Brugada syndrome electrocardiogram: Difference between revisions
m (Bot: Adding CME Category::Cardiology) |
|||
| (37 intermediate revisions by 5 users not shown) | |||
| Line 5: | Line 5: | ||
There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as [[ajmaline]] and [[flecainide]]. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as [[ajmaline]], [[flecainide]]) or it may be unmasked by various [[Brugada syndrome risk factors|triggers]] or [[Brugada syndrome risk factors|risk factors]]. | There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as [[ajmaline]] and [[flecainide]]. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as [[ajmaline]], [[flecainide]]) or it may be unmasked by various [[Brugada syndrome risk factors|triggers]] or [[Brugada syndrome risk factors|risk factors]]. | ||
Type 1 Brugada pattern is characterized by ST elevations in | ==Electrocardiogram== | ||
Type 1 Brugada pattern is characterized by ST elevations in leads V<sub>1</sub>-V<sub>3</sub> with a [[right bundle branch block]] ([[RBBB]]) like pattern, although it is actually a cause of "pseudo right bundle branch block" as electrocardiographically right bundle branch block is not actually present. A [[prolongation of the PR interval]] is also frequently seen. The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the [[ST segment]] elevation, while vagal stimulation worsens it. The administration of class Ia, Ic and III drugs increases the [[ST segment]] elevation, as does [[fever]]. Exercise decreases [[ST segment]] elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of [[ST segment]] elevation. When the heart rate decreases, the [[ST segment]] elevation increases and when the heart rate increases the [[ST segment]] elevation decreases. | |||
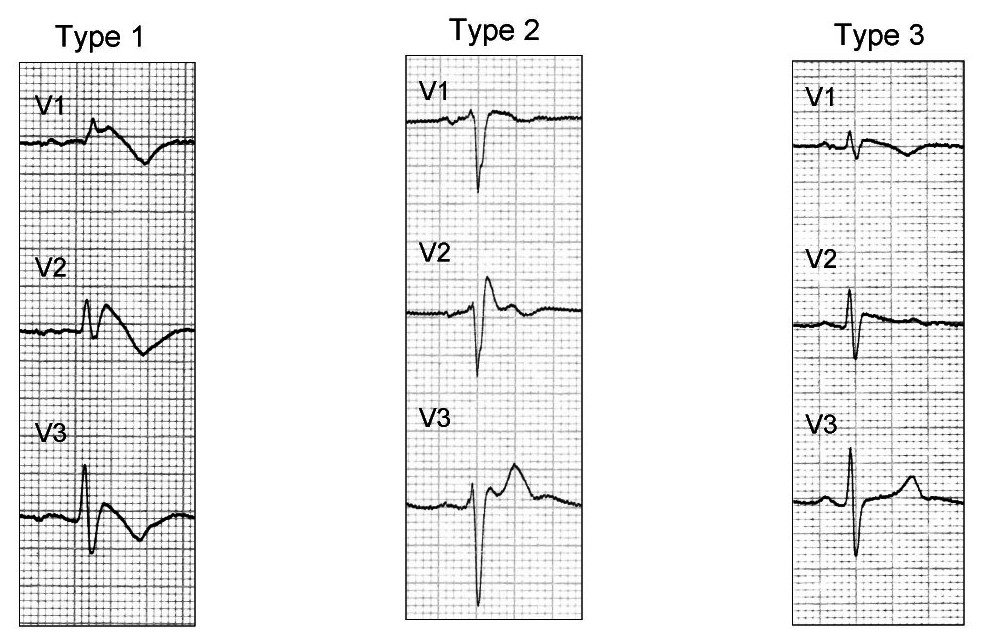
The three patterns of Brugada syndrome (Type I,II,III) are shown below: | The three patterns of Brugada syndrome (Type I,II,III) are shown below: | ||
[[File:Brugada type 123.jpg|center|500px]] | [[File:Brugada type 123.jpg|center|500px]] | ||
The table below is from ECGpedia and is adapted from Wilde et al.<ref name="pmid12417552">{{cite journal |author=Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA |title=Proposed diagnostic criteria for the Brugada syndrome: consensus report |journal=[[Circulation]] |volume=106 |issue=19 |pages=2514–9 |year=2002 |month=November |pmid=12417552 |doi= |url=http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=12417552 |issn= |accessdate=2012-10-14}}</ref> | |||
<center> | <center> | ||
{| class="wikitable" font-size="90%" | {| class="wikitable" font-size="90%" | ||
| Line 42: | Line 44: | ||
|} | |} | ||
</center> | </center> | ||
---- | |||
Brugada syndrome algorithm is shown below. | |||
