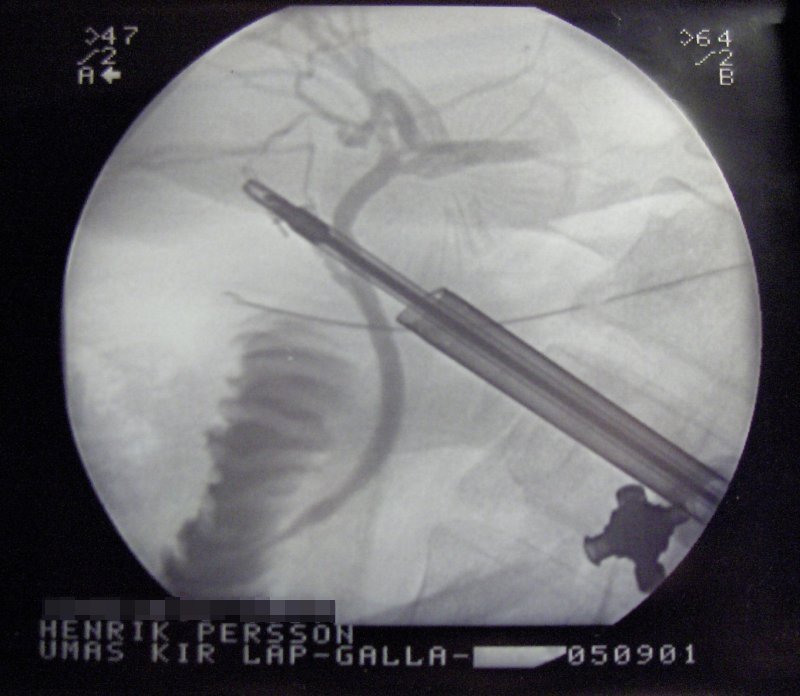
[[Image:Laprascopy-Roentgen.jpg|thumb|center|260px|X-Ray during laparoscopic cholecystectomy]] | |||
==References== | |||
{{reflist|2}} | |||
[[Category:Gastroenterology]] | |||
{{ | [[Category:Hepatology]] | ||
[[Category:Surgery]] | |||
[[Category:Emergency medicine]] | |||
{{WH}} | |||
{{WS}} | |||
Latest revision as of 21:15, 21 February 2018
|
Chronic cholecystitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chronic cholecystitis surgery On the Web |
|
American Roentgen Ray Society Images of Chronic cholecystitis surgery |
|
Risk calculators and risk factors for Chronic cholecystitis surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2]
Overview
Gallbladder removal, cholecystectomy, can be accomplished by the open surgery or a laparoscopic procedure. Laparoscopic cholecystectomy is the operation of choice in uncomplicated calculous cholecystitis. Open cholecystectomy may be performed in complicated cases or when trained/skilled personal for laparoscopic procedure is not available. Supportive measures are instituted in the meantime to prepare the patient for surgery. These measures include fluid resuscitation and antibiotics. Antibiotic regimens usually consist of a broad spectrum cephalosporin such as ceftriaxone and an antibacterial with good cover against anaerobic bacteria, such as metronidazole.
Surgery
Removal of the gallbladder may be done by open surgery or a laparoscopic approach. Laparoscopic cholecystectomy is the procedure of choice in uncomplicated calculous cholecystitis. Open cholecystectomy may be performed in complicated cases or when trained or skilled personal for laparoscopic procedure is not available. Supportive measures such as fluid resuscitation and antibiotics are instituted in the meantime to prepare the patient for surgery. Antibiotic regimens usually consist of a broad spectrum cephalosporin such as ceftriaxone and an antibacterial with good cover against anaerobic bacteria, such as metronidazole.[1][2]
Laparoscopic cholecystectomy
Laparoscopic cholecystectomy is a minimally invasive surgical procedure and has various indications in addition to the chronic cholecystitis. There are two main types of procedures used for the laparoscopic cholecystectomy ; Single-incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC).[3][4][5][6]
- Single-incision laparoscopic cholecystectomy (SILC)
- As compared to CMLC, SILC has the following features:
- Improved cosmetic results
- Decreased postoperative pain
- Increased operative time
- Increased intraoperative blood loss
- As compared to CMLC, SILC has the following features:
- Conventional multiport laparoscopic cholecystectomy (CMLC)
- As compared to SILC, CMLC has the following features:
- Decreased operative time
- Decreased intra-operative blood loss
- As compared to SILC, CMLC has the following features:
Indications
- Indications of laparoscopic cholecystitis are:[1][2]
- Cholecystitis (acute/chronic)
- Symptomatic cholelithiasis
- Biliary dyskinesia
- Acalculous cholecystitis
- Gallstone pancreatitis
- Gallbladder mass or polyps
Contraindications
The contraindications of laparoscopic cholecystitis include:[1][2]
- Inability to tolerate pneumoperitoneum or general anesthesia
- Uncorrectable coagulopathy
- Metastatic disease
Major Complications of cholecystectomy
The major complications associated with the cholecystectomy are:[7]
- Abscess
- Ascending cholangitis
- Bile duct injury
- Bleeding (liver surface and cystic artery most common sites)
- Hernia
- Pancreatitis
- Perforation or rupture
- Wound infection
- Organ injury (intestine and liver at highest risk, especially if gallbladder through inflammation has become scarred or adherent to other organs (e.g. transverse colon))
- Deep vein thrombosis/pulmonary embolism (unusual- risk can be decreased through use of sequential compression devices on legs during surgery)
Percutaneous cholecystostomy
Percutaneous cholecystostomy (PC) is an alternative to emergency cholecystectomy in complicated cases of high-risk patients.[8][9][10]
- The results showed that the mortality, morbidity and conversion rate were the same in PC and laparoscopic cholecystectomy.
