COVID-19 CT scan: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 16: | Line 16: | ||
**Severity of illness | **Severity of illness | ||
*Bilateral ground glass opacities ± [[consolidation]] in [[posterior]] and peripheral lung regions are considered as the | *Bilateral ground glass opacities ± [[consolidation]] in [[posterior]] and peripheral lung regions are considered as the hallmark for [[COVID-19]]. <ref name="pmid32017661">{{cite journal| author=Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X | display-authors=etal| title=CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). | journal=Radiology | year= 2020 | volume= 295 | issue= 1 | pages= 202-207 | pmid=32017661 | doi=10.1148/radiol.2020200230 | pmc=7194022 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32017661 }} </ref> | ||
*However, there are a large number of typical and atypical [[chest]] [[CT]] findings for [[COVID-19]] that are summarized in the figure below. <ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> <ref name="pmid32489929">{{cite journal| author=Sun Z, Zhang N, Li Y, Xu X| title=A systematic review of chest imaging findings in COVID-19. | journal=Quant Imaging Med Surg | year= 2020 | volume= 10 | issue= 5 | pages= 1058-1079 | pmid=32489929 | doi=10.21037/qims-20-564 | pmc=7242306 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32489929 }} </ref> | *However, there are a large number of typical and atypical [[chest]] [[CT]] findings for [[COVID-19]] that are summarized in the figure below. <ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> <ref name="pmid32489929">{{cite journal| author=Sun Z, Zhang N, Li Y, Xu X| title=A systematic review of chest imaging findings in COVID-19. | journal=Quant Imaging Med Surg | year= 2020 | volume= 10 | issue= 5 | pages= 1058-1079 | pmid=32489929 | doi=10.21037/qims-20-564 | pmc=7242306 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32489929 }} </ref> | ||
[[File:CT-COVID-19.PNG| | [[File:CT-FINDINGS-COVID-19.PNG|700px|center]] | ||
| Line 29: | Line 29: | ||
