COVID-19-associated encephalitis: Difference between revisions
| Line 60: | Line 60: | ||
[[COVID-19]]-associated [[encephalitis]] must be differentiated from other [[diseases]] that cause [[fever]], [[headache]], and [[altered mental status]] with or without [[cough]], such as | [[COVID-19]]-associated [[encephalitis]] must be differentiated from other [[diseases]] that cause [[fever]], [[headache]], and [[altered mental status]] with or without [[cough]], such as | ||
* [[Meningitis]] | * [[Meningitis]]<ref name="pmid32251791" /> | ||
* Acute [[hypoglycemia]] | * Acute [[hypoglycemia]] | ||
* [[Brain abscess]] | * [[Brain abscess]] | ||
| Line 70: | Line 70: | ||
* [[Tuberculosis]] | * [[Tuberculosis]] | ||
* [[Sepsis]] | * [[Sepsis]] | ||
*[[Glial tumor]]<ref name="pmid32479911">{{cite journal| author=Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K| title=COVID-19-Associated Encephalitis Mimicking Glial Tumor. | journal=World Neurosurg | year= 2020 | volume= 140 | issue= | pages= 46-48 | pmid=32479911 | doi=10.1016/j.wneu.2020.05.194 | pmc=7256557 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32479911 }}</ref> | |||
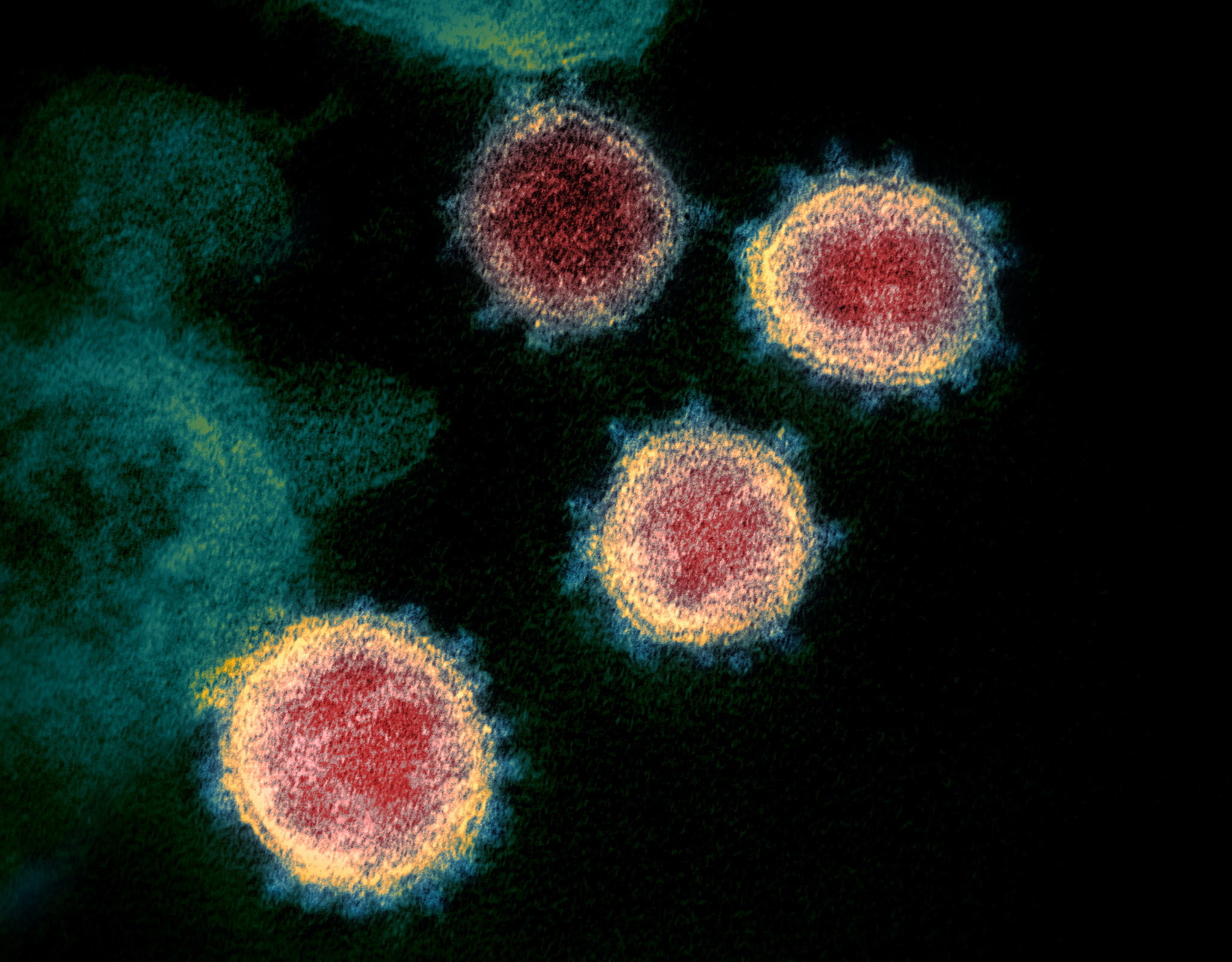
[[File:SARS-CoV-2 49534865371.jpg|thumb|Case courtesy of Dr. Daniel J Bell, Radiopaedia.org, rID: 74536]] | |||
==Risk Factors== | |||
Common risk factors in the development of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] may be occupational, environmental, and [[genetic]]. | |||
* [[Risk factors]] for this [[disease]] are the same as for [[COVID-19]]. | * [[Risk factors]] for this [[disease]] are the same as for [[COVID-19]]. | ||
* Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapies.<ref name="pmid32229625">{{cite journal| author=Nath A| title=Neurologic complications of coronavirus infections. | journal=Neurology | year= 2020 | volume= 94 | issue= 19 | pages= 809-810 | pmid=32229625 | doi=10.1212/WNL.0000000000009455 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32229625 }}</ref> | * Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapies.<ref name="pmid32229625">{{cite journal| author=Nath A| title=Neurologic complications of coronavirus infections. | journal=Neurology | year= 2020 | volume= 94 | issue= 19 | pages= 809-810 | pmid=32229625 | doi=10.1212/WNL.0000000000009455 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32229625 }}</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Risk factors for COVID-19-associated encephalitis | |+Risk factors for COVID-19-associated encephalitis | ||
!Autoimmune disease | !Autoimmune disease | ||
!Immunosuppression | !Immunosuppression | ||
|- | |- | ||
|Multiple sclerosis | |Multiple sclerosis | ||
| Line 161: | Line 109: | ||
* There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis. | * There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis. | ||
== | ==Complications== | ||
* If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause: | * If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause: | ||
| Line 169: | Line 117: | ||
{{familytree | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | }} | {{familytree | |,|-|-|-|v|-|-|-|+|-|-|-|v|-|-|-|.| | }} | ||
{{familytree | |!| | | |!| | | |!| | | |!| | | |!| | | }} | {{familytree | |!| | | |!| | | |!| | | |!| | | |!| | | }} | ||
{{familytree | D01 | | D02 | | D03 | | D04 | | D05 |D01=Memory loss|D02=Epilepsy|D03=Personality changes|D04=Hearing/vision | {{familytree | D01 | | D02 | | D03 | | D04 | | D05 |D01=Memory loss|D02=Epilepsy|D03=Personality changes|D04=Hearing/vision loss|D05=Coma/Death}} | ||
{{familytree/end}} | {{familytree/end}}<br /> | ||
==Diagnosis== | ==Diagnosis== | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
* The majority of patients with COVID-19-associated encephalitis present with respiratory symptoms. ''e.g.'' cough, shortness of breath ''etc''. | |||
* '''Two''' '''cases''' reported till now has specific clinical manifestations: | |||
===Physical Examination=== | ===Physical Examination=== | ||
Revision as of 16:12, 29 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2]
Synonyms and keywords:
Overview
Encephalitis is inflammation of the brain parenchyma and it is commonly caused by viruses. COVID-19 is a virus related to the severe acute respiratory syndrome coronavirus (SARS-CoV) group and named as SARS-CoV-2.
