Bupropion: Difference between revisions
No edit summary |
No edit summary |
||
| Line 408: | Line 408: | ||
* WELLBUTRIN Tablets, 100 mg of bupropion hydrochloride, are red, round, biconvex tablets printed with “WELLBUTRIN 100” in bottles of 100 (NDC 0173-0178-55). | * WELLBUTRIN Tablets, 100 mg of bupropion hydrochloride, are red, round, biconvex tablets printed with “WELLBUTRIN 100” in bottles of 100 (NDC 0173-0178-55). | ||
|storage=* Store at room temperature, 20° to 25°C (68° to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [See USP Controlled Room Temperature]. Protect from light and moisture. | |storage=* Store at room temperature, 20° to 25°C (68° to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [See USP Controlled Room Temperature]. Protect from light and moisture. | ||
|fdaPatientInfo=For patient information, please click [[here]]. | |fdaPatientInfo=For patient information, please click [[here]]. | ||
* Advise the patient to read the FDA-approved patient labeling (Medication Guide) | * Advise the patient to read the FDA-approved patient labeling (Medication Guide) | ||
| Line 432: | Line 428: | ||
:* Instruct patients to discontinue and not restart WELLBUTRIN if they experience a seizure while on treatment. Advise patients that the excessive use or abrupt discontinuation of [[alcohol]], [[benzodiazepines]], [[antiepileptic drugs]], or [[sedatives]]/[[hypnotics]] can increase the risk of [[seizure]]. Advise patients to minimize or avoid use of [[alcohol]]. | :* Instruct patients to discontinue and not restart WELLBUTRIN if they experience a seizure while on treatment. Advise patients that the excessive use or abrupt discontinuation of [[alcohol]], [[benzodiazepines]], [[antiepileptic drugs]], or [[sedatives]]/[[hypnotics]] can increase the risk of [[seizure]]. Advise patients to minimize or avoid use of [[alcohol]]. | ||
* Bupropion-Containing Products | |||
:* Educate patients that WELLBUTRIN contains the same active ingredient (bupropion hydrochloride) found in ZYBAN, which is used as an aid to smoking cessation treatment, and that WELLBUTRIN should not be used in combination with ZYBAN or any other medications that contain bupropion (such as WELLBUTRIN SR®, the sustained-release formulation and WELLBUTRIN XL® or FORFIVO XL™, the extended-release formulations, and APLENZIN®, the extended-release formulation of bupropion hydrobromide). In addition, there are a number of generic bupropion HCl products for the immediate-, sustained-, and extended-release formulations. | :* Educate patients that WELLBUTRIN contains the same active ingredient (bupropion hydrochloride) found in ZYBAN, which is used as an aid to smoking cessation treatment, and that WELLBUTRIN should not be used in combination with ZYBAN or any other medications that contain bupropion (such as WELLBUTRIN SR®, the sustained-release formulation and WELLBUTRIN XL® or FORFIVO XL™, the extended-release formulations, and APLENZIN®, the extended-release formulation of bupropion hydrobromide). In addition, there are a number of generic bupropion HCl products for the immediate-, sustained-, and extended-release formulations. | ||
Revision as of 14:39, 20 May 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Chetan Lokhande, M.B.B.S [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Suicidal thoughts and behaviours; and neuropsychiatry reactions
See full prescribing information for complete Boxed Warning.
*Increased risk of suicidal thinking and behavior in children, adolescents, and young adults taking antidepressants.
|
Overview
Bupropion is a tetracyclics and unicyclics that is FDA approved for the {{{indicationType}}} of major depressive disorder (MDD)depression, associated with seasonal affective disorder; prophylaxis. There is a Black Box Warning for this drug as shown here. Common adverse reactions include suicidal thoughts and behaviors in adolescents and young adults, neuropsychiatric symptoms and suicide risk in smoking cessation treatment, seizure, hypertension, activation of mania or hypomania, psychosis and other neuropsychiatric reactions, hypersensitivity reactions.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Major depressive disorder (MDD)
- To minimize the risk of seizure, increase the dose gradually [see Warnings and Precautions]. Increases in dose should not exceed 100 mg per day in a 3‑day period. Bupropion Tablets should be swallowed whole and not crushed, divided, or chewed. Bupropion may be taken with or without food.
- The recommended starting dose is 200 mg per day, given as 100 mg twice daily. After 3 days of dosing, the dose may be increased to 300 mg per day, given as 100 mg 3 times daily, with at least 6 hours between successive doses. Dosing above 300 mg per day may be accomplished using the 75- or 100-mg tablets.
- A maximum of 450 mg per day, given in divided doses of not more than 150 mg each, may be considered for patients who show no clinical improvement after several weeks of treatment at 300 mg per day. Administer the 100‑mg tablet 4 times daily to not exceed the limit of 150 mg in a single dose.
- It is generally agreed that acute episodes of depression require several months or longer of antidepressant drug treatment beyond the response in the acute episode. It is unknown whether the dose of Bupropion needed for maintenance treatment is identical to the dose that provided an initial response. Periodically reassess the need for maintenance treatment and the appropriate dose for such treatment.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Condition 1
- Developed by: (Organization)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- There is limited information about Off-Label Non–Guideline-Supported Use of Bupropion in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organization)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Condition 1
- Dosing Information
- There is limited information about Off-Label Non–Guideline-Supported Use of Bupropion in pediatric patients.
Contraindications
- Seizure disorder
- Bulimia or anorexia nervosa
- Patients undergoing abrupt discontinuation of alcohol, benzodiazepines, barbiturates, and antiepileptic drugs
Warnings
|
Suicidal thoughts and behaviours; and neuropsychiatry reactions
See full prescribing information for complete Boxed Warning.
