Breast cancer classification
|
Breast Cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Breast cancer classification On the Web |
|
American Roentgen Ray Society Images of Breast cancer classification |
|
Risk calculators and risk factors for Breast cancer classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Assistant Editor(s)-In-Chief: Jack Khouri
Overview
Breast cancer classification divides all forms of breast cancer according to four different schemes, each based on different criteria and serving a different purpose. The four approaches consider pathology, the grade of the tumor, expression of proteins and genes, and the stage of the tumor.
Classifications of breast cancer are usually, but not always, classified by the histological appearance of tissue in the tumor. Rare variants are defined on the basis of physical exam findings. For example, Inflammatory breast cancer (IBC), a form of ductal carcinoma or malignant cancer in the ducts, is distinguished from other carcinomas by the inflamed appearance of the affected breast.[1] In the future, some pathologic classifications may be changed. For example, a subset of ductal carcinomas may be re-named basal-like carcinoma (part of the "triple-negative" tumors).
Major schemes
- Pathology - A pathologist will categorize each tumor based on its histological (microscopic anatomy) appearance and other criteria. The most common pathologic types of breast cancer are invasive ductal carcinoma, malignant cancer in the breast's ducts, and invasive lobular carcinoma, malignant cancer in the breast's lobules.
- Grade of tumor - The histological grade of a tumor is determined by a pathologist under a microscope. A well-differentiated (low grade) tumor resembles normal tissue. A poorly differentiated (high grade) tumor is composed of disorganized cells and, therefore, does not look like normal tissue. Moderately differentiated (intermediate grade) tumors are somewhere in between.
- Protein & gene expression status - Currently, all breast cancers should be tested for expression, or detectable effect, of the estrogen receptor (ER), progesterone receptor (PR) and HER2/neu proteins. These tests are usually done by immunohistochemistry and are presented in a pathologist's report. The profile of expression of a given tumor helps predict its prognosis, or outlook, and helps an oncologist choose the most appropriate treatment. More genes and/or proteins may be tested in the future (eg PAX2[2]).
- Stage of a tumor - The currently accepted staging scheme for breast cancer is the TNM classification.
Staging
Tumor - There are five tumor classification values (Tis, T1, T2, T3 or T4) which depend on the presence or absence of invasive cancer, the dimensions of the invasive cancer, and the presence or absence of invasion outside of the breast (e.g. to the skin of the breast, to the muscle or to the rib cage underneath):
- Tx - Primary tumor cannot be assessed.
- T0 - No evidence of primary tumor.
- Tis - Carcinoma in situ.
- Tis(DCIS) - Intraductal Carcinoma in situ.
- Tis(LCIS) - Lobular Carcinoma in situ.
- Tis(Paget's) - Paget's disease of the nipple with no tumor.
- T1 - Tumor 2cm or less in its greatest dimension.
- T1mic - Microinvasion 0.1cm or less in greatest dimension.
- T1a - Tumor more than 0.1cm but not more than 0.5cm in its greatest dimension.
- T1b - Tumor more than 0.5cm but not more than 1.0cm in its greatest dimension.
- T1c - Tumor more than 1.0cm but not more than 2.0cm in its greatest dimension.
- T2 - Tumor more than 2.0cm but not more than 5.0cm in its greatest dimension.
- T3 - Tumor more than 5cm in its greatest dimension.
- T4 - Tumor of any size with direct extension to (a) chest wall or (b) skin as described below:
- T4a - Extension to chest wall.
- T4b - Edema (including peau d'orange) or ulceration of the breast skin, or satellite skin nodules confined to the same breast.
- T4c - Both T4a and T4b.
- T4d - Inflammatory breast cancer.
Lymph Node - There are four lymph node classification values (N0, N1, N2 or N3) which depend on the number, size and location of breast cancer cell deposits in lymph nodes.
- Nx - regional lymph nodes cannot be assessed. Perhaps due to previous removal.
- N0 - no regional lymph node metastasis.
- N1 - metastasis to movable regional axillary lymph nodes on the same side as the affected breast.
- N2 - metastasis to fixed regional axillary lymph nodes, or metastasis to the internal mammary lymph nodes, on the same side as the affected breast.
- N3 - metastasis to supraclavicular lymph nodes or infraclavicular lymph nodes or metastasis to the internal mammary lymph nodes with metastasis to the axillary lymph nodes.