[[Image:Brugada syndrome algorithm.png|center|500px]] | |||
==Type 1 Brugada Pattern== | |||
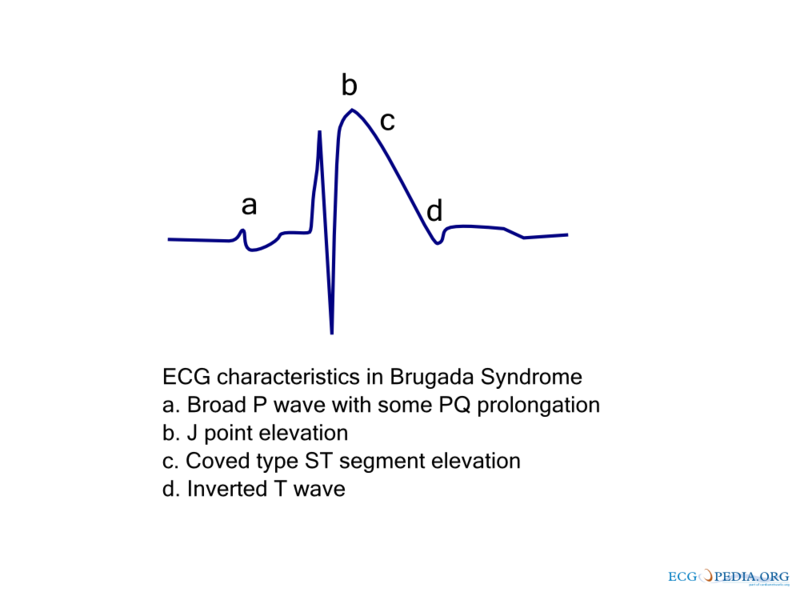
As shown by the tracing below, the EKG characteristics of Type 1 Brugada pattern include the following EKG findings in the right precordial leads (V<sub>1</sub>-V<sub>3</sub>): | |||
*a) A broad [[P-wave]] with some [[PR prolongation]] | |||
==Type 1 Brugada | |||
As shown by the tracing below, the EKG characteristics of Type 1 Brugada | |||
*a) A broad [[P-wave]] with some [[ | |||
*b) [[J point]] elevation in the right precordial leads (V<sub>1</sub>-V<sub>3</sub>) | *b) [[J point]] elevation in the right precordial leads (V<sub>1</sub>-V<sub>3</sub>) | ||
*c) Coved [[ST segment elevation]] | *c) Coved [[ST segment elevation]] | ||
| Line 66: | Line 59: | ||
[[File:Brugada ecg characteristics.png|center|500px]] | [[File:Brugada ecg characteristics.png|center|500px]] | ||
Slight [[QT prolongation]] may also be observed, particularly in the right precordial leads.<ref> <div>'' Alings M, Wilde A. “Brugada” syndrome: clinical data and suggested pathophysiological mechanism. Circulation''. '' 1999; 99: 666–673.''</div></ref><ref>''Bezzina C, Veldkamp MW, van Den Berg MP, Postma AV, Rook MB, Viersma JW, Van Langen IM, Tan-Sindhunata G, Bink-Boelkens MT, van Der Hout AH, Mannens MM, Wilde AA. A single Na(+) channel mutation causing both long-QT and Brugada syndromes. Circ Res''. '' 1999; 85: 1206–1213.''</ref><ref>''Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Brignole M, Giordano U, Giovannini T, Menozzi C, Bloise R, Crotti L, Terreni L, Schwartz PJ. Clinical and genetic heterogeneity of right bundle branch block and ST-segment elevation syndrome: a prospective evaluation of 52 families. Circulation''. '' 2000; 102: 2509–2515.''</ref> | |||
Typically these changes are in the right precordial leads but these EKG changes can occur in the inferior <ref name="pmid10695469">{{cite journal |author=Kalla H, Yan GX, Marinchak R |title=Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant? |journal=[[Journal of Cardiovascular Electrophysiology]] |volume=11 |issue=1 |pages=95–8 |year=2000 |month=January |pmid=10695469 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> or left precordial leads<ref name="pmid14661171">{{cite journal |author=Horigome H, Shigeta O, Kuga K, Isobe T, Sakakibara Y, Yamaguchi I, Matsui A |title=Ventricular fibrillation during anesthesia in association with J waves in the left precordial leads in a child with coarctation of the aorta |journal=[[Journal of Electrocardiology]] |volume=36 |issue=4 |pages=339–43 |year=2003 |month=October |pmid=14661171 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0022073603000797 |issn= |accessdate=2012-10-14}}</ref>. The fact