*Increased risk of suicidal thinking and behavior in children, adolescents, and young adults taking antidepressants.
|
Suicidal Thoughts and Behaviors in Children, Adolescents, and Young Adults
- Worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior.
- Pooled analyses of short‑term placebo‑controlled trials of antidepressant drugs (selective serotonin reuptake inhibitors [SSRIs] and others) show that these drugs *Increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with MDD and other psychiatric disorders. Short-term clinical trials did not show an increase in the risk of suicidality with antidepressants compared with placebo in adults beyond age 24; there was a reduction with antidepressants compared with placebo in adults aged 65 and older.
- The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short‑term trials of 9 antidepressant drugs in over 4,400 subjects. The pooled analyses of placebo‑controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short‑term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 subjects. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger subjects for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs. placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1,000 subjects treated) are provided in Table 1
{
Adverse Reactions
Clinical Trials Experience
Central Nervous System
- Confusion (major depressive disorder, 8% ), dizziness (6% to 11%), headache (25% to 34% ), insomnia (11% to 20% )
Cardiovascular
- Tachycardia (major depressive disorder, 11% )
Respiratory
- Nasopharyngitis (seasonal affective disorder, 13% ), pharyngitis (major depressive disorder, 3% to 11% ), upper respiratory infection (seasonal affective disorder, 9% )
Gastrointestinal
- Abdominal pain (2% to 9%), constipation (5% to 10%), nausea (13% to 18%), xerostomia (17% to 26%)
Endocrine metabolic
- Weight gain (2% to 9% ), weight loss (major depressive disorder, 14% to 19% )
Psychiatric
- Agitation (2% to 9%)
Postmarketing Experience
Central Nervous System
- Aggression, coma, completed suicide, delirium, dream abnormalities, paranoid ideation, paresthesia, restlessness, suicide attempt, unmasking of tardive dyskinesia
Cardiovascular
- (list/description of adverse reactions)
Respiratory
- Hypertension (in some cases severe), orthostatic hypotension, third degree heart block.
Gastrointestinal
Body (General)
- Arthralgia, myalgia, and fever with rash and other symptoms suggestive of delayed hypersensitivity. These symptoms may resemble serum sickness.
Endocrine
Hemic and Lymphatic
- Ecchymosis, leukocytosis, leukopenia, thrombocytopenia. Altered PT and/or INR, infrequently associated with hemorrhagic or thrombotic complications, were observed when bupropion was coadministered with warfarin.
Musculoskeletal
Skin and Appendages
Special Senses
- Tinnitus, increased intraocular pressure.
Drug Interactions
- Potential for Other Drugs to Affect Bupropion
- Bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between bupropion and drugs that are inhibitors or inducers of CYP2B6.
- Inhibitors of CYP2B6:Ticlopidine and Clopidogrel: Concomitant treatment with these drugs can increase bupropion exposure but decrease hydroxybupropion exposure. Based on clinical response, dosage adjustment of bupropion may be necessary when coadministered with CYP2B6 inhibitors (e.g., ticlopidine or clopidogrel) [see Clinical Pharmacology].
- Inducers of CYP2B6:Ritonavir, Lopinavir, and Efavirenz: Concomitant treatment with these drugs can decrease bupropion and hydroxybupropion exposure. Dosage increase of bupropion may be necessary when coadministered with ritonavir, lopinavir, or efavirenz [see Clinical Pharmacology] but should not exceed the maximum recommended dose.
- Carbamazepine, Phenobarbital, Phenytoin: While not systematically studied, these drugs may induce the metabolism of bupropion and may decrease bupropion exposure [see Clinical Pharmacology]. If bupropion is used concomitantly with a CYP inducer, it may be necessary to increase the dose of bupropion, but the maximum recommended dose should not be exceeded.
- Potential for Bupropion to Affect Other Drugs
- Drugs Metabolized by CYP2D6: Bupropion and its metabolites (erythrohydrobupropion, threohydrobupropion, hydroxybupropion) are CYP2D6 inhibitors. Therefore, coadministration of bupropion with drugs that are metabolized by CYP2D6 can increase the exposures of drugs that are substrates of CYP2D6. Such drugs include certain antidepressants (e.g., venlafaxine, nortriptyline, imipramine, desipramine, paroxetine, fluoxetine, and sertraline), antipsychotics (e.g., haloperidol, risperidone, thioridazine), beta-blockers (e.g., metoprolol), and Type 1C antiarrhythmics (e.g., propafenone and flecainide). When used concomitantly with bupropion, it may be necessary to decrease the dose of these CYP2D6 substrates, particularly for drugs with a narrow therapeutic index.
- Drugs that require metabolic activation by CYP2D6 to be effective (e.g., tamoxifen) theoretically could have reduced efficacy when administered concomitantly with inhibitors of CYP2D6 such as bupropion. Patients treated concomitantly with bupropion and such drugs may require increased doses of the drug see Clinical Pharmacology .
- Drugs That Lower Seizure Threshold
- Use extreme caution when coadministering bupropion with other drugs that lower seizure threshold (e.g., other bupropion products, antipsychotics, antidepressants, theophylline, or systemic corticosteroids). Use low initial doses and increase the dose gradually [see Contraindications and Warnings and Precautions].