**Septal thickening | **Septal thickening | ||
**Subpleural and lower lobe involvement more likely | **Subpleural and lower lobe involvement more likely | ||
*[[Chest]] [[Computed tomography|CT scan]] findings | *[[Chest]] [[Computed tomography|CT scan]] findings in [[Patient|patients]] [[Infection|infected]] with [[COVID-19]] are usually: | ||
**Bilateral | **Bilateral peripheral [[lung]] [[opacities]]<ref name="LeiLi2020">{{cite journal|last1=Lei|first1=Junqiang|last2=Li|first2=Junfeng|last3=Li|first3=Xun|last4=Qi|first4=Xiaolong|title=CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia|journal=Radiology|year=2020|pages=200236|issn=0033-8419|doi=10.1148/radiol.2020200236}}</ref> | ||
** | **without subpleural sparing | ||
*[[Right]] and [[left]] lower [[lung]] [[lobes]] were the most common involved [[lobes]] (65% and 63%) in [[COVID-19]]. <ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref> | *[[Right]] and [[left]] lower [[lung]] [[lobes]] were the most common involved [[lobes]] (65% and 63%) in [[COVID-19]]. <ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref> | ||
*Time interval between onset of [[symptoms]] and [[chest]] [[CT]] manifestations is classified into 3 stages<ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref>: | *Time interval between onset of [[symptoms]] and [[chest]] [[CT]] manifestations is classified into 3 stages<ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref>: | ||
** | ** Early: between 0-2 days | ||
** | **Intermediate: between 3-5 days | ||
** | **Late: between 6-12 days | ||
*[[Ground-glass opacities]] and [[consolidation]] are more likely to develop in the | *[[Ground-glass opacities]] and [[consolidation]] are more likely to develop in the intermediate and late stages. <ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref> | ||
*[[Linear]] [[opacities]], [[crazy-paving pattern]], and [[reverse halo]] sign usually develop during the | *[[Linear]] [[opacities]], [[crazy-paving pattern]], and [[reverse halo]] sign usually develop during the late stages. <ref name="pmid32077789">{{cite journal| author=Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N | display-authors=etal| title=Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection. | journal=Radiology | year= 2020 | volume= 295 | issue= 3 | pages= 200463 | pmid=32077789 | doi=10.1148/radiol.2020200463 | pmc=7233369 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32077789 }} </ref> | ||