that these cases may represent atypical variants of Brugada syndrome is supported by the observation that these cases were associated with [[SCN5A]] genetic abnormalities. | Typically these changes are in the right precordial leads but these EKG changes can occur in the inferior <ref name="pmid10695469">{{cite journal |author=Kalla H, Yan GX, Marinchak R |title=Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant? |journal=[[Journal of Cardiovascular Electrophysiology]] |volume=11 |issue=1 |pages=95–8 |year=2000 |month=January |pmid=10695469 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> or left precordial leads<ref name="pmid14661171">{{cite journal |author=Horigome H, Shigeta O, Kuga K, Isobe T, Sakakibara Y, Yamaguchi I, Matsui A |title=Ventricular fibrillation during anesthesia in association with J waves in the left precordial leads in a child with coarctation of the aorta |journal=[[Journal of Electrocardiology]] |volume=36 |issue=4 |pages=339–43 |year=2003 |month=October |pmid=14661171 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0022073603000797 |issn= |accessdate=2012-10-14}}</ref>. The fact that these cases may represent atypical variants of Brugada syndrome is supported by the observation that these cases were associated with [[SCN5A]] genetic abnormalities. | ||
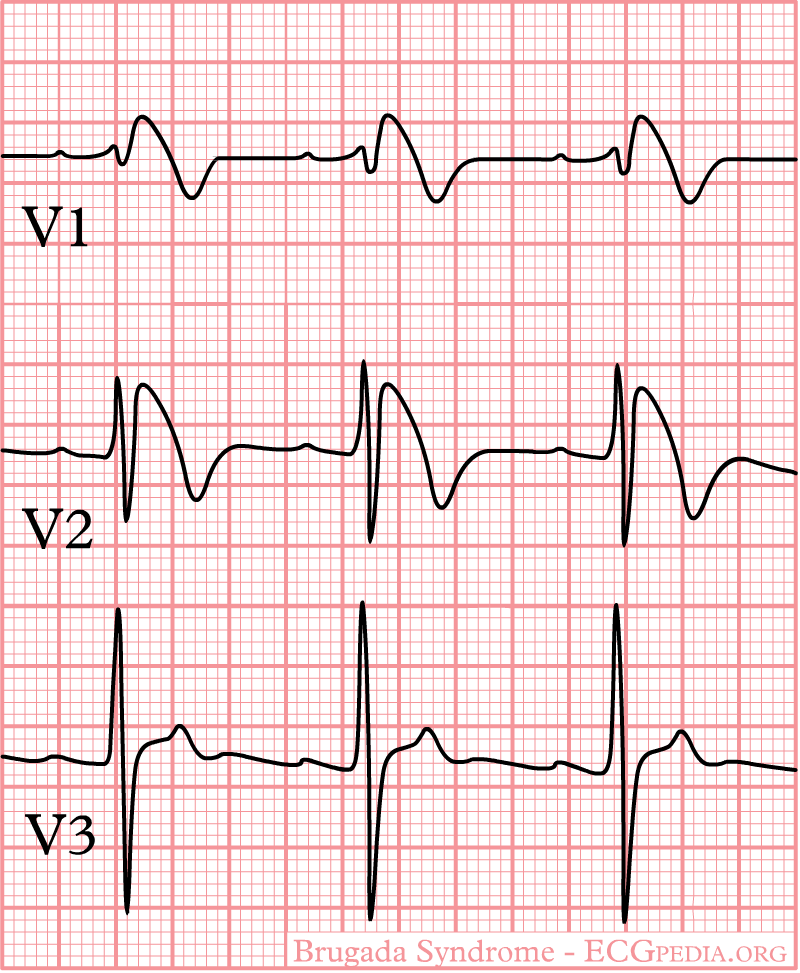
Shown below is an | Shown below is an EKG characteristic in Type I Brugada syndrome - a [[right bundle branch block]] morphology in leads V<sub>1-3</sub> and [[ST segment elevation]] in leads V<sub>1-3</sub>: | ||
[[Image:BrugadaS.jpg|center|500px]] | |||
[[ | ;For more examples of Type I Brugada syndrome, click [[Brugada syndrome electrocardiographic examples of Type I Brugada syndrome|here]] | ||
==Unmaksing Type 1 Brugada | ==Unmaksing Type 1 Brugada Pattern== | ||
The electrocardiographic findings of Type 1 Brugada syndrome are often concealed, but may be unmasked by placing the leads higher on the chest (i.e. using the "Brugada Leads") or by infusion of a | The electrocardiographic findings of Type 1 Brugada syndrome are often concealed, but may be unmasked by placing the leads higher on the chest (i.e. using the "Brugada Leads") or by infusion of a sodium channel blockers. Infusion of a sodium channel blocker may also convert a Type II or Type III Brugada pattern to a Type I Brugada pattern to establish a definitive diagnosis of the syndrome. | ||
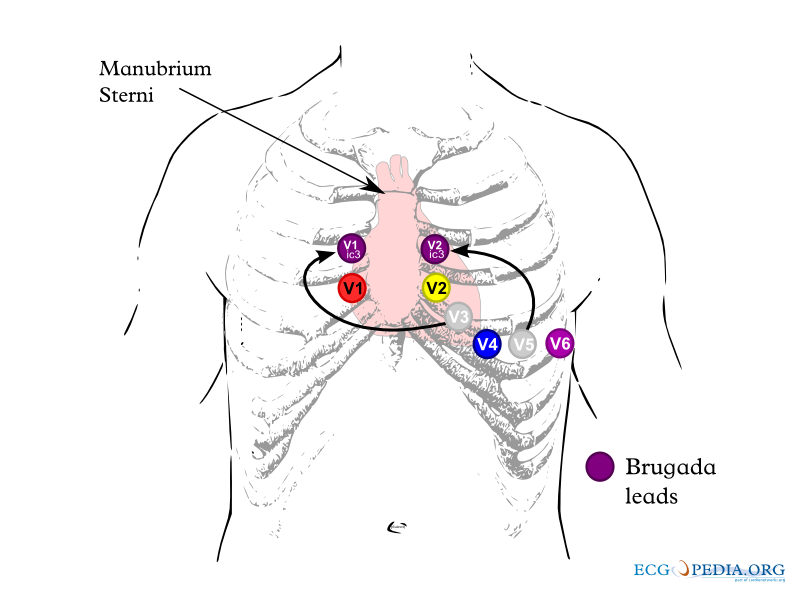
===Unmasking Brugada Syndrome by Positioning the EKG Leads Higher on the Chest Wall: The Brugada Leads=== | ===Unmasking Brugada Syndrome by Positioning the EKG Leads Higher on the Chest Wall: The Brugada Leads=== | ||
