Bronchiectasis CT: Difference between revisions
(→CT) |
No edit summary |
||
| Line 2: | Line 2: | ||
{{Bronchiectasis}} | {{Bronchiectasis}} | ||
{{CMG}} | {{CMG}} | ||
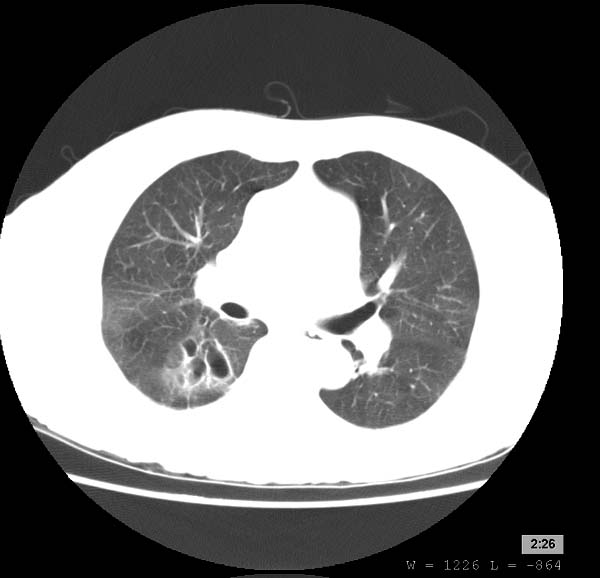
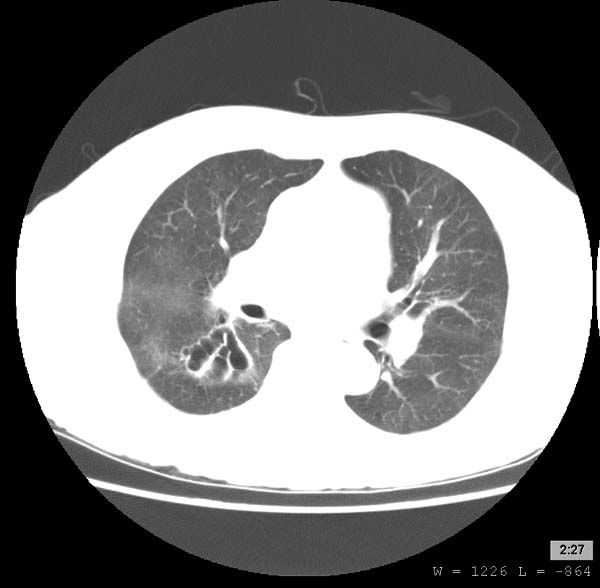
Criteria for diagnosing HRCT bronchiectasis consists of bronchial dilatation, whereby the internal diameter of a bronchus is >1.5 times (>150%) the diameter of the accompanying pulmonary artery (also known as the ‘signet ring’ pattern when the dilated airway is seen end on); and bronchial wall thickening, represented by parallel (tram) lines (Figure 1a and b). Other supporting features include failure of bronchial tapering, crowding of bronchi with lobar volume loss and thickening and plugging of small airways resulting in ‘tree-in-bud’ appearance.9 | |||
==Overview== | ==Overview== | ||
High-resolution computed tomography (HRCT) is the preferred diagnostic tool in identifying bronchiectasis. Common findings include increased diameter of a bronchus, tree-in-bud abnormalities, and cysts with definable borders. | |||
==CT== | ==Bronchiectasis CT== | ||
The diagnosis of bronchiectasis is based on the review of clinical history and characteristic patterns in | *The diagnosis of bronchiectasis is based on the review of clinical history and characteristic patterns in the HRCT findings. | ||
*The internal diameter of a bronchus is >1.5 times (>150%) the diameter of the accompanying pulmonary artery (also known as the ‘signet ring’ pattern when the dilated airway is seen end on)<ref name="pmid23728208">{{cite journal| author=McDonnell MJ, Ward C, Lordan JL, Rutherford RM| title=Non-cystic fibrosis bronchiectasis. | journal=QJM | year= 2013 | volume= 106 | issue= 8 | pages= 709-15 | pmid=23728208 | doi=10.1093/qjmed/hct109 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23728208 }} </ref> | |||
*Bronchial wall thickening (parallel tram lines0 | |||
*"Tree-in-bud" appearance | |||
:*Failure of bronchial tapering | |||
:*Crowding of bronchi with lobar volume loss | |||
:*Thickening an plugging of small airways | |||
*Cysts with definable borders | |||
*In one small study, CT findings of bronchiectasis and multiple small nodules were reported to have a [[Sensitivity_%28tests%29|sensitivity]] of 80%, [[Specificity_%28tests%29|specificity]] of 87%, and accuracy of 80% for the detection of bronchiectasis. | |||
*Bronchiectasis may also be diagnosed without CT scan confirmation if clinical history clearly demonstrates frequent, respiratory infections, as well as confirmation of an underlying problem via [[blood test|blood work]] and [[sputum]] culture samples.<ref>{{cite journal |author=Miller, JC |title=Pulmonary Mycobacterium Avium-Intracellular Infections in Women |language=English |journal=Radiology Rounds |volume=4 |issue=2 |pages= |year=2006 |pmid= |doi=}}</ref> | |||
'''Patient #1''' | '''Patient #1''' | ||
Revision as of 13:31, 24 June 2015
|
Bronchiectasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bronchiectasis CT On the Web |
|
American Roentgen Ray Society Images of Bronchiectasis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Criteria for diagnosing HRCT bronchiectasis consists of bronchial dilatation, whereby the internal diameter of a bronchus is >1.5 times (>150%) the diameter of the accompanying pulmonary artery (also known as the ‘signet ring’ pattern when the dilated airway is seen end on); and bronchial wall thickening, represented by parallel (tram) lines (Figure 1a and b). Other supporting features include failure of bronchial tapering, crowding of bronchi with lobar volume loss and thickening and plugging of small airways resulting in ‘tree-in-bud’ appearance.9
Overview
High-resolution computed tomography (HRCT) is the preferred diagnostic tool in identifying bronchiectasis. Common findings include increased diameter of a bronchus, tree-in-bud abnormalities, and cysts with definable borders.
Bronchiectasis CT
- The diagnosis of bronchiectasis is based on the review of clinical history and characteristic patterns in the HRCT findings.
- The internal diameter of a bronchus is >1.5 times (>150%) the diameter of the accompanying pulmonary artery (also known as the ‘signet ring’ pattern when the dilated airway is seen end on)[1]
- Bronchial wall thickening (parallel tram lines0
- "Tree-in-bud" appearance
- Failure of bronchial tapering
- Crowding of bronchi with lobar volume loss
- Thickening an plugging of small airways
- Cysts with definable borders
- In one small study, CT findings of bronchiectasis and multiple small nodules were reported to have a sensitivity of 80%, specificity of 87%, and accuracy of 80% for the detection of bronchiectasis.
- Bronchiectasis may also be diagnosed without CT scan confirmation if clinical history clearly demonstrates frequent, respiratory infections, as well as confirmation of an underlying problem via blood work and sputum culture samples.[2]
Patient #1
Patient #2
References
- ↑ McDonnell MJ, Ward C, Lordan JL, Rutherford RM (2013). "Non-cystic fibrosis bronchiectasis". QJM. 106 (8): 709–15. doi:10.1093/qjmed/hct109. PMID 23728208.
- ↑ Miller, JC (2006). "Pulmonary Mycobacterium Avium-Intracellular Infections in Women". Radiology Rounds. 4 (2).