Metastases - There are two metastatic classification values (M0 or M1) which depend on the presence or absence of breast cancer cells in locations other than the breast and lymph nodes (so-called distant metastases, e.g. to bone, brain, lung).
Pathologic types
Note: The following table includes benign tumours (non cancers) as well as malignant tumours (cancers)
The latest (2003) World Health Organization (WHO) classification of tumors of the breast[3] recommends the following pathological types:
Invasive breast carcinomas
- Invasive ductal carcinoma
- Most are "not otherwise specified"
- The remainder are given subtypes:
- Mixed type carcinoma
- Pleomorphic carcinoma
- Carcinoma with osteoclastic giant cells
- Carcinoma with choriocarcinomatous features
- Carcinoma with melanotic features
- Invasive lobular carcinoma
- Tubular carcinoma
- Invasive cribriform carcinoma
- Medullary carcinoma
- Mucinous carcinoma and other tumours with abundant mucin
- Mucinous carcinoma
- Cystadenocarcinoma and columnar cell mucinous carcinoma
- Signet ring cell carcinoma
- Neuroendocrine tumours
- Solid neuroendocrine carcinoma (carcinoid of the breast)
- Atypical carcinoid tumour
- Small cell / oat cell carcinoma
- Large cell neuroendocrine carcioma
- Invasive papillary carcinoma
- Invasive micropapillary carcinoma
- Apocrine carcinoma
- Metaplastic carcinomas
- Pure epithelial metaplastic carciomas
- Squamous cell carcinoma
- Adenocarcinoma with spindle cell metaplasia
- Adenosquamous carcinoma
- Mucoepidermoid carcinoma
- Mixed epithelial/mesenchymal metaplastic carcinomas
- Pure epithelial metaplastic carciomas