The electrocardiographic findings of Brugada syndrome can be unmasked by placing the electrocardiographic leads higher on the chest. The EKG leads should be placed on the second and third intercostal space rather than the fourth intercostal space as shown below. When the electrodes are placed in this higher position they are called Brugada leads.<ref name="pmid10809492">{{cite journal |author=Shimizu W, Matsuo K, Takagi M, Tanabe Y, Aiba T, Taguchi A, Suyama K, Kurita T, Aihara N, Kamakura S |title=Body surface distribution and response to drugs of ST segment elevation in Brugada syndrome: clinical implication of eighty-seven-lead body surface potential mapping and its application to twelve-lead electrocardiograms |journal=[[Journal of Cardiovascular Electrophysiology]] |volume=11 |issue=4 |pages=396–404 |year=2000 |month=April |pmid=10809492 |doi= |url= |issn= |accessdate=2012-10-14}}</ref><ref>''sukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J''. '' 2001; 22: 2290–2296.''</ref> | |||
[[Image:Brugada_lead_placement.jpg|center|500px]] | [[Image:Brugada_lead_placement.jpg|center|500px]] | ||
| Line 92: | Line 87: | ||
# The [[ST segment elevation]] in Type 2 increases by ≥ 2 mm | # The [[ST segment elevation]] in Type 2 increases by ≥ 2 mm | ||
# [[Premature ventricular beats]] or other arrhythmias develop | # [[Premature ventricular beats]] or other arrhythmias develop | ||
# | # The [[QRS]] widens to ≥ 130% of baseline | ||
==Type II Brugada | ====Precautions==== | ||
The infusion should be carried out in a highly monitored area equipped to perform resuscitation. In an elderly patient with prolongation of the electrocardiographic intervals, the test is best performed in the electrophysiology laboratory. Exercise caution in the presence of pre-existing conduction abnormalities, or in the presence of QRS prolongation as the infusion may cause [[complete AV block]]. Isoproteronol can be used as an antidote should this complication should occur. | |||
==Type II Brugada Pattern== | |||
The Type II Brugada pattern is not diagnostic of Brugada syndrome. The Type II Brugada pattern is characterized by a "saddleback appearance" to the ST segment. The ST segment must be elevated greater than 2 mm, and the trough of the ST segment elevation at the bottom of the saddle must be elevated > 1 mm. The Type II Brugada pattern may alternate with the Type I Brugada pattern at different times in the same patient. | The Type II Brugada pattern is not diagnostic of Brugada syndrome. The Type II Brugada pattern is characterized by a "saddleback appearance" to the ST segment. The ST segment must be elevated greater than 2 mm, and the trough of the ST segment elevation at the bottom of the saddle must be elevated > 1 mm. The Type II Brugada pattern may alternate with the Type I Brugada pattern at different times in the same patient. | ||