*The presence of [[consolidation]] is a sign of | *The presence of [[consolidation]] is a sign of disease progression. <ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> | ||
*The presence of [[pleural effusion]] in [[COVID-19]] is associated with poor [[prognosis]].<ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> | *The presence of [[pleural effusion]] in [[COVID-19]] is associated with poor [[prognosis]].<ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> | ||
*The presence of [[lymphadenopathy]] and [[pericardial effusion]] are associated with severe [[COVID-19]] [[pneumonia]]. <ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> | *The presence of [[lymphadenopathy]] and [[pericardial effusion]] are associated with severe [[COVID-19]] [[pneumonia]]. <ref name="pmid32193638">{{cite journal| author=Ye Z, Zhang Y, Wang Y, Huang Z, Song B| title=Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. | journal=Eur Radiol | year= 2020 | volume= | issue= | pages= | pmid=32193638 | doi=10.1007/s00330-020-06801-0 | pmc=7088323 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32193638 }} </ref> | ||
Revision as of 19:12, 19 July 2020
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19 CT scan On the Web |
|
American Roentgen Ray Society Images of COVID-19 CT scan |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sabawoon Mirwais, M.B.B.S, M.D.[2] Syed Hassan A. Kazmi BSc, MD [3] Aditya Ganti M.B.B.S. [4] Nasrin Nikravangolsefid, MD-MPH [5]
Overview
Non-contrast Chest CT scan is an effective method for the rapid diagnosis of COVID-19 and monitoring the disease progression. Chest CT scan findings in patients infected with coronavirus can include unilateral or bilateral pneumonia, mottling and ground glass opacity, focal or multifocal opacities, consolidation, and septal thickening with subpleural and lower lobe involvement more likely.
CT scan
