Cefdinir microbiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
| Line 7: | Line 9: | ||
==Cefdinir microbiology== | ==Cefdinir microbiology== | ||
As with other cephalosporins, bactericidal activity of cefdinir results from inhibition of cell wall synthesis. Cefdinir is stable in the presence of some, but not all, β-lactamase enzymes. As a result, many organisms resistant to | As with other [[[[cephalosporins]]]], bactericidal activity of cefdinir results from inhibition of cell wall synthesis. Cefdinir is stable in the presence of some, but not all, [[Beta-lactamase|[[Beta-lactamase|β-lactamase enzymes]] enzymes]]. As a result, many organisms resistant to [[penicillin]]s and some [[[[cephalosporins]]]] are susceptible to cefdinir. | ||
Cefdinir has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in INDICATIONS AND USAGE. | Cefdinir has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in INDICATIONS AND USAGE. | ||
'''Aerobic Gram-Positive Microorganisms''': | '''[[Aerobic]] Gram-Positive Microorganisms''': | ||
*Staphylococcus aureus (including β-lactamase producing strains) | *[[Staphylococcus aureus]] (including [[Beta-lactamase|β-lactamase enzymes]] producing strains) | ||
NOTE: Cefdinir is inactive against methicillin-resistant staphylococci. | NOTE: Cefdinir is inactive against methicillin-resistant staphylococci. | ||
*Streptococcus pneumoniae (penicillin-susceptible strains only) | *[[Streptococcus pneumoniae]] ([[penicillin]]-susceptible strains only) | ||
*Streptococcus pyogenes | *[[Streptococcus pyogenes]] | ||
'''Aerobic Gram-Negative Microorganisms''': | '''[[Aerobic]] Gram-Negative Microorganisms''': | ||
*Haemophilus influenzae (including β-lactamase producing strains) | *[[Haemophilus influenzae]] (including [[Beta-lactamase|β-lactamase enzymes]] producing strains) | ||
*Haemophilus parainfluenzae (including β-lactamase producing strains) | *[[Haemophilus parainfluenzae]] (including [[Beta-lactamase|β-lactamase enzymes]] producing strains) | ||
*Moraxella catarrhalis (including β-lactamase producing strains) | *[[Moraxella catarrhalis]] (including [[Beta-lactamase|β-lactamase enzymes]] producing strains) | ||
The following in vitro data are available, but their clinical significance is unknown. | The following in vitro data are available, but their clinical significance is unknown. | ||
| Line 33: | Line 35: | ||
Cefdinir exhibits in vitro minimum inhibitory concentrations (MICs) of 1 mcg/mL or less against (≥90%) strains of the following microorganisms; however, the safety and effectiveness of cefdinir in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials. | Cefdinir exhibits in vitro minimum inhibitory concentrations (MICs) of 1 mcg/mL or less against (≥90%) strains of the following microorganisms; however, the safety and effectiveness of cefdinir in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials. | ||
'''Aerobic Gram-Positive Microorganisms''': | '''[[Aerobic]] Gram-Positive Microorganisms''': | ||
*Staphylococcus epidermidis (methicillin-susceptible strains only) | *[[Staphylococcus epidermidis (methicillin-susceptible strains only) | ||
*Streptococcus agalactiae | *[[Streptococcus agalactiae]] | ||
*Viridans group streptococci | *Viridans group [[streptococci]] | ||
NOTE: Cefdinir is inactive against Enterococcus and methicillin-resistant Staphylococcus species. | NOTE: Cefdinir is inactive against Enterococcus and methicillin-resistant Staphylococcus species. | ||
'''Aerobic Gram-Negative Microorganisms''': | '''[[Aerobic]] Gram-Negative Microorganisms''': | ||
*Citrobacter diversus | *[[Citrobacter diversus]] | ||
*Escherichia coli | *[[Escherichia coli]] | ||
*Klebsiella pneumoniae | *[[Klebsiella pneumoniae]] | ||
*Proteus mirabilis | *[[Proteus mirabilis]] | ||
NOTE: Cefdinir is inactive against Pseudomonas and Enterobacter species. | NOTE: Cefdinir is inactive against Pseudomonas and Enterobacter species. | ||
| Line 71: | Line 73: | ||
'''For Streptococcus spp''': | '''For Streptococcus spp''': | ||