In order for a patient with type II Brugada pattern to be diagnosed as having Brugada syndrome, there must be a conversion of the Type II pattern to a Type I pattern with greater than 2 mm of ST segment elevation in the right precordial leads (either spontaneously or following infusion of a sodium channel blocking agent). In addition to these electrocardiographic changes, the required clinical criteria to establish the diagnosis of Brugada syndrome described above for the Type I Brugada pattern must also be present. | In order for a patient with type II Brugada pattern to be diagnosed as having Brugada syndrome, there must be a conversion of the Type II pattern to a Type I pattern with greater than 2 mm of ST segment elevation in the right precordial leads (either spontaneously or following infusion of a sodium channel blocking agent). In addition to these electrocardiographic changes, the required clinical criteria to establish the diagnosis of Brugada syndrome described above for the Type I Brugada pattern must also be present. | ||
Shown below are | Shown below are EKGs of the Type II Brugada pattern demonstrating J point elevation, and a "saddle shaped" ST segment: | ||
[[Image: | [[Image:BrugadaSyndromeType2_1.png|center|800px]] | ||
[[Image: | [[Image:BrugadaSyndromeType2.jpg|center|800px]] | ||
==Type III Brugada | ==Type III Brugada Pattern== | ||
The Type 3 Brugada pattern is associated with either a "saddleback" or a "coved" appearance but the magnitude of ST-segment elevation is <1 mm. | The Type 3 Brugada pattern is associated with either a "saddleback" or a "coved" appearance but the magnitude of ST-segment elevation is <1 mm. | ||
| Line 110: | Line 108: | ||
A sodium channel blocker infusion can be administered to convert a type III Brugada pattern to a type I Brugada pattern to facilitate the definitive diagnosis of Brugada syndrome, however the conversion of a type III Brugada pattern to a type II Brugada pattern is not considered diagnostic of the Brugada syndrome.<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> | A sodium channel blocker infusion can be administered to convert a type III Brugada pattern to a type I Brugada pattern to facilitate the definitive diagnosis of Brugada syndrome, however the conversion of a type III Brugada pattern to a type II Brugada pattern is not considered diagnostic of the Brugada syndrome.<ref name="pmid15898165">{{cite journal |author=Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A |title=Brugada syndrome: report of the second consensus conference |journal=[[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] |volume=2 |issue=4 |pages=429–40 |year=2005 |month=April |pmid=15898165 |doi= |url= |issn= |accessdate=2012-10-14}}</ref> | ||