- Non-contrast Chest CT scan is an effective method not only for the rapid diagnosis of COVID-19 but also for monitoring the disease progression. [1]
- Given the high sensitivity of chest CT, it can be used in suspected patients with negative RT-PCR. [2]
- Various chest CT features have been found diagnostic for COVID-19 that are associated with:
- Duration of illness
- Severity of illness
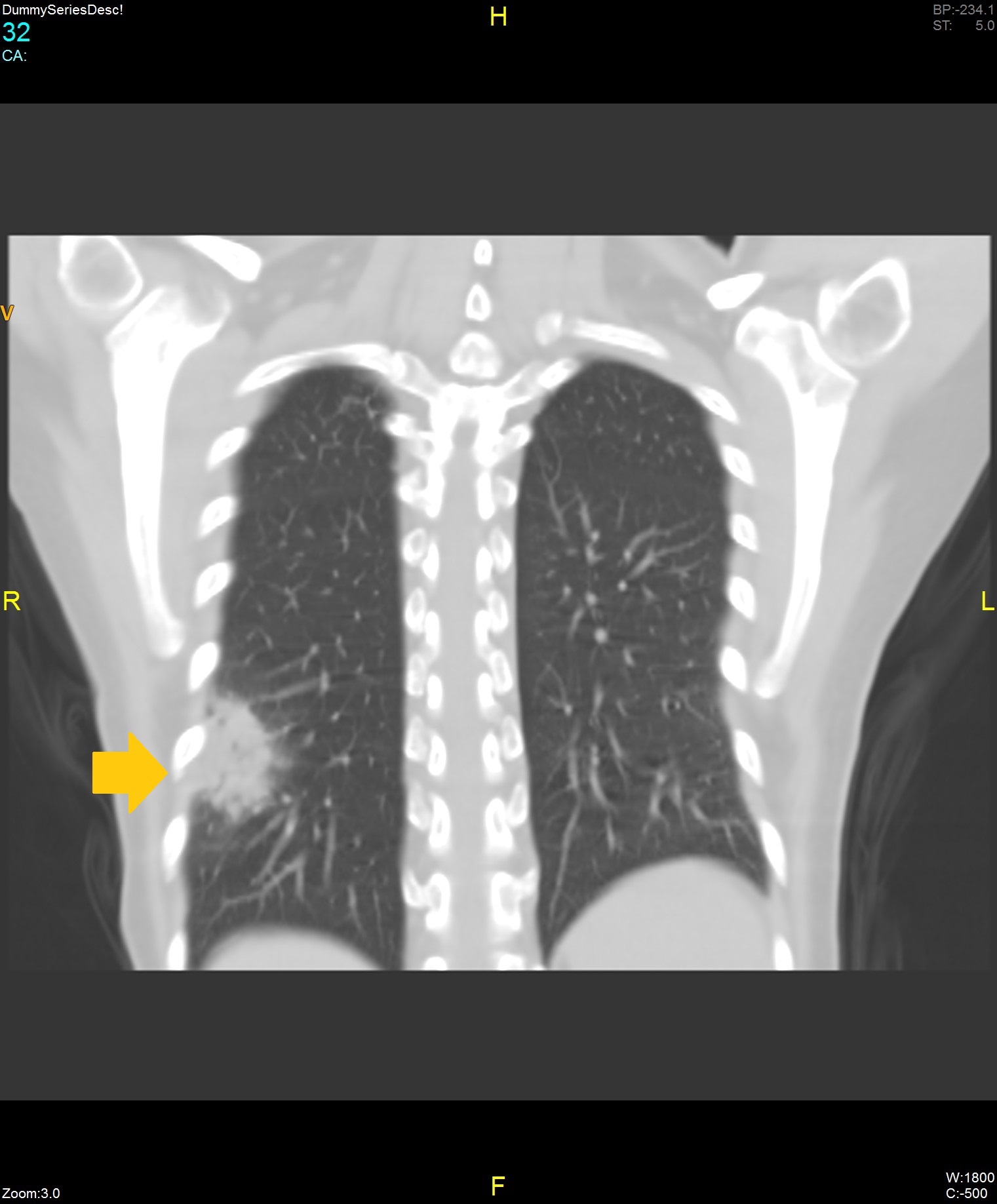
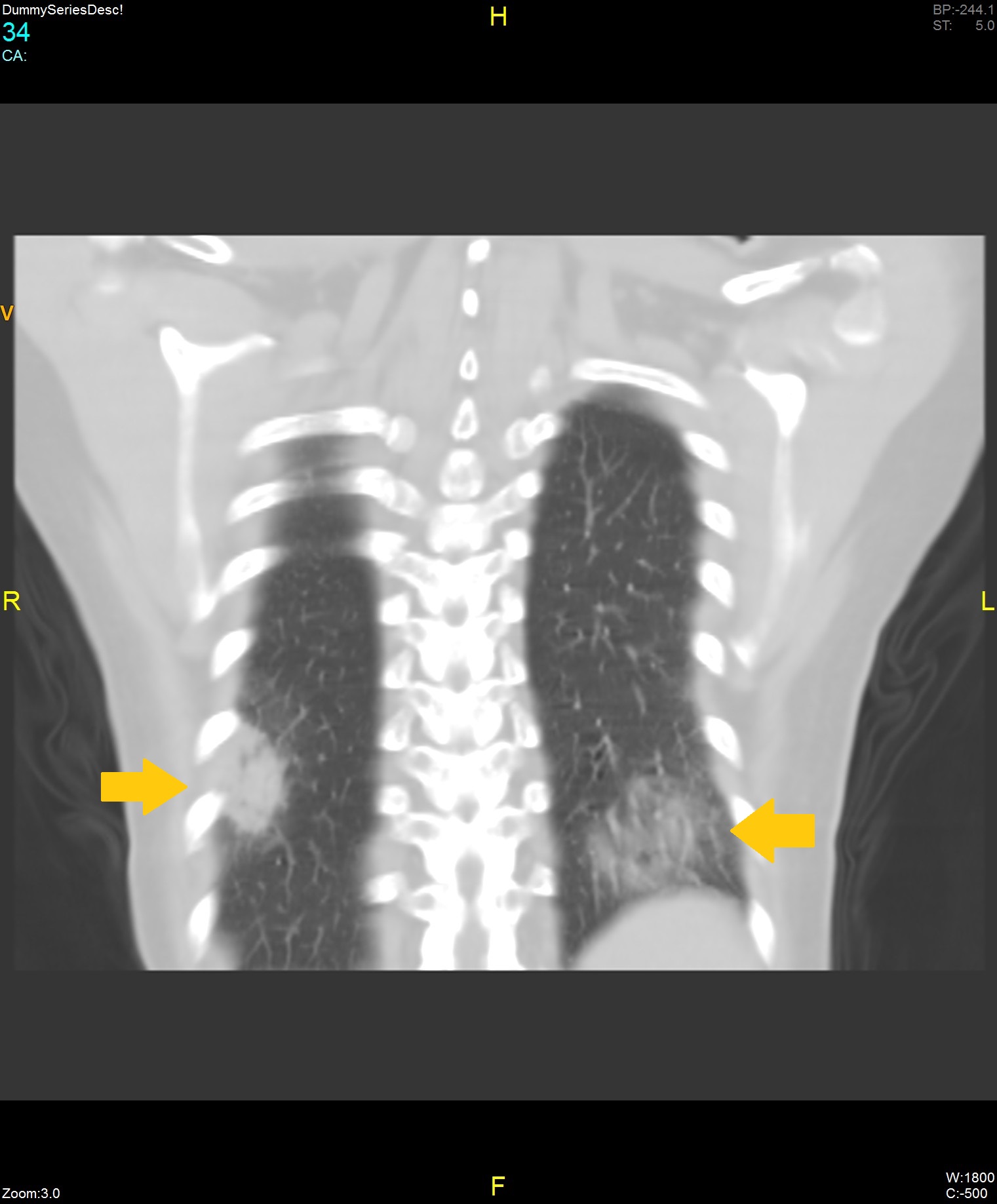
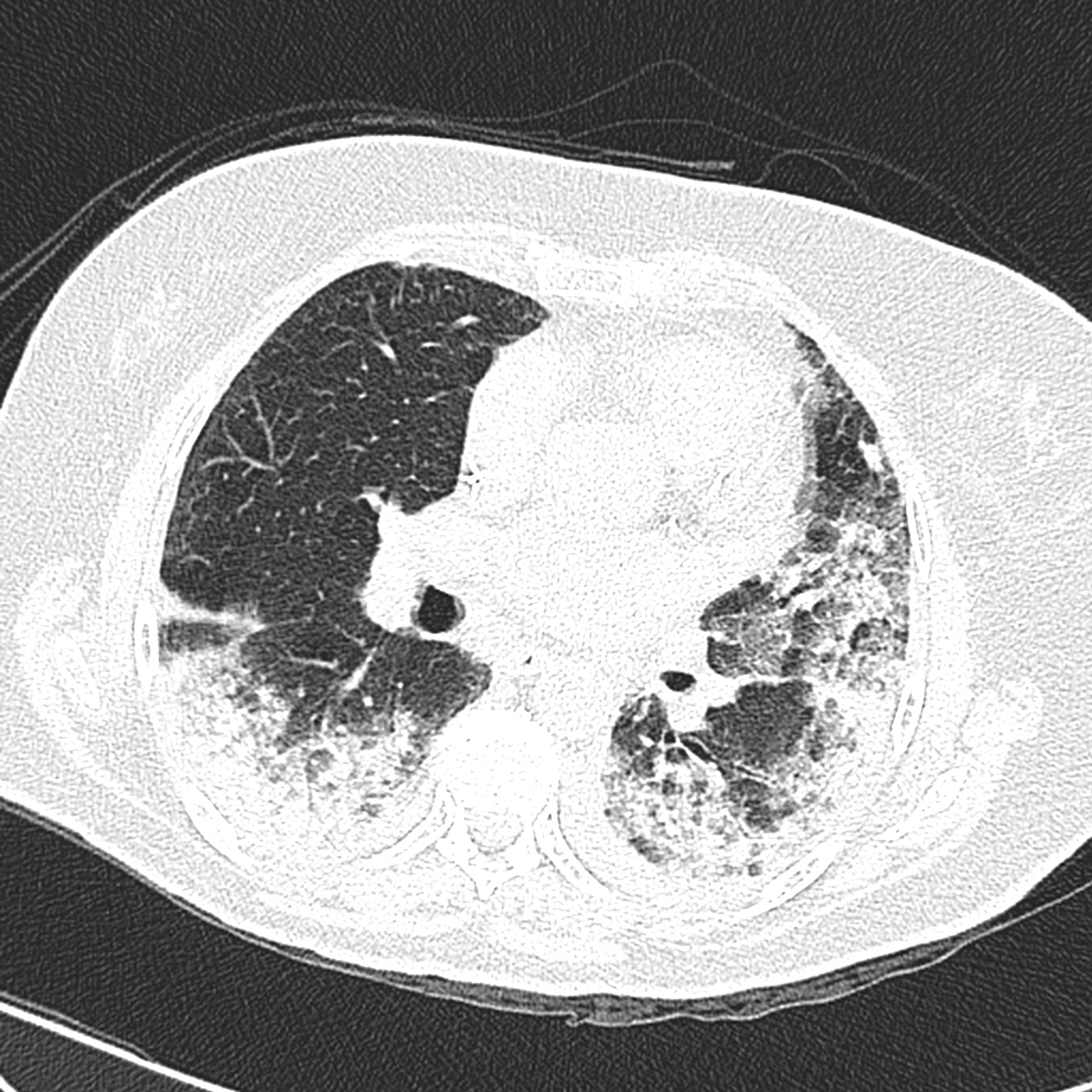
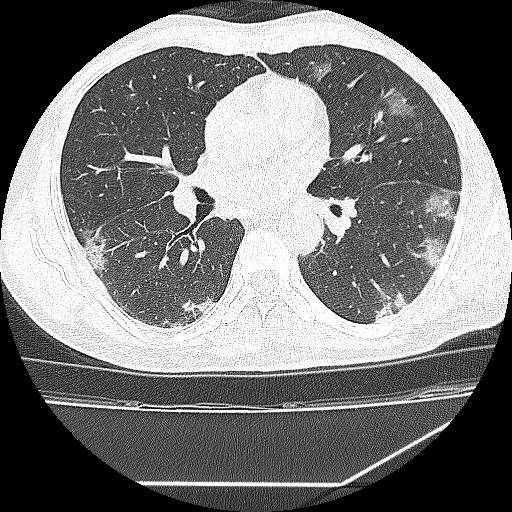
- Bilateral ground glass opacities ± consolidation in posterior and peripheral lung regions are considered as the hallmark for COVID-19. [3]
- However, there are a large number of typical and atypical chest CT findings for COVID-19 that are summarized in the figure below. [4] [5]

- Chest CT scan findings in patients infected with coronavirus can include:
- Unilateral or bilateral pneumonia[6][7][8]
- Mottling and ground-glass opacity
- Focal or multifocal opacities
- Consolidation
- Septal thickening
- Subpleural and lower lobe involvement more likely
- Chest CT scan findings in patients infected with COVID-19 are usually:
- Time interval between onset of symptoms and chest CT manifestations is classified into 3 stages[10]:
- Early: between 0-2 days
- Intermediate: between 3-5 days
- Late: between 6-12 days
- Ground-glass opacities and consolidation are more likely to develop in the intermediate and late stages. [10]
- Linear opacities, crazy-paving pattern, and reverse halo sign usually develop during the late stages. [10]
- The presence of consolidation is a sign of disease progression. [4]
- The presence of pleural effusion in COVID-19 is associated with poor prognosis.[4]
- The presence of lymphadenopathy and pericardial effusion are associated with severe COVID-19 pneumonia. [4]
- chest CT manifestations are usually resolved within 14 days of symptoms onset. [11]
Radiological Society of North America
The Radiological Society of North America (RSNA) classified CT findings of COVID-19 infection into four categories which were endorsed by the Society of Thoracic Radiology and the American College of Radiology (ACR):