- Older patients with increased comorbidities usually undergo cholecystectomy.
- If a patient is not a good surgical candidate at the time of presentation, cholecystectomy is preferred. Patients usually have biliary complications and cholecystectomy is required ultimately.
References
- ↑ 1.0 1.1 1.2 Movchun AA, Koloss OE, Oppel' TA, Abdullaeva UA (1998). "[Surgical treatment of chronic calculous cholecystitis and its complications]". Khirurgiia (Mosk) (in Russian) (1): 8–10. PMID 9511287.
- ↑ 2.0 2.1 2.2 Fletcher DR (2001). "Gallstones. Modern management". Aust Fam Physician. 30 (5): 441–5. PMID 11432016.
- ↑ Sato N, Yabuki K, Shibao K, Mori Y, Tamura T, Higure A, Yamaguchi K (2014). "Risk factors for a prolonged operative time in a single-incision laparoscopic cholecystectomy". HPB (Oxford). 16 (2): 177–82. doi:10.1111/hpb.12100. PMC 3921014. PMID 23557447.
- ↑ Antoniou SA, Pointner R, Granderath FA (2011). "Single-incision laparoscopic cholecystectomy: a systematic review". Surg Endosc. 25 (2): 367–77. doi:10.1007/s00464-010-1217-5. PMID 20607556.
- ↑ Leung D, Yetasook AK, Carbray J, Butt Z, Hoeger Y, Denham W, Barrera E, Ujiki MB (2012). "Single-incision surgery has higher cost with equivalent pain and quality-of-life scores compared with multiple-incision laparoscopic cholecystectomy: a prospective randomized blinded comparison". J. Am. Coll. Surg. 215 (5): 702–8. doi:10.1016/j.jamcollsurg.2012.05.038. PMID 22819642.
- ↑ Pisanu A, Reccia I, Porceddu G, Uccheddu A (2012). "Meta-analysis of prospective randomized studies comparing single-incision laparoscopic cholecystectomy (SILC) and conventional multiport laparoscopic cholecystectomy (CMLC)". J. Gastrointest. Surg. 16 (9): 1790–801. doi:10.1007/s11605-012-1956-9. PMID 22767084.
- ↑ "www.ncbi.nlm.nih.gov" (PDF). Retrieved 2012-08-20.
- ↑ Knab LM, Boller AM, Mahvi DM (2014). "Cholecystitis". Surg. Clin. North Am. 94 (2): 455–70. doi:10.1016/j.suc.2014.01.005. PMID 24679431.
- ↑ Gomes CA, Junior CS, Di Saverio S, Sartelli M, Kelly MD, Gomes CC, Gomes FC, Corrêa LD, Alves CB, Guimarães SF (2017). "Acute calculous cholecystitis: Review of current best practices". World J Gastrointest Surg. 9 (5): 118–126. doi:10.4240/wjgs.v9.i5.118. PMC 5442405. PMID 28603584.
- ↑ Yeo CS, Tay VW, Low JK, Woon WW, Punamiya SJ, Shelat VG (2016). "Outcomes of percutaneous cholecystostomy and predictors of eventual cholecystectomy". J Hepatobiliary Pancreat Sci. 23 (1): 65–73. doi:10.1002/jhbp.304. PMID 26580708.