Historical Perspective
- Covid-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2.[1][2]
- The association between COVID-19 and encephalitis was made during this pandemic started in December in Wuhan, China and named as Wuhan coronavirus.[3]
- In March 2020, Dr. Ali A. was the first to discover the association between COVID-19 and neurological diseases e.g. encephalitis. He made a clinical diagnosis along with his team and then MRI used to diagnose the disease.[4]
- In January 2020, Chinese doctors confirmed the first case of encephalitis due to COVID-19 in a 56 year old male and they conducted gene sequencing on cerebrospinal fluid (CSF) samples and confirmed the novel virus inside brain, but it was not published.
- There have been several outbreaks of SARS and MERS.
Classification
- There is no established system for the classification of COVID-19 associated encephalitis.
- Based on the duration of symptoms, this disease is classified as acute.
Pathophysiology
- The exact pathogenesis of COVID-19 encephalitis is not fully understood.
- It is thought that this viral encephalitis is the result of multiple pathologies.
| SARS-CoV-2 Entry via Nose | |||||||||||||||||||||||||||||||||||||||||
| Olfactory Epithelium | |||||||||||||||||||||||||||||||||||||||||
| Olfactory Bulb | |||||||||||||||||||||||||||||||||||||||||
| ACE2 | Direct Injury due to Infection | Immune Injury | Hypoxic Injury | Hypercoagulability | |||||||||||||||||||||||||||||||||||||
| Viral Encephalitis | |||||||||||||||||||||||||||||||||||||||||
- ACE2: Angiotensin converting enzyme receptor 2 is present in multiple organs e.g. lungs, brain, and kidney, etc.
- Hypercoagulability: With elevated D-dimer
- Immune injury: Cytokine activation and vascular involvement.
- Direct injury: Due to hematogenous and neuronal pathway involvement.
- Hypoxic injury: Due to anaerobic metabolism.[5]
Causes
- Coronavirus disease 2019 (COVID-19) associated encephalitis is caused by SARS-CoV-2.
- To read more about this virus, click here.
Differentiating COVID-19-associated encephalitis from other Diseases
COVID-19-associated encephalitis must be differentiated from other diseases that cause fever, headache, and altered mental status with or without cough, such as
- Meningitis[2]
- Acute hypoglycemia
- Brain abscess
- Herpes simplex encephalitis
- Leptospirosis in humans
- Status epilepticus
- Systemic lupus erythematosus (SLE)
- Cat scratch disease
- Tuberculosis
- Sepsis
- Glial tumor[6]
Risk Factors
Common risk factors in the development of COVID-19-associated encephalitis may be occupational, environmental, and genetic.
- Risk factors for this disease are the same as for COVID-19.
- Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapies.[7]
| Autoimmune disease | Immunosuppression |
|---|---|
| Multiple sclerosis | Interferon beta
Glatiramer Corticosteroids |
| Myasthenia gravis | Corticosteroids |
| Neuromyeilits optica | Monoclonal antibody |
| Sarcoidosis | Corticosteroids
Methotrexate Azathioprine |
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis.
Complications
- If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause:
| Encephalitis | |||||||||||||||||||||||||||||||||||||||||
| Memory loss | Epilepsy | Personality changes | Hearing/vision loss | Coma/Death | |||||||||||||||||||||||||||||||||||||
Diagnosis
History and Symptoms
- The majority of patients with COVID-19-associated encephalitis present with respiratory symptoms. e.g. cough, shortness of breath etc.
- Two cases reported till now has specific clinical manifestations:
Physical Examination
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Laboratory Findings
An elevated/reduced concentration of serum/blood/urinary/CSF/other [lab test] is diagnostic of [disease name].
OR
Laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
OR
[Test] is usually normal among patients with [disease name].
OR
Some patients with [disease name] may have elevated/reduced concentration of [test], which is usually suggestive of [progression/complication].
OR
There are no diagnostic laboratory findings associated with [disease name].
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
There are no CT scan findings associated with [disease name].
OR
[Location] CT scan may be helpful in the diagnosis of [disease name]. Findings on CT scan suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no CT scan findings associated with [disease name]. However, a CT scan may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
MRI
There are no MRI findings associated with [disease name].