| RSNA CT findings classification of Covid-19[12] | |
|---|---|
| Typical appearance |
|
| Indeterminate appearance | Absence of typical CT findings and the presence of
|
| Atypical appearance | Absence of typical or indeterminate features and the presence of
|
| Negative for pneumonia | No CT features to suggest pneumonia, in particular, absent GGO and consolidation |
Images
References
- ↑ Xu B, Xing Y, Peng J, Zheng Z, Tang W, Sun Y; et al. (2020). "Chest CT for detecting COVID-19: a systematic review and meta-analysis of diagnostic accuracy". Eur Radiol. doi:10.1007/s00330-020-06934-2. PMC 7227176 Check
|pmc=value (help). PMID 32415585 Check|pmid=value (help). - ↑ Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P; et al. (2020). "Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR". Radiology: 200432. doi:10.1148/radiol.2020200432. PMC 7233365 Check
|pmc=value (help). PMID 32073353 Check|pmid=value (help). - ↑ Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X; et al. (2020). "CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)". Radiology. 295 (1): 202–207. doi:10.1148/radiol.2020200230. PMC 7194022 Check
|pmc=value (help). PMID 32017661 Check|pmid=value (help). - ↑ 4.0 4.1 4.2 4.3 Ye Z, Zhang Y, Wang Y, Huang Z, Song B (2020). "Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review". Eur Radiol. doi:10.1007/s00330-020-06801-0. PMC 7088323 Check
|pmc=value (help). PMID 32193638 Check|pmid=value (help). - ↑ Sun Z, Zhang N, Li Y, Xu X (2020). "A systematic review of chest imaging findings in COVID-19". Quant Imaging Med Surg. 10 (5): 1058–1079. doi:10.21037/qims-20-564. PMC 7242306 Check
|pmc=value (help). PMID 32489929 Check|pmid=value (help). - ↑ Paul NS, Roberts H, Butany J, Chung T, Gold W, Mehta S, Konen E, Rao A, Provost Y, Hong HH, Zelovitsky L, Weisbrod GL (2004). "Radiologic pattern of disease in patients with severe acute respiratory syndrome: the Toronto experience". Radiographics. 24 (2): 553–63. doi:10.1148/rg.242035193. PMID 15026600.