==Sources== | |||
Copyleft images obtained courtesy of ECGpedia, http://en.ecgpedia.org/index.php?title=Special:NewFiles&offset=&limit=500 | |||
==References== | ==References== | ||
{{ | {{Reflist|2}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
[[CME Category::Cardiology]] | |||
[[Category:Electrophysiology]] | |||
[[Category:Cardiology]] | |||
[[Category:Channelopathy]] | |||
[[Category:Genetic disorders]] | |||
[[Category:Best pages]] | |||
Latest revision as of 05:46, 15 March 2016
|
Brugada syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Brugada syndrome electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Brugada syndrome electrocardiogram |
|
Risk calculators and risk factors for Brugada syndrome electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
There are three electrocardiographic patterns associated with Brugada syndrome: Type I, Type II and Type III. The diagnosis of Brugada syndrome is based upon the presence of Type I EKG changes. Patients with Type II or Type III Brugada patterns can convert to a Type I Brugada pattern following the administration of sodium channel blockers such as ajmaline and flecainide. Type 1 Brugada syndrome may always be present on the EKG, or it may be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels such as ajmaline, flecainide) or it may be unmasked by various triggers or risk factors.
Electrocardiogram
Type 1 Brugada pattern is characterized by ST elevations in leads V1-V3 with a right bundle branch block (RBBB) like pattern, although it is actually a cause of "pseudo right bundle branch block" as electrocardiographically right bundle branch block is not actually present. A prolongation of the PR interval is also frequently seen. The EKG changes of Brugada syndrome can vary over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the ST segment elevation, while vagal stimulation worsens it. The administration of class Ia, Ic and III drugs increases the ST segment elevation, as does fever. Exercise decreases ST segment elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of ST segment elevation. When the heart rate decreases, the ST segment elevation increases and when the heart rate increases the ST segment elevation decreases.
The three patterns of Brugada syndrome (Type I,II,III) are shown below:
The table below is from ECGpedia and is adapted from Wilde et al.[1]
| Type I | Type II | Type III | |
|---|---|---|---|
| J wave amplitude | >= 2mm | >= 2mm | >= 2mm |
| T wave | Negative | Positive or biphasis | Positive |
| ST-T configuration | Coved type | Saddleback | Saddleback |
| ST segment (terminal portion) | Gradually descending | Elevated >= 1mm | Elevated < 1mm |
Brugada syndrome algorithm is shown below.