OR
[Location] MRI may be helpful in the diagnosis of [disease name]. Findings on MRI suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no MRI findings associated with [disease name]. However, a MRI may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Other Imaging Findings
There are no other imaging findings associated with [disease name].
OR
[Imaging modality] may be helpful in the diagnosis of [disease name]. Findings on an [imaging modality] suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
There is no treatment for [disease name]; the mainstay of therapy is supportive care.
OR
Supportive therapy for [disease name] includes [therapy 1], [therapy 2], and [therapy 3].
OR
The majority of cases of [disease name] are self-limited and require only supportive care.
OR
[Disease name] is a medical emergency and requires prompt treatment.
OR
The mainstay of treatment for [disease name] is [therapy].
OR
The optimal therapy for [malignancy name] depends on the stage at diagnosis.
OR
[Therapy] is recommended among all patients who develop [disease name].
OR
Pharmacologic medical therapy is recommended among patients with [disease subclass 1], [disease subclass 2], and [disease subclass 3].
OR
Pharmacologic medical therapies for [disease name] include (either) [therapy 1], [therapy 2], and/or [therapy 3].
OR
Empiric therapy for [disease name] depends on [disease factor 1] and [disease factor 2].
OR
Patients with [disease subclass 1] are treated with [therapy 1], whereas patients with [disease subclass 2] are treated with [therapy 2].
Surgery
Surgical intervention is not recommended for the management of [disease name].
OR
Surgery is not the first-line treatment option for patients with [disease name]. Surgery is usually reserved for patients with either [indication 1], [indication 2], and [indication 3]
OR
The mainstay of treatment for [disease name] is medical therapy. Surgery is usually reserved for patients with either [indication 1], [indication 2], and/or [indication 3].
OR
The feasibility of surgery depends on the stage of [malignancy] at diagnosis.
OR
Surgery is the mainstay of treatment for [disease or malignancy].
Primary Prevention
There are no established measures for the primary prevention of [disease name].
OR
There are no available vaccines against [disease name].
OR
Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
OR
[Vaccine name] vaccine is recommended for [patient population] to prevent [disease name]. Other primary prevention strategies include [strategy 1], [strategy 2], and [strategy 3].
Secondary Prevention
There are no established measures for the secondary prevention of [disease name].
OR
Effective measures for the secondary prevention of [disease name] include [strategy 1], [strategy 2], and [strategy 3].
References
- ↑ Velavan TP, Meyer CG (2020). "The COVID-19 epidemic". Trop Med Int Health. 25 (3): 278–280. doi:10.1111/tmi.13383. PMC 7169770 Check
|pmc=value (help). PMID 32052514 Check|pmid=value (help). - ↑ 2.0 2.1 Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Riou J, Althaus CL (2020). "Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020". Euro Surveill. 25 (4). doi:10.2807/1560-7917.ES.2020.25.4.2000058. PMC 7001239 Check
|pmc=value (help). PMID 32019669 Check|pmid=value (help). - ↑ Asadi-Pooya AA, Simani L (2020). "Central nervous system manifestations of COVID-19: A systematic review". J Neurol Sci. 413: 116832. doi:10.1016/j.jns.2020.116832. PMC 7151535 Check
|pmc=value (help). PMID 32299017 Check|pmid=value (help). - ↑ Baig AM (2020). "Neurological manifestations in COVID-19 caused by SARS-CoV-2". CNS Neurosci Ther. 26 (5): 499–501. doi:10.1111/cns.13372. PMC 7163592 Check
|pmc=value (help). PMID 32266761 Check|pmid=value (help). - ↑ Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K (2020). "COVID-19-Associated Encephalitis Mimicking Glial Tumor". World Neurosurg. 140: 46–48. doi:10.1016/j.wneu.2020.05.194. PMC 7256557 Check
|pmc=value (help). PMID 32479911 Check|pmid=value (help). - ↑ Nath A (2020). "Neurologic complications of coronavirus infections". Neurology. 94 (19): 809–810. doi:10.1212/WNL.0000000000009455. PMID 32229625 Check
|pmid=value (help).