- Dopaminergic Drugs (Levodopa and Amantadine)
- Bupropion, levodopa, and amantadine have dopamine agonist effects. CNS toxicity has been reported when bupropion was coadministered with levodopa or amantadine. Adverse reactions have included restlessness, agitation, tremor, ataxia, gait disturbance, vertigo, and dizziness. It is presumed that the toxicity results from cumulative dopamine agonist effects. Use caution when administering bupropion concomitantly with these drugs.
- Bupropion inhibits the reuptake of dopamine and norepinephrine. Concomitant use of MAOIs and bupropion is contraindicated because there is an increased risk of hypertensive reactions if bupropion is used concomitantly with MAOIs. Studies in animals demonstrate that the acute toxicity of bupropion is enhanced by the MAO inhibitor phenelzine. At least 14 days should elapse between discontinuation of an MAOI intended to treat depression and initiation of treatment with bupropion. Conversely, at least 14 days should be allowed after stopping bupropion before starting an MAOI antidepressant [see Dosage and Administration and Contraindications].
- Drug-Laboratory Test Interactions
- False-positive urine immunoassay screening tests for amphetamines have been reported in patients taking bupropion. This is due to lack of specificity of some screening tests. False-positive test results may result even following discontinuation of bupropion therapy. Confirmatory tests, such as gas chromatography/mass spectrometry, will distinguish bupropion from amphetamines.
Use in Specific Populations
Pregnancy
- Risk Summary:Data from epidemiological studies of pregnant women exposed to bupropion in the first trimester indicate no increased risk of congenital malformations overall. All pregnancies, regardless of drug exposure, have a background rate of 2% to 4% for major malformations, and 15% to 20% for pregnancy loss. No clear evidence of teratogenic activity was found in reproductive developmental studies conducted in rats and rabbits; however, in rabbits, slightly increased incidences of fetal malformations and skeletal variations were observed at doses approximately equal to the maximum recommended human dose (MRHD) and greater and decreased fetal weights were seen at doses twice the MRHD and greater. Bupropion should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Clinical Considerations:Consider the risks of untreated depression when discontinuing or changing treatment with antidepressant medications during pregnancy and postpartum.
- Human Data:Data from the international bupropion Pregnancy Registry (675 first-trimester exposures) and a retrospective cohort study using the United Healthcare database (1,213 first trimester exposures) did not show an increased risk for malformations overall.
- No increased risk for cardiovascular malformations overall has been observed after bupropion exposure during the first trimester. The prospectively observed rate of cardiovascular malformations in pregnancies with exposure to bupropion in the first trimester from the international Pregnancy Registry was 1.3% (9 cardiovascular malformations/675 first-trimester maternal bupropion exposures), which is similar to the background rate of cardiovascular malformations (approximately 1%). Data from the United Healthcare database and a case-control study (6,853 infants with cardiovascular malformations and 5,763 with non-cardiovascular malformations) from the National Birth Defects Prevention Study (NBDPS) did not show an increased risk for cardiovascular malformations overall after bupropion exposure during the first trimester.
- Study findings on bupropion exposure during the first trimester and risk for left ventricular outflow tract obstruction (LVOTO) are inconsistent and do not allow conclusions regarding a possible association. The United Healthcare database lacked sufficient power to evaluate this association; the NBDPS found increased risk for LVOTO (n = 10; adjusted OR = 2.6; 95% CI: 1.2, 5.7), and the Slone Epidemiology case control study did not find increased risk for LVOTO.
- Study findings on bupropion exposure during the first trimester and risk for ventricular septal defect (VSD) are inconsistent and do not allow conclusions regarding a possible association. The Slone Epidemiology Study found an increased risk for VSD following first trimester maternal bupropion exposure (n = 17; adjusted OR = 2.5; 95% CI: 1.3, 5.0) but did not find increased risk for any other cardiovascular malformations studied (including LVOTO as above). The NBDPS and United Healthcare database study did not find an association between first trimester maternal bupropion exposure and VSD.
- For the findings of LVOTO and VSD, the studies were limited by the small number of exposed cases, inconsistent findings among studies, and the potential for chance findings from multiple comparisons in case control studies.
Animal Data:In studies conducted in rats and rabbits, bupropion was administered orally during the period of organogenesis at doses of up to 450 and 150 mg/kg/day, respectively (approximately 11 and 7 times the MRHD, respectively, on a mg/m2basis). No clear evidence of teratogenic activity was found in either species; however, in rabbits, slightly increased incidences of fetal malformations and skeletal variations were observed at the lowest dose tested (25 mg/kg/day, approximately equal to the MRHD on a mg/m2 basis) and greater. Decreased fetal weights were observed at 50 mg/kg and greater.
When rats were administered bupropion at oral doses of up to 300 mg/kg/day (approximately 7 times the MRHD on a mg/m2basis) prior to mating and throughout pregnancy and lactation, there were no apparent adverse effects on offspring development.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Bupropion in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Bupropion during labor and delivery.
Nursing Mothers
- Nursing Mothers
- Bupropion and its metabolites are present in human milk. In a lactation study of 10 women, levels of orally dosed bupropion and its active metabolites were measured in expressed milk. The average daily infant exposure (assuming 150 mL/kg daily consumption) to bupropion and its active metabolites was 2% of the maternal weight-adjusted dose. Exercise caution when bupropion is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established [see Boxed Warning and Warnings and Precautions].
Geriatic Use
- Geriatric Use
- Of the approximately 6,000 subjects who participated in clinical trials with bupropion sustained-release tablets (depression and smoking cessation trials), 275 were aged ≥65 years and 47 were aged ≥75 years. In addition, several hundred subjects aged ≥65 years participated in clinical trials using the immediate-release formulation of bupropion (depression trials). No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
- Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and excreted by the kidneys. The risk of adverse reactions may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, it may be necessary to consider this factor in dose selection; it may be useful to monitor renal function [see Dosage and Administration , Use in Specific Populations , and Clinical Pharmacology ].