Streptococcus pneumoniae that are susceptible to penicillin (MIC ≤0.06 mcg/mL), or streptococci other than S. pneumoniae that are susceptible to penicillin (MIC ≤0.12 mcg/mL), can be considered susceptible to cefdinir. Testing of cefdinir against penicillin-intermediate or penicillin-resistant isolates is not recommended. Reliable interpretive criteria for cefdinir are not available. | Streptococcus pneumoniae that are susceptible to [[penicillin]] (MIC ≤0.06 mcg/mL), or streptococci other than S. pneumoniae that are susceptible to [[penicillin]] (MIC ≤0.12 mcg/mL), can be considered susceptible to cefdinir. Testing of cefdinir against [[[[penicillin]]]]-intermediate or [[[[penicillin]]]]-resistant isolates is not recommended. Reliable interpretive criteria for cefdinir are not available. | ||
A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected. | A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected. | ||
| Line 103: | Line 105: | ||
For Streptococcus spp: | For Streptococcus spp: | ||
Isolates of Streptococcus pneumoniae should be tested against a 1 mcg oxacillin disk. Isolates with oxacillin zone sizes ≥20 mm are susceptible to penicillin and can be considered susceptible to cefdinir. Streptococci other than S. pneumoniae should be tested with a 10 unit penicillin disk. Isolates with penicillin zone sizes ≥28 mm are susceptible to penicillin and can be considered susceptible to cefdinir. | Isolates of [[Streptococcus pneumoniae]] should be tested against a 1 mcg [[oxacillin]] disk. Isolates with oxacillin zone sizes ≥20 mm are susceptible to [[[[penicillin]]]] and can be considered susceptible to cefdinir. Streptococci other than S. pneumoniae should be tested with a 10 unit [[[[penicillin]]]] disk. Isolates with [[penicillin]] zone sizes ≥28 mm are susceptible to [[penicillin]] and can be considered susceptible to cefdinir. | ||
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms to control the technical aspects of laboratory procedures. For the diffusion technique, the 5 mcg cefdinir disk should provide the following zone diameters in these laboratory quality control strains: | As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms to control the technical aspects of laboratory procedures. For the diffusion technique, the 5 mcg cefdinir disk should provide the following zone diameters in these laboratory quality control strains: | ||
| Line 115: | Line 117: | ||
|- | |- | ||
|} | |}<ref>{{Cite web | last = |first = |title = http://www.accessdata.fda.gov/drugsatfda_docs/label/1999/50739S2LBL.pdf |url =http://www.accessdata.fda.gov/drugsatfda_docs/label/1999/50739S2LBL.pdf |publisher = |date = | accessdate = }}</ref> | ||
==References== | |||
{{Reflist}} | |||
{{FDA}} | |||
[[Category:Antibiotics]] | |||
[[Category:Wikinfect]] | |||
Revision as of 20:04, 23 December 2013
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Cefdinir microbiology
As with other [[cephalosporins]], bactericidal activity of cefdinir results from inhibition of cell wall synthesis. Cefdinir is stable in the presence of some, but not all, [[Beta-lactamase|β-lactamase enzymes enzymes]]. As a result, many organisms resistant to penicillins and some [[cephalosporins]] are susceptible to cefdinir.
Cefdinir has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in INDICATIONS AND USAGE.
Aerobic Gram-Positive Microorganisms:
- Staphylococcus aureus (including β-lactamase enzymes producing strains)
NOTE: Cefdinir is inactive against methicillin-resistant staphylococci.
- Streptococcus pneumoniae (penicillin-susceptible strains only)
Aerobic Gram-Negative Microorganisms:
- Haemophilus influenzae (including β-lactamase enzymes producing strains)
- Haemophilus parainfluenzae (including β-lactamase enzymes producing strains)
- Moraxella catarrhalis (including β-lactamase enzymes producing strains)
The following in vitro data are available, but their clinical significance is unknown.
Cefdinir exhibits in vitro minimum inhibitory concentrations (MICs) of 1 mcg/mL or less against (≥90%) strains of the following microorganisms; however, the safety and effectiveness of cefdinir in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic Gram-Positive Microorganisms:
- [[Staphylococcus epidermidis (methicillin-susceptible strains only)
- Viridans group streptococci
NOTE: Cefdinir is inactive against Enterococcus and methicillin-resistant Staphylococcus species.
Aerobic Gram-Negative Microorganisms:
NOTE: Cefdinir is inactive against Pseudomonas and Enterobacter species.