Type 1 Brugada Pattern
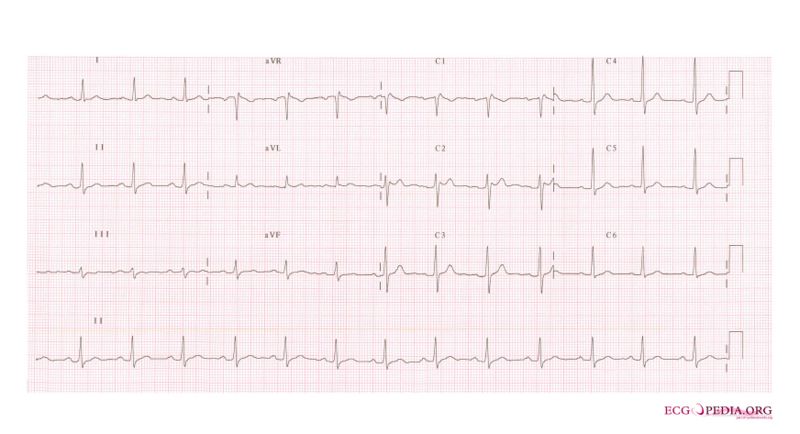
As shown by the tracing below, the EKG characteristics of Type 1 Brugada pattern include the following EKG findings in the right precordial leads (V1-V3):
- a) A broad P-wave with some PR prolongation
- b) J point elevation in the right precordial leads (V1-V3)
- c) Coved ST segment elevation
- d) An inverted T wave
Slight QT prolongation may also be observed, particularly in the right precordial leads.[2][3][4] Typically these changes are in the right precordial leads but these EKG changes can occur in the inferior [5] or left precordial leads[6]. The fact that these cases may represent atypical variants of Brugada syndrome is supported by the observation that these cases were associated with SCN5A genetic abnormalities.
Shown below is an EKG characteristic in Type I Brugada syndrome - a right bundle branch block morphology in leads V1-3 and ST segment elevation in leads V1-3:
- For more examples of Type I Brugada syndrome, click here
Unmaksing Type 1 Brugada Pattern
The electrocardiographic findings of Type 1 Brugada syndrome are often concealed, but may be unmasked by placing the leads higher on the chest (i.e. using the "Brugada Leads") or by infusion of a sodium channel blockers. Infusion of a sodium channel blocker may also convert a Type II or Type III Brugada pattern to a Type I Brugada pattern to establish a definitive diagnosis of the syndrome.
Unmasking Brugada Syndrome by Positioning the EKG Leads Higher on the Chest Wall: The Brugada Leads
The electrocardiographic findings of Brugada syndrome can be unmasked by placing the electrocardiographic leads higher on the chest. The EKG leads should be placed on the second and third intercostal space rather than the fourth intercostal space as shown below. When the electrodes are placed in this higher position they are called Brugada leads.[7][8]
Sodium Channel Blocker Challenge
Agents
Several sodium channel blockers are effective in unmasking Type 1 Brugada syndrome and in converting Type II and III Brugada syndrome to Type I to establish the diagnosis of Brugada syndrome. These agents include:
- Ajmaline 1 mg/kg/5 min IV
- Flecainide 2 mg/kg/10 min IV or 400 mg PO
- Procainamide 10 mg/kg/10 min IV
- Pilsicainide 1 mg/kg/10 min IV
When to Terminate the Sodium Channel Blocker Infusion
The sodium challenge should be terminated when:
- A diagnostic Type 1 Brugada pattern ST-segment elevation develops
- The ST segment elevation in Type 2 increases by ≥ 2 mm
- Premature ventricular beats or other arrhythmias develop
- The QRS widens to ≥ 130% of baseline
Precautions
The infusion should be carried out in a highly monitored area equipped to perform resuscitation. In an elderly patient with prolongation of the electrocardiographic intervals, the test is best performed in the electrophysiology laboratory. Exercise caution in the presence of pre-existing conduction abnormalities, or in the presence of QRS prolongation as the infusion may cause complete AV block. Isoproteronol can be used as an antidote should this complication should occur.
Type II Brugada Pattern
The Type II Brugada pattern is not diagnostic of Brugada syndrome. The Type II Brugada pattern is characterized by a "saddleback appearance" to the ST segment. The ST segment must be elevated greater than 2 mm, and the trough of the ST segment elevation at the bottom of the saddle must be elevated > 1 mm. The Type II Brugada pattern may alternate with the Type I Brugada pattern at different times in the same patient.
In order for a patient with type II Brugada pattern to be diagnosed as having Brugada syndrome, there must be a conversion of the Type II pattern to a Type I pattern with greater than 2 mm of ST segment elevation in the right precordial leads (either spontaneously or following infusion of a sodium channel blocking agent). In addition to these electrocardiographic changes, the required clinical criteria to establish the diagnosis of Brugada syndrome described above for the Type I Brugada pattern must also be present.