Gender
There is no FDA guidance on the use of Bupropion with respect to specific gender populations.
Race
There is no FDA guidance on the use of Bupropion with respect to specific racial populations.
Renal Impairment
- Renal Impairment
- Consider a reduced dose and/or dosing frequency of bupropion in patients with renal impairment (Glomerular Filtration Rate: <90 mL/min). Bupropion and its metabolites are cleared renally and may accumulate in such patients to a greater extent than usual. Monitor closely for adverse reactions that could indicate high bupropion or metabolite exposures [see Dosage and Administration and Clinical Pharmacology ].
Hepatic Impairment
- Hepatic Impairment
- In patients with moderate to severe hepatic impairment (Child-Pugh score: 7 to 15), the maximum dose of bupropion is 75 mg daily. In patients with mild hepatic impairment (Child-Pugh score: 5 to 6), consider reducing the dose and/or frequency of dosing [see Dosage and Administration and Clinical Pharmacology].
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Bupropion in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Bupropion in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Bupropion Administration in the drug label.
Monitoring
There is limited information regarding Bupropion Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Bupropion and IV administrations.
Overdosage
- Human Overdose Experience
- Overdoses of up to 30 grams or more of bupropion have been reported. Seizure was reported in approximately one-third of all cases. Other serious reactions reported with overdoses of bupropion alone included hallucinations, loss of consciousness, sinus tachycardia, and ECG changes such as conduction disturbances (including QRS prolongation) or arrhythmias. Fever, muscle rigidity, rhabdomyolysis, hypotension, stupor, coma, and respiratory failure have been reported mainly when bupropion was part of multiple drug overdoses.
- Although most patients recovered without sequelae, deaths associated with overdoses of bupropion alone have been reported in patients ingesting large doses of the drug. Multiple uncontrolled seizures, bradycardia, cardiac failure, and cardiac arrest prior to death were reported in these patients.
- Overdosage Management
- Consult a Certified Poison Control Center for up-to-date guidance and advice. Telephone numbers for certified poison control centers are listed in the Physician’s Desk Reference (PDR). Call 1-800-222-1222 or refer to www.poison.org.
- There are no known antidotes for bupropion. In case of an overdose, provide supportive care, including close medical supervision and monitoring. Consider the possibility of multiple drug overdose. Ensure an adequate airway, oxygenation, and ventilation. Monitor cardiac rhythm and vital signs. Induction of emesis is not recommended.
Pharmacology
Mechanism of Action
The exact mechanism of the antidepressant action of bupropion is not known, but is presumed to be related to noradrenergic and/or dopaminergic mechanisms. Bupropion is a relatively weak inhibitor of the neuronal reuptake of norepinephrine and dopamine, and does not inhibit the reuptake of serotonin. Bupropion does not inhibit monoamine oxidase.
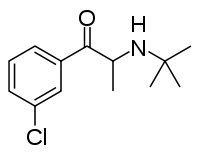
Structure
There is limited information regarding Bupropion Structure in the drug label.
Pharmacodynamics
There is limited information regarding Bupropion Pharmacodynamics in the drug label.
Pharmacokinetics
- Bupropion is a racemic mixture. The pharmacological activity and pharmacokinetics of the individual enantiomers have not been studied. The mean elimination half-life (±SD) of bupropion after chronic dosing is 21 (±9) hours, and steady-state plasma concentrations of bupropion are reached within 8 days.
- Absorption
- The absolute bioavailability of bupropion in humans has not been determined because an intravenous formulation for human use is not available. However, it appears likely that only a small proportion of any orally administered dose reaches the systemic circulation intact. In rat and dog studies, the bioavailability of bupropion ranged from 5% to 20%.
In humans, following oral administration of bupropion, peak plasma bupropion concentrations are usually achieved within 2 hours. Plasma bupropion concentrations are dose‑proportional following single doses of 100 to 250 mg; however, it is not known if the proportionality between dose and plasma level is maintained in chronic use.
- Distribution
- In vitro tests show that bupropion is 84% bound to human plasma proteins at concentrations up to 200 mcg/mL. The extent of protein binding of the hydroxybupropion metabolite is similar to that for bupropion, whereas the extent of protein binding of the threohydrobupropion metabolite is about half that seen with bupropion.
- Metabolism
- Bupropion is extensively metabolized in humans. Three metabolites are active: hydroxybupropion, which is formed via hydroxylation of the tert-butyl group of bupropion, and the amino-alcohol isomers threohydrobupropion and erythrohydrobupropion, which are formed via reduction of the carbonyl group. In vitro findings suggest that CYP2B6 is the principal isoenzyme involved in the formation of hydroxybupropion, while cytochrome P450 enzymes are not involved in the formation of threohydrobupropion. Oxidation of the bupropion side chain results in the formation of a glycine conjugate of meta-chlorobenzoic acid, which is then excreted as the major urinary metabolite. The potency and toxicity of the metabolites relative to bupropion have not been fully characterized. However, it has been demonstrated in an antidepressant screening test in mice that hydroxybupropion is one‑half as potent as bupropion, while threohydrobupropion and erythrohydrobupropion are 5-fold less potent than bupropion. This may be of clinical importance because the plasma concentrations of the metabolites are as high as or higher than those of bupropion.