- Lipid-rich carcinoma
- Secretory carcinoma
- Oncocytic carcinoma
- Adenoid cystic carcinoma
- Acinic cell carcinoma
- Glycogen-rich clear cell carcinoma
- Sebaceous carcinoma
- Inflammatory carcinoma
- Bilateral breast carcinoma
Mesenchymal tumors (including sarcoma)
- Haemangioma
- Angiomatosis
- Haemangiopericytoma
- Pseudoangiomatous stromal hyperplasia
- Myofibroblastoma
- Fibromatosis (aggressive)
- Inflammatory myofibroblastic tumour
- Lipoma
- Angiolipoma
- Granular cell tumour
- Neurofibroma
- Schwannoma
- Angiosarcoma
- Liposarcoma
- Rhabdomyosarcoma
- Osteosarcoma
- Leiomyoma
- Leiomysarcoma
Precursor lesions
- Lobular neoplasia
- lobular carcinoma in situ
- Intraductal proliferative lesions
- Usual ductal hyperplasia
- Flat epithelial hyperplasia
- Atypical ductal hyperplasia
- Ductal carcinoma in situ
- Microinvasive carcinoma
- Intraductal papillary neoplasms
- Central papilloma
- Peripheral papilloma
- Atypical papilloma
- Intraductal papillary carcinoma
- Intracystic papillary carcinoma
Benign epithelial lesions
- Adenosis, including variants
- Sclerosing adenosis
- Apocrine adenosis
- Blunt duct adenosis
- Microglandular adenosis
- Adenomyoepithelial adenosis
- Radial scar / complex sclerosing lesion
- Adenomas
- Tubular adenoma
- Lactating adenoma
- Apocrine adenoma
- Pleomorphic adenoma
- Ductal adenoma
Myoepithelial lesions
- Myoepitheliosis
- Adenomyoepithelial adenosis
- Adenomyoepithelioma
- Malignant myoepithelioma
Fibroepithelial tumours
- Fibroadenoma
- Phyllodes tumour
- Benign
- Borderline
- Malignant
- Periductal stromal sarcoma, low grade
- Mammary hamartoma
Tumours of the nipple