Shown below are EKGs of the Type II Brugada pattern demonstrating J point elevation, and a "saddle shaped" ST segment:

Type III Brugada Pattern
The Type 3 Brugada pattern is associated with either a "saddleback" or a "coved" appearance but the magnitude of ST-segment elevation is <1 mm.
In order for a patient with type II Brugada pattern to be diagnosed as having Brugada syndrome, there must be a conversion of the Type II pattern to a Type I pattern with greater than 2 mm of ST segment elevation in the right precordial leads (either spontaneously or following infusion of a sodium channel blocking agent). In addition to these electrocardiographic changes, the required clinical criteria to establish the diagnosis of Brugada syndrome described above for the Type I Brugada pattern must also be present.
A sodium channel blocker infusion can be administered to convert a type III Brugada pattern to a type I Brugada pattern to facilitate the definitive diagnosis of Brugada syndrome, however the conversion of a type III Brugada pattern to a type II Brugada pattern is not considered diagnostic of the Brugada syndrome.[9]
Sources
Copyleft images obtained courtesy of ECGpedia, http://en.ecgpedia.org/index.php?title=Special:NewFiles&offset=&limit=500
References
- ↑ Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA (2002). "Proposed diagnostic criteria for the Brugada syndrome: consensus report". Circulation. 106 (19): 2514–9. PMID 12417552. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help) - ↑ Alings M, Wilde A. “Brugada” syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999; 99: 666–673.
- ↑ Bezzina C, Veldkamp MW, van Den Berg MP, Postma AV, Rook MB, Viersma JW, Van Langen IM, Tan-Sindhunata G, Bink-Boelkens MT, van Der Hout AH, Mannens MM, Wilde AA. A single Na(+) channel mutation causing both long-QT and Brugada syndromes. Circ Res. 1999; 85: 1206–1213.
- ↑ Priori SG, Napolitano C, Gasparini M, Pappone C, Della Bella P, Brignole M, Giordano U, Giovannini T, Menozzi C, Bloise R, Crotti L, Terreni L, Schwartz PJ. Clinical and genetic heterogeneity of right bundle branch block and ST-segment elevation syndrome: a prospective evaluation of 52 families. Circulation. 2000; 102: 2509–2515.
- ↑ Kalla H, Yan GX, Marinchak R (2000). "Ventricular fibrillation in a patient with prominent J (Osborn) waves and ST segment elevation in the inferior electrocardiographic leads: a Brugada syndrome variant?". Journal of Cardiovascular Electrophysiology. 11 (1): 95–8. PMID 10695469. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ Horigome H, Shigeta O, Kuga K, Isobe T, Sakakibara Y, Yamaguchi I, Matsui A (2003). "Ventricular fibrillation during anesthesia in association with J waves in the left precordial leads in a child with coarctation of the aorta". Journal of Electrocardiology. 36 (4): 339–43. PMID 14661171. Retrieved 2012-10-14. Unknown parameter
|month=ignored (help) - ↑ Shimizu W, Matsuo K, Takagi M, Tanabe Y, Aiba T, Taguchi A, Suyama K, Kurita T, Aihara N, Kamakura S (2000). "Body surface distribution and response to drugs of ST segment elevation in Brugada syndrome: clinical implication of eighty-seven-lead body surface potential mapping and its application to twelve-lead electrocardiograms". Journal of Cardiovascular Electrophysiology. 11 (4): 396–404. PMID 10809492. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ sukhowong P, Tungsanga K. New electrocardiographic leads and the procainamide test for the detection of the Brugada sign in sudden unexplained death syndrome survivors and their relatives. Eur Heart J. 2001; 22: 2290–2296.
- ↑ Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, Gussak I, LeMarec H, Nademanee K, Perez Riera AR, Shimizu W, Schulze-Bahr E, Tan H, Wilde A (2005). "Brugada syndrome: report of the second consensus conference". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 2 (4): 429–40. PMID 15898165. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help)