- Following a single dose in humans, peak plasma concentrations of hydroxybupropion occur approximately 3 hours after administration of bupropion and are approximately 10 times the peak level of the parent drug at steady state. The elimination half‑life of hydroxybupropion is approximately 20 (±5) hours, and its AUC at steady state is about 17 times that of bupropion. The times to peak concentrations for the erythrohydrobupropion and threohydrobupropion metabolites are similar to that of the hydroxybupropion metabolite. However, their elimination half‑lives are longer, 33 (±10) and 37 (±13) hours, respectively, and steady‑state AUCs are 1.5 and 7 times that of bupropion, respectively.
- Bupropion and its metabolites exhibit linear kinetics following chronic administration of 300 to 450 mg per day.
- Elimination
- Following oral administration of 200 mg of 14C-bupropion in humans, 87% and 10% of the radioactive dose were recovered in the urine and feces, respectively. Only 0.5% of the oral dose was excreted as unchanged bupropion.
- Population Subgroups
- Factors or conditions altering metabolic capacity (e.g., liver disease, congestive heart failure [CHF], age, concomitant medications, etc.) or elimination may be expected to influence the degree and extent of accumulation of the active metabolites of bupropion. The elimination of the major metabolites of bupropion may be affected by reduced renal or hepatic function because they are moderately polar compounds and are likely to undergo further metabolism or conjugation in the liver prior to urinary excretion.
- Renal Impairment
- There is limited information on the pharmacokinetics of bupropion in patients with renal impairment. An inter-trial comparison between normal subjects and subjects with end-stage renal failure demonstrated that the parent drug Cmax and AUC values were comparable in the 2 groups, whereas the hydroxybupropion and threohydrobupropion metabolites had a 2.3- and 2.8-fold increase, respectively, in AUC for subjects with end-stage renal failure. A second trial, comparing normal subjects and subjects with moderate‑to‑severe renal impairment (GFR 30.9 10.8 mL/min) showed that after a single 150-mg dose of sustained-release bupropion, exposure to bupropion was approximately 2-fold higher in subjects with impaired renal function, while levels of the hydroxybupropion and threo/erythrohydrobupropion (combined) metabolites were similar in the 2 groups. Bupropion is extensively metabolized in the liver to active metabolites, which are further metabolized and subsequently excreted by the kidneys. The elimination of the major metabolites of bupropion may be reduced by impaired renal function. WELLBUTRIN should be used with caution in patients with renal impairment and a reduced frequency and/or dose should be considered [see Use in Specific Populations].
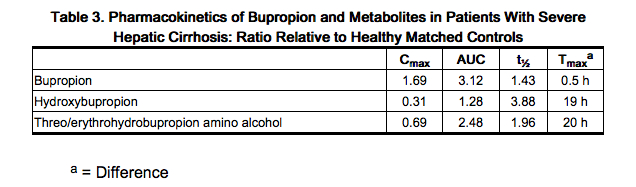
- Hepatic Impairment
- The effect of hepatic impairment on the pharmacokinetics of bupropion was characterized in 2 single-dose trials, one in subjects with alcoholic liver disease and one in subjects with mild-to-severe cirrhosis. The first trial demonstrated that the half‑life of hydroxybupropion was significantly longer in 8 subjects with alcoholic liver disease than in 8 healthy volunteers (32 ± 14 hours versus 21 ± 5 hours, respectively). Although not statistically significant, the AUCs for bupropion and hydroxybupropion were more variable and tended to be greater (by 53% to 57%) in volunteers with alcoholic liver disease. The differences in half‑life for bupropion and the other metabolites in the 2 groups were minimal.
- The second trial demonstrated no statistically significant differences in the pharmacokinetics of bupropion and its active metabolites in 9 subjects with mild-to-moderate hepatic cirrhosis compared with 8 healthy volunteers. However, more variability was observed in some of the pharmacokinetic parameters for bupropion (AUC, Cmax, and Tmax) and its active metabolites (t½) in subjects with mild-to-moderate hepatic cirrhosis. In subjects with severe hepatic cirrhosis, significant alterations in the pharmacokinetics of bupropion and its metabolites were seen (Table 3).
-
- During a chronic dosing trial with bupropion in 14 depressed subjects with left ventricular dysfunction (history of CHF or an enlarged heart on x-ray), there was no apparent effect on the pharmacokinetics of bupropion or its metabolites, compared with healthy volunteers.
- Age
- The effects of age on the pharmacokinetics of bupropion and its metabolites have not been fully characterized, but an exploration of steady‑state bupropion concentrations from several depression efficacy trials involving subjects dosed in a range of 300 to 750 mg per day, on a 3 times daily schedule, revealed no relationship between age (18 to 83 years) and plasma concentration of bupropion. A single‑dose pharmacokinetic trial demonstrated that the disposition of bupropion and its metabolites in elderly subjects was similar to that of younger subjects. These data suggest there is no prominent effect of age on bupropion concentration; however, another single- and multiple-dose pharmacokinetics trial suggested that the elderly are at increased risk for accumulation of bupropion and its metabolites [see Use in Specific Populations].
- Gender
- Pooled analysis of bupropion pharmacokinetic data from 90 healthy male and 90 healthy female volunteers revealed no sex-related differences in the peak plasma concentrations of bupropion. The mean systemic exposure (AUC) was approximately 13% higher in male volunteers compared with female volunteers. The clinical significance of this finding is unknown.
- Smokers: The effects of cigarette smoking on the pharmacokinetics of bupropion were studied in 34 healthy male and female volunteers; 17 were chronic cigarette smokers and 17 were nonsmokers. Following oral administration of a single 150-mg dose of bupropion, there were no statistically significant differences in Cmax, half-life, Tmax, AUC, or clearance of bupropion or its active metabolites between smokers and nonsmokers.