Susceptibility Tests':
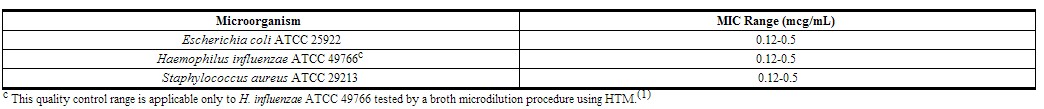
Dilution Techniques: Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MICs). These MICs provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MICs should be determined using a standardized procedure. Standardized procedures are based on a dilution method(1) (broth or agar) or equivalent with standardized inoculum concentrations and standardized concentrations of cefdinir powder. The MIC values should be interpreted according to the following criteria:
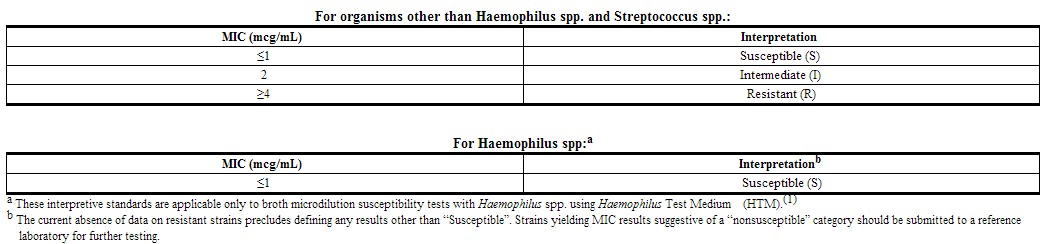 |
For Streptococcus spp:
Streptococcus pneumoniae that are susceptible to penicillin (MIC ≤0.06 mcg/mL), or streptococci other than S. pneumoniae that are susceptible to penicillin (MIC ≤0.12 mcg/mL), can be considered susceptible to cefdinir. Testing of cefdinir against [[penicillin]]-intermediate or [[penicillin]]-resistant isolates is not recommended. Reliable interpretive criteria for cefdinir are not available.
A report of "Susceptible" indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentration usually achievable. A report of "Intermediate" indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of "Resistant" indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Standardized susceptibility test procedures require the use of laboratory control microorganisms to control the technical aspects of laboratory procedures. Standard cefdinir powder should provide the following MIC values:
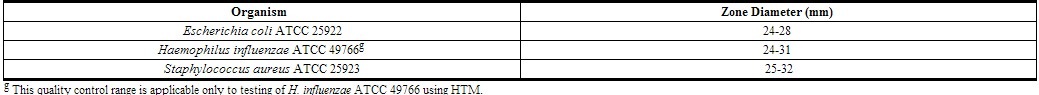
Diffusion Techniques: Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure(2) requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 5 mcg cefdinir to test the susceptibility of microorganisms to cefdinir.
Reports from the laboratory providing results of the standard single-disk susceptibility test with a 5 mcg cefdinir disk should be interpreted according to the following criteria:
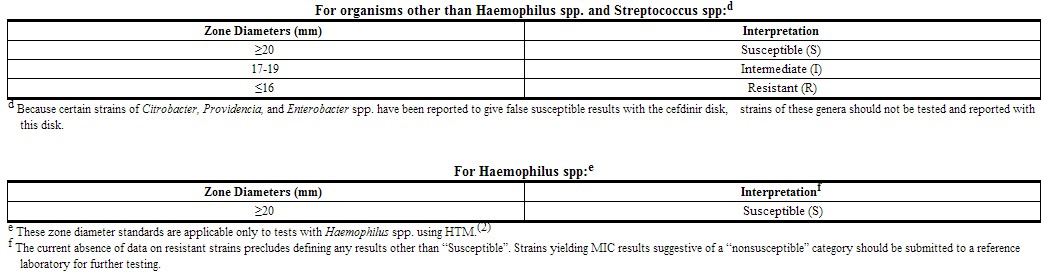 |
For Streptococcus spp:
Isolates of Streptococcus pneumoniae should be tested against a 1 mcg oxacillin disk. Isolates with oxacillin zone sizes ≥20 mm are susceptible to [[penicillin]] and can be considered susceptible to cefdinir. Streptococci other than S. pneumoniae should be tested with a 10 unit [[penicillin]] disk. Isolates with penicillin zone sizes ≥28 mm are susceptible to penicillin and can be considered susceptible to cefdinir.
As with standardized dilution techniques, diffusion methods require the use of laboratory control microorganisms to control the technical aspects of laboratory procedures. For the diffusion technique, the 5 mcg cefdinir disk should provide the following zone diameters in these laboratory quality control strains:
References
- ↑ "http://www.accessdata.fda.gov/drugsatfda_docs/label/1999/50739S2LBL.pdf" (PDF). External link in
|title=(help)
Adapted from the FDA Package Insert.