- ↑ Ajlan AM, Ahyad RA, Jamjoom LG, Alharthy A, Madani TA (October 2014). "Middle East respiratory syndrome coronavirus (MERS-CoV) infection: chest CT findings". AJR Am J Roentgenol. 203 (4): 782–7. doi:10.2214/AJR.14.13021. PMID 24918624.
- ↑ Chen, Nanshan; Zhou, Min; Dong, Xuan; Qu, Jieming; Gong, Fengyun; Han, Yang; Qiu, Yang; Wang, Jingli; Liu, Ying; Wei, Yuan; Xia, Jia'an; Yu, Ting; Zhang, Xinxin; Zhang, Li (2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". The Lancet. doi:10.1016/S0140-6736(20)30211-7. ISSN 0140-6736.
- ↑ Lei, Junqiang; Li, Junfeng; Li, Xun; Qi, Xiaolong (2020). "CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia". Radiology: 200236. doi:10.1148/radiol.2020200236. ISSN 0033-8419.
- ↑ 10.0 10.1 10.2 10.3 Bernheim A, Mei X, Huang M, Yang Y, Fayad ZA, Zhang N; et al. (2020). "Chest CT Findings in Coronavirus Disease-19 (COVID-19): Relationship to Duration of Infection". Radiology. 295 (3): 200463. doi:10.1148/radiol.2020200463. PMC 7233369 Check
|pmc=value (help). PMID 32077789 Check|pmid=value (help). - ↑ Pan, Feng; Ye, Tianhe; Sun, Peng; Gui, Shan; Liang, Bo; Li, Lingli; Zheng, Dandan; Wang, Jiazheng; Hesketh, Richard L.; Yang, Lian; Zheng, Chuansheng (2020). "Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19)". Radiology. 295 (3): 715–721. doi:10.1148/radiol.2020200370. ISSN 0033-8419.
- ↑ Simpson, Scott; Kay, Fernando U.; Abbara, Suhny; Bhalla, Sanjeev; Chung, Jonathan H.; Chung, Michael; Henry, Travis S.; Kanne, Jeffrey P.; Kligerman, Seth; Ko, Jane P.; Litt, Harold (2020). "Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA". Radiology: Cardiothoracic Imaging. 2 (2): e200152. doi:10.1148/ryct.2020200152. ISSN 2638-6135.
- ↑ Case courtesy of Medico Assistente Dr. Chong Keng Sang, Sam, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/73890">rID: 73890</a>
- ↑ Case courtesy of Medico Assistente Dr. Chong Keng Sang, Sam, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/73890">rID: 73890</a>
- ↑ Case courtesy of Dr Antonio Rodrigues de Aguiar Neto, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/76921">rID: 76921</a>
- ↑ Case courtesy of Dr Bahman Rasuli, <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/75768">rID: 75768</a>