- Drug Interactions:Potential for Other Drugs to Affect Bupropion: In vitro studies indicate that bupropion is primarily metabolized to hydroxybupropion by CYP2B6. Therefore, the potential exists for drug interactions between bupropion and drugs that are inhibitors or inducers of CYP2B6. In addition, in vitro studies suggest that paroxetine, sertraline, norfluoxetine, fluvoxamine, and nelfinavir inhibit the hydroxylation of bupropion.
- Inhibitors of CYP2B6
- Ticlopidine, Clopidogrel: In a trial in healthy male volunteers, clopidogrel 75 mg once daily or ticlopidine 250 mg twice daily increased exposures (Cmax and AUC) of bupropion by 40% and 60% for clopidogrel, and by 38% and 85% for ticlopidine, respectively. The exposures (Cmax and AUC) of hydroxybupropion were decreased 50% and 52%, respectively, by clopidogrel, and 78% and 84%, respectively, by ticlopidine. This effect is thought to be due to the inhibition of the CYP2B6-catalyzed bupropion hydroxylation.
- Inhibitors of CYP2B6
-
- Prasugrel is a weak inhibitor of CYP2B6. In healthy subjects, prasugrel increased bupropion Cmax and AUC values by 14% and 18%, respectively, and decreased Cmax and AUC values of hydroxybupropion, an active metabolite of bupropion, by 32% and 24%, respectively.
-
- The threohydrobupropion metabolite of bupropion does not appear to be produced by cytochrome P450 enzymes. The effects of concomitant administration of cimetidine on the pharmacokinetics of bupropion and its active metabolites were studied in 24 healthy young male volunteers. Following oral administration of bupropion 300 mg with and without cimetidine 800 mg, the pharmacokinetics of bupropion and hydroxybupropion were unaffected. However, there were 16% and 32% increases in the AUC and Cmax, respectively of the combined moieties of threohydrobupropion and erythrohydrobupropion.
-
- Citalopram did not affect the pharmacokinetics of bupropion and its three metabolites.
- Inducers of CYP2B6
-
- In a healthy volunteer trial, ritonavir 100 mg twice daily reduced the AUC and Cmax of bupropion by 22% and 21%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 23%, the threohydrobupropion decreased by 38%, and the erythrohydrobupropion decreased by 48%. In a second healthy volunteer trial, ritonavir 600 mg twice daily decreased the AUC and the Cmax of bupropion by 66% and 62%, respectively. The exposure of the hydroxybupropion metabolite was decreased by 78%, the threohydrobupropion decreased by 50%, and the erythrohydrobupropion decreased by 68%.
- In another healthy volunteer trial, lopinavir 400 mg/ritonavir 100 mg twice daily decreased bupropion AUC and Cmax by 57%. The AUC and Cmax of hydroxybupropion were decreased by 50% and 31%, respectively.
-
- In a trial in healthy volunteers, efavirenz 600 mg once daily for 2 weeks reduced the AUC and Cmax of bupropion by approximately 55% and 34%, respectively. The AUC of hydroxybupropion was unchanged, whereas Cmax of hydroxybupropion was increased by 50%.
-
- While not systematically studied, these drugs may induce the metabolism of bupropion.
- Potential for WELLBUTRIN to Affect Other Drugs
- Animal data indicated that bupropion may be an inducer of drug-metabolizing enzymes in humans. In one trial, following chronic administration of bupropion 100 mg three times daily to 8 healthy male volunteers for 14 days, there was no evidence of induction of its own metabolism. Nevertheless, there may be potential for clinically important alterations of blood levels of co-administered drugs.
- Drugs Metabolized by CYP2D6
- In vitro, bupropion and its metabolites (erythrohydrobupropion, threohydrobupropion, hydroxybupropion) are CYP2D6 inhibitors. In a clinical trial of 15 male subjects (ages 19 to 35 years) who were extensive metabolizers of CYP2D6, bupropion 300 mg per day followed by a single dose of 50 mg desipramine increased the Cmax, AUC, and t1/2 of desipramine by an average of approximately 2-, 5-, and 2-fold, respectively. The effect was present for at least 7 days after the last dose of bupropion. Concomitant use of bupropion with other drugs metabolized by CYP2D6 has not been formally studied.
-
- Although citalopram is not primarily metabolized by CYP2D6, in one trial bupropion increased the Cmax and AUC of citalopram by 30% and 40%, respectively.
-
- Multiple oral doses of bupropion had no statistically significant effects on the single-dose pharmacokinetics of lamotrigine in 12 healthy volunteers.
Nonclinical Toxicology
- Carcinogenesis, Mutagenesis, Impairment of Fertility
- Lifetime carcinogenicity studies were performed in rats and mice at bupropion doses up to 300 and 150 mg/kg/day, respectively. These doses are approximately 7 and 2 times the MRHD, respectively, on a mg/m2 basis. In the rat study there was an increase in nodular proliferative lesions of the liver at doses of 100 to 300 mg/kg/day (approximately 2 to 7 times the MRHD on a mg/m2 basis); lower doses were not tested. The question of whether or not such lesions may be precursors of neoplasms of the liver is currently unresolved. Similar liver lesions were not seen in the mouse study, and no increase in malignant tumors of the liver and other organs was seen in either study.
- Bupropion produced a positive response (2 to 3 times control mutation rate) in 2 of 5 strains in the Ames bacterial mutagenicity assay. Bupropion produced an increase in chromosomal aberrations in 1 of 3 in vivo rat bone marrow cytogenetic studies.
- A fertility study in rats at doses up to 300 mg/kg/day revealed no evidence of impaired fertility.
Clinical Studies
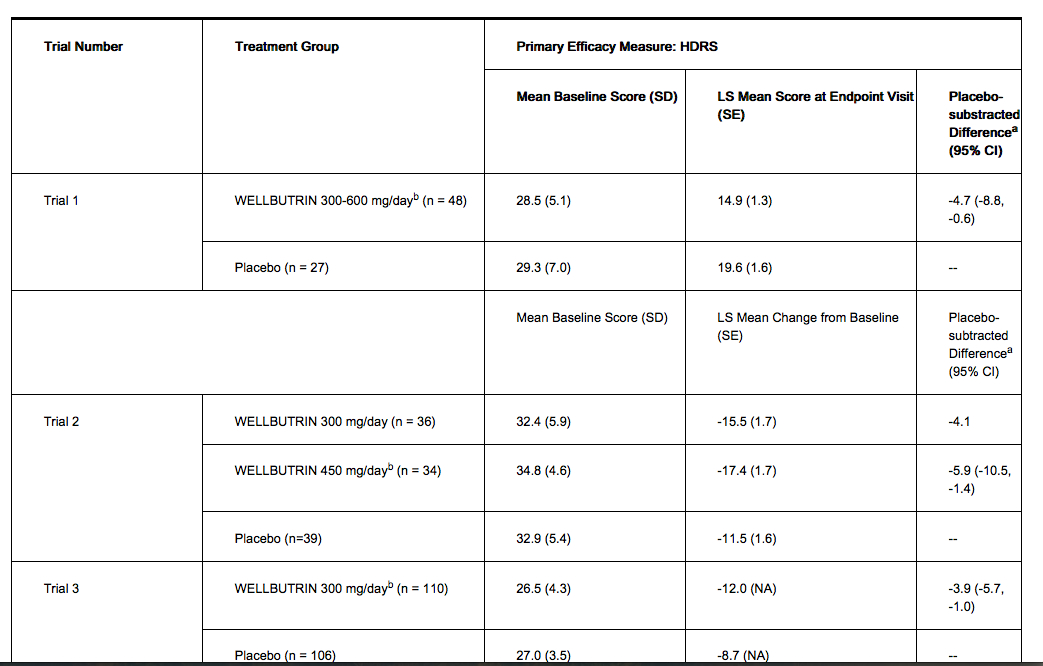
The efficacy of WELLBUTRIN in the treatment of major depressive disorder was established in two 4‑week, placebo‑controlled trials in adult inpatients with MDD (Trials 1 and 2 in Table 4) and in one 6‑week, placebo‑controlled trial in adult outpatients with MDD (Trial 3 in Table 4). In the first trial, the dose range of WELLBUTRIN was 300 mg to 600 mg per day administered in 3 divided doses; 78% of subjects were treated with doses of 300 mg to 450 mg per day. The trial demonstrated the efficacy of WELLBUTRIN as measured by the Hamilton Depression Rating Scale (HDRS) total score, the HDRS depressed mood item (item 1), and the Clinical Global Impressions-severity score (CGI-S). The second trial included 2 doses of WELLBUTRIN (300 and 450 mg per day) and placebo. This trial demonstrated the effectiveness of WELLBUTRIN for only the 450‑mg-per-day dose. The efficacy results were statistically significant for the HDRS total score and the CGI-S score, but not for HDRS item 1. In the third trial, outpatients were treated with 300 mg per day of WELLBUTRIN. This trial demonstrated the efficacy of WELLBUTRIN as measured by the HDRS total score, the HDRS item 1, the Montgomery‑Asberg Depression Rating Scale (MADRS), the CGI-S score, and the CGI-Improvement Scale (CGI-I) score. Effectiveness of WELLBUTRIN in long‑term use, that is, for more than 6 weeks, has not been systematically evaluated in controlled trials.
Table 4. Efficacy of WELLBUTRIN for the Treatment of Major Depressive Disorder
How Supplied
- WELLBUTRIN Tablets, 75 mg of bupropion hydrochloride, are yellow‑gold, round, biconvex tablets printed with “WELLBUTRIN 75” in bottles of 100 (NDC 0173-0177-55).
- WELLBUTRIN Tablets, 100 mg of bupropion hydrochloride, are red, round, biconvex tablets printed with “WELLBUTRIN 100” in bottles of 100 (NDC 0173-0178-55).
Storage
- Store at room temperature, 20° to 25°C (68° to 77°F); excursions permitted between 15°C and 30°C (59°F and 86°F) [See USP Controlled Room Temperature]. Protect from light and moisture.
Images
Drug Images
{{#ask: Page Name::Bupropion |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Bupropion |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
For patient information, please click here.
- Advise the patient to read the FDA-approved patient labeling (Medication Guide)
- Inform patients, their families, and their caregivers about the benefits and risks associated with treatment with WELLBUTRIN and counsel them in its appropriate use.
- A patient Medication Guide about “Antidepressant Medicines, Depression and Other Serious Mental Illnesses, and Suicidal Thoughts or Actions,” “Quitting Smoking, Quit-Smoking Medications, Changes in Thinking and Behavior, Depression, and Suicidal Thoughts or Actions,” and “What Other Important Information Should I Know About WELLBUTRIN?” is available for WELLBUTRIN. Instruct patients, their families, and their caregivers to read the Medication Guide and assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.Advise patients regarding the following issues and to alert their prescriber if these occur while taking WELLBUTRIN.
- Suicidal Thoughts and Behaviors
- Instruct patients, their families, and/or their caregivers to be alert to the emergence of anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, mania, other unusual changes in behavior, worsening of depression, and suicidal ideation, especially early during antidepressant treatment and when the dose is adjusted up or down. Advise families and caregivers of patients to observe for the emergence of such symptoms on a day-to-day basis, since changes may be abrupt. Such symptoms should be reported to the patient’s prescriber or healthcare professional, especially if they are severe, abrupt in onset, or were not part of the patient’s presenting symptoms. Symptoms such as these may be associated with an increased risk for suicidal thinking and behavior and indicate a need for very close monitoring and possibly changes in the medication.
- Neuropsychiatric Symptoms and Suicide Risk in Smoking Cessation Treatment
- Although WELLBUTRIN is not indicated for smoking cessation treatment, it contains the same active ingredient as ZYBAN® which is approved for this use. Advise patients, families and caregivers that quitting smoking, with or without ZYBAN, may trigger nicotine withdrawal symptoms (e.g., including depression or agitation), or worsen pre-existing psychiatric illness. Some patients have experienced changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, aggression, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide when attempting to quit smoking while taking ZYBAN. If patients develop agitation, hostility, depressed mood, or changes in thinking or behavior that are not typical for them, or if patients develop suicidal ideation or behavior, they should be urged to report these symptoms to their healthcare provider immediately.
- Severe Allergic Reactions
- Educate patients on the symptoms of hypersensitivity and to discontinue WELLBUTRIN if they have a severe allergic reaction.
- Seizure
- Instruct patients to discontinue and not restart WELLBUTRIN if they experience a seizure while on treatment. Advise patients that the excessive use or abrupt discontinuation of alcohol, benzodiazepines, antiepileptic drugs, or sedatives/hypnotics can increase the risk of seizure. Advise patients to minimize or avoid use of alcohol.
- Bupropion-Containing Products
- Educate patients that WELLBUTRIN contains the same active ingredient (bupropion hydrochloride) found in ZYBAN, which is used as an aid to smoking cessation treatment, and that WELLBUTRIN should not be used in combination with ZYBAN or any other medications that contain bupropion (such as WELLBUTRIN SR®, the sustained-release formulation and WELLBUTRIN XL® or FORFIVO XL™, the extended-release formulations, and APLENZIN®, the extended-release formulation of bupropion hydrobromide). In addition, there are a number of generic bupropion HCl products for the immediate-, sustained-, and extended-release formulations.
- Potential for Cognitive and Motor Impairment
- Advise patients that any CNS‑active drug like WELLBUTRIN may impair their ability to perform tasks requiring judgment or motor and cognitive skills. Advise patients that until they are reasonably certain that WELLBUTRIN does not adversely affect their performance, they should refrain from driving an automobile or operating complex, hazardous machinery. WELLBUTRIN may lead to decreased alcohol tolerance.
- Concomitant Medications
- Counsel patients to notify their healthcare provider if they are taking or plan to take any prescription or over‑the‑counter drugs because WELLBUTRIN and other drugs may affect each others’ metabolisms.
- Pregnancy
- Advise patients to notify their healthcare provider if they become pregnant or intend to become pregnant during therapy.
Precautions for Nursing Mothers: Advise patients that WELLBUTRIN is present in human milk in small amounts.
- Storage Information
- Instruct patients to store WELLBUTRIN at room temperature, between 59°F and 86°F (15°C to 30°C) and keep the tablets dry and out of the light.
- Administration Information
- Instruct patients to take WELLBUTRIN in equally divided doses 3 or 4 times a day, with doses separated by least 6 hours to minimize the risk of seizure. Instruct patients if they miss a dose, not to take an extra tablet to make up for the missed dose and to take the next tablet at the regular time because of the dose-related risk of seizure. Instruct patients that WELLBUTRIN Tablets should be swallowed whole and not crushed, divided, or chewed. WELLBUTRIN can be taken with or without food.
Precautions with Alcohol
- Use With Alcohol
- In postmarketing experience, there have been rare reports of adverse neuropsychiatric events or reduced alcohol tolerance in patients who were drinking alcohol during treatment with bupropion. The consumption of alcohol during treatment with bupropion should be minimized or avoided.
Brand Names
There is limited information regarding Bupropion Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Bupropion Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 1.2 1.3 "Zyban 150 mg prolonged release film-coated tablets - Summary of Product Characteristics (SPC)". electronic Medicines Compendium. GlaxoSmithKline UK. 1 August 2013. Retrieved 22 October 2013.
- ↑ 2.0 2.1 "Prexaton Bupropion hydrochloride PRODUCT INFORMATION". TGA eBusiness Services. Ascent Pharma Pty Ltd. 2 October 2012. Retrieved 22 October 2013.
- ↑ 3.0 3.1 3.2 3.3 "BUPROPION HYDROCHLORIDE tablet, film coated [Sandoz Inc]". DailyMed. Sandoz, Inc. April 2013. Retrieved 22 October 2013.
- ↑ Template:Cite isbn
- ↑ 5.0 5.1 5.2 "PRODUCT INFORMATION ZYBAN® SUSTAINED RELEASE TABLETS". TGA eBusiness Services. Aspen Pharmacare Australia Pty Ltd. 19 April 2013. Retrieved 22 October 2013.
- ↑ "WELLBUTRIN (bupropion hydrochloride) tablet, film coated [GlaxoSmithKline LLC]". DailyMed. GlaxoSmithKline LLC. March 2013. Retrieved 22 October 2013.