- Nipple adenoma
- Syringomatous adenoma
- Paget's disease of the nipple
Malignant lymphoma
Metastatic tumours
Tumours of the male breast
- Gynecomastia
- Carcinoma
- In situ
- Invasive
Gallery
-
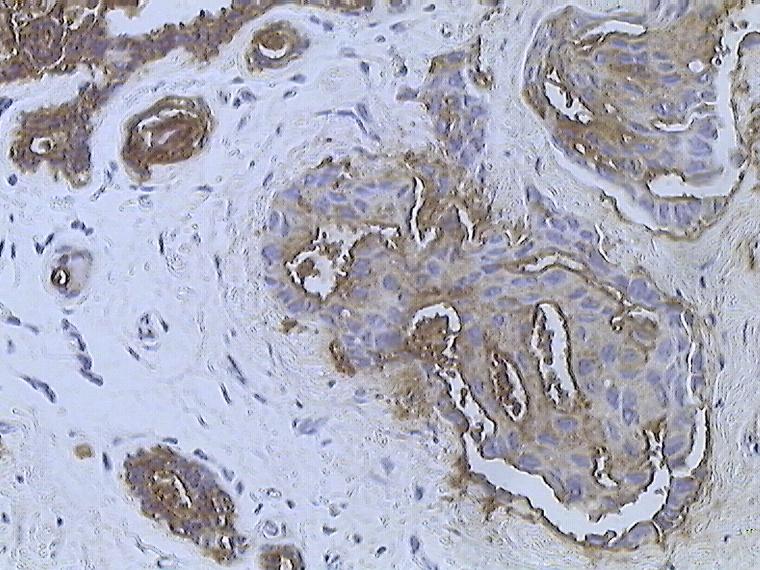
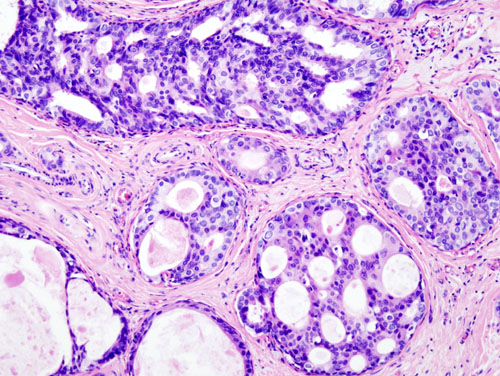
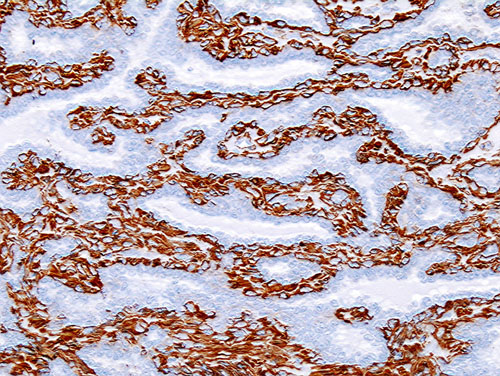
Infiltrating ductal carcinoma of the Breast assayed with anti Mucin 1 antibody
-
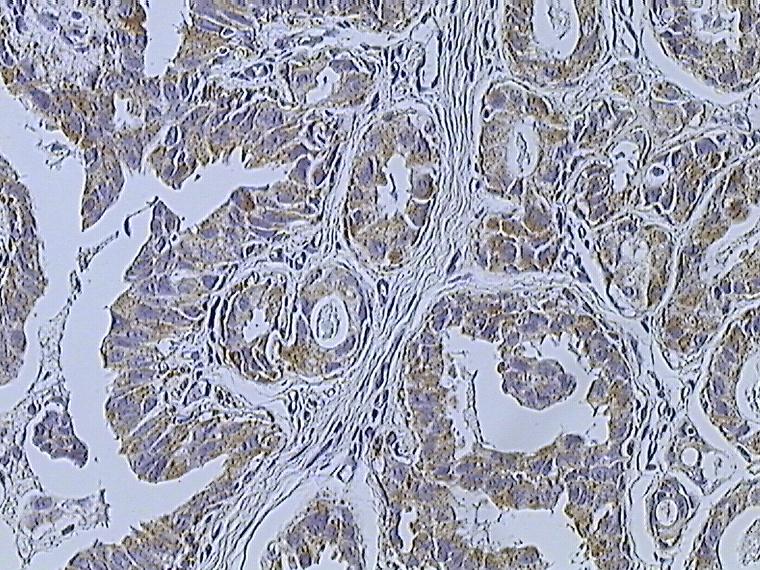
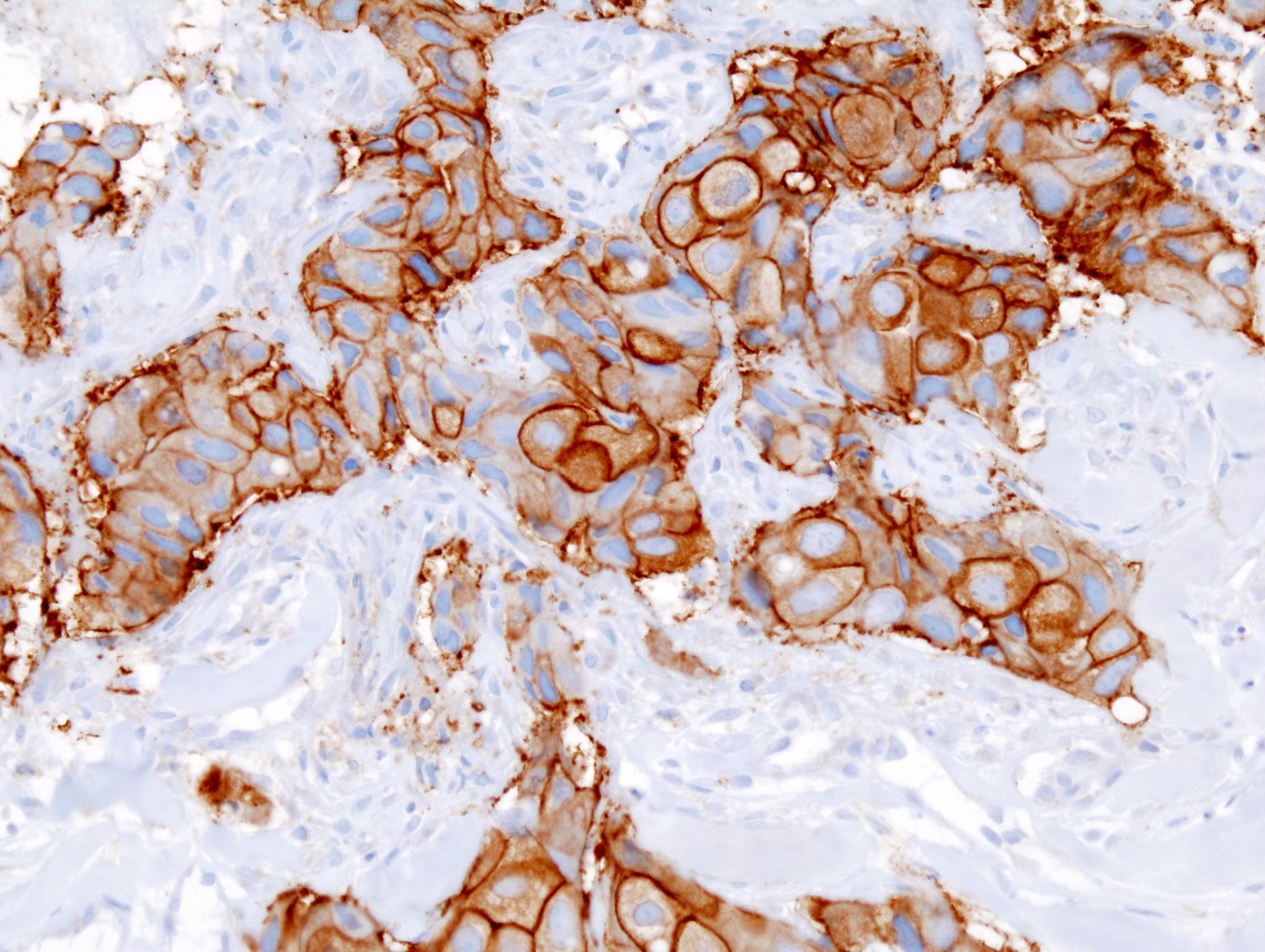
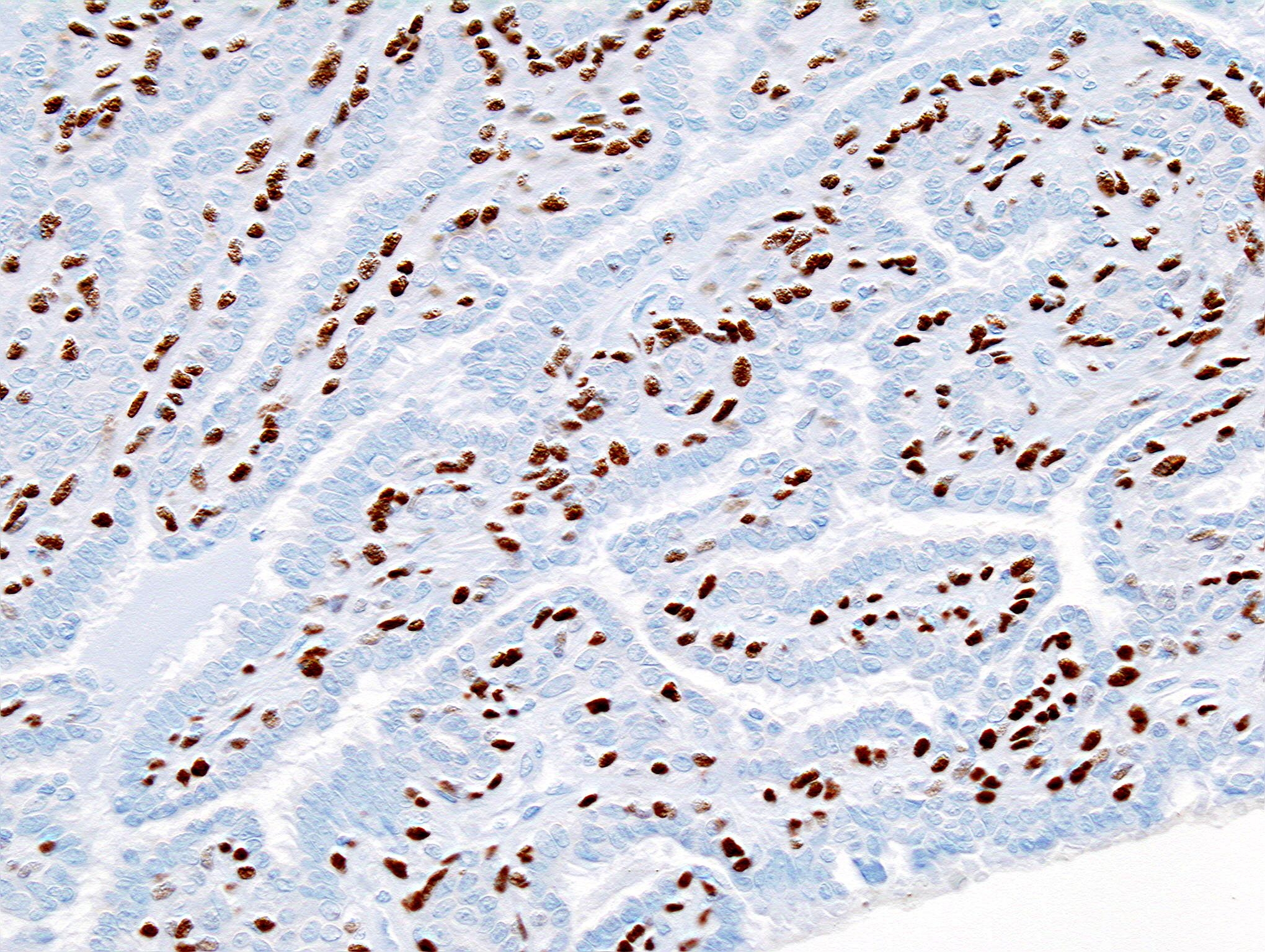
Breast cancer (Infiltrating ductal carcinoma of the breast) assayed with anti HER-2 (ErbB2) antibody
-
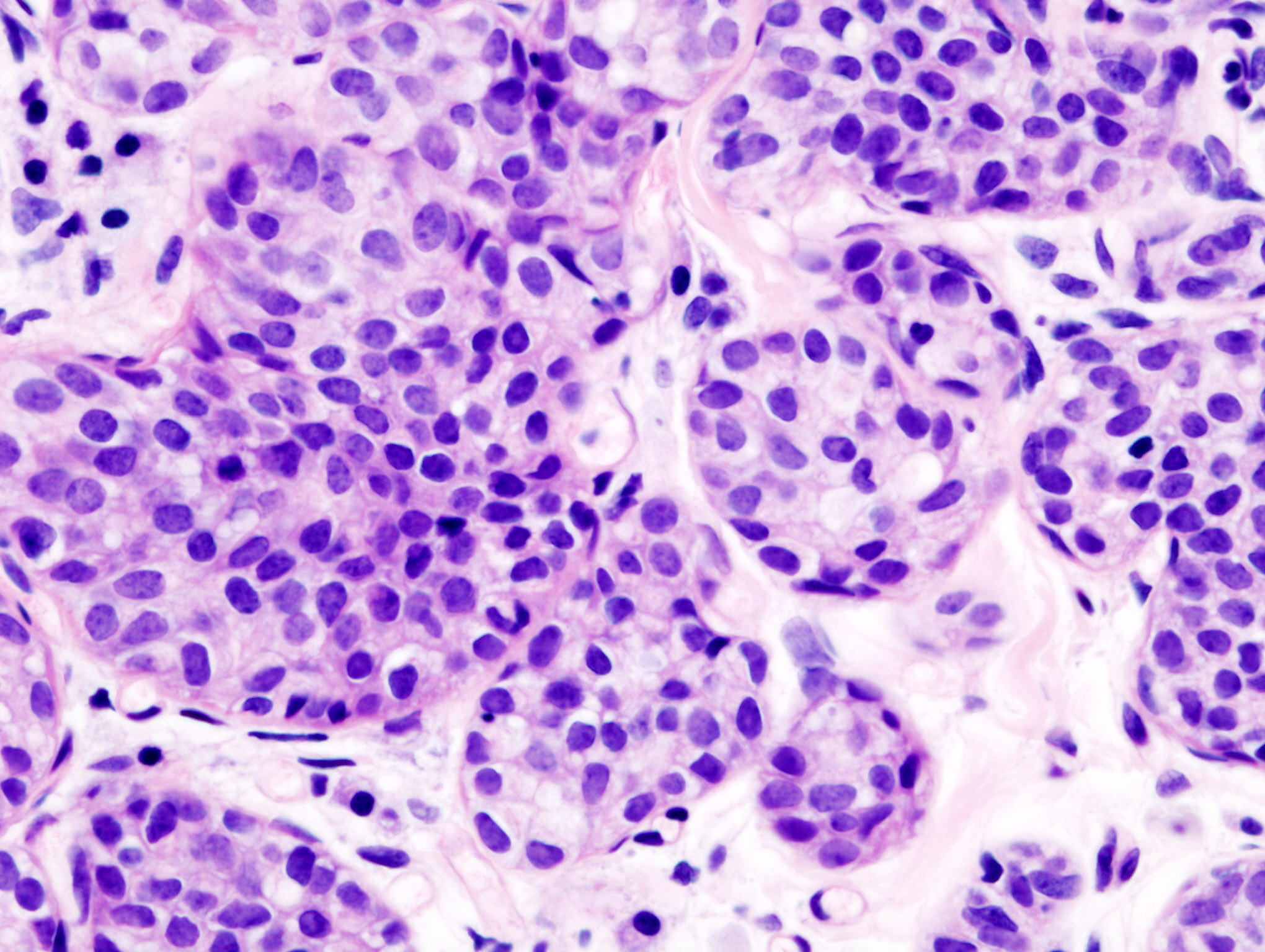
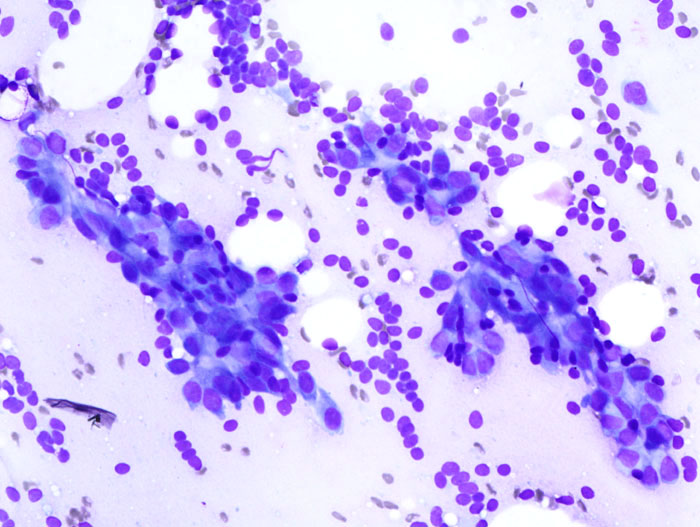
Invasive lobular carcinoma of the breast demonstrating a predominantly lobular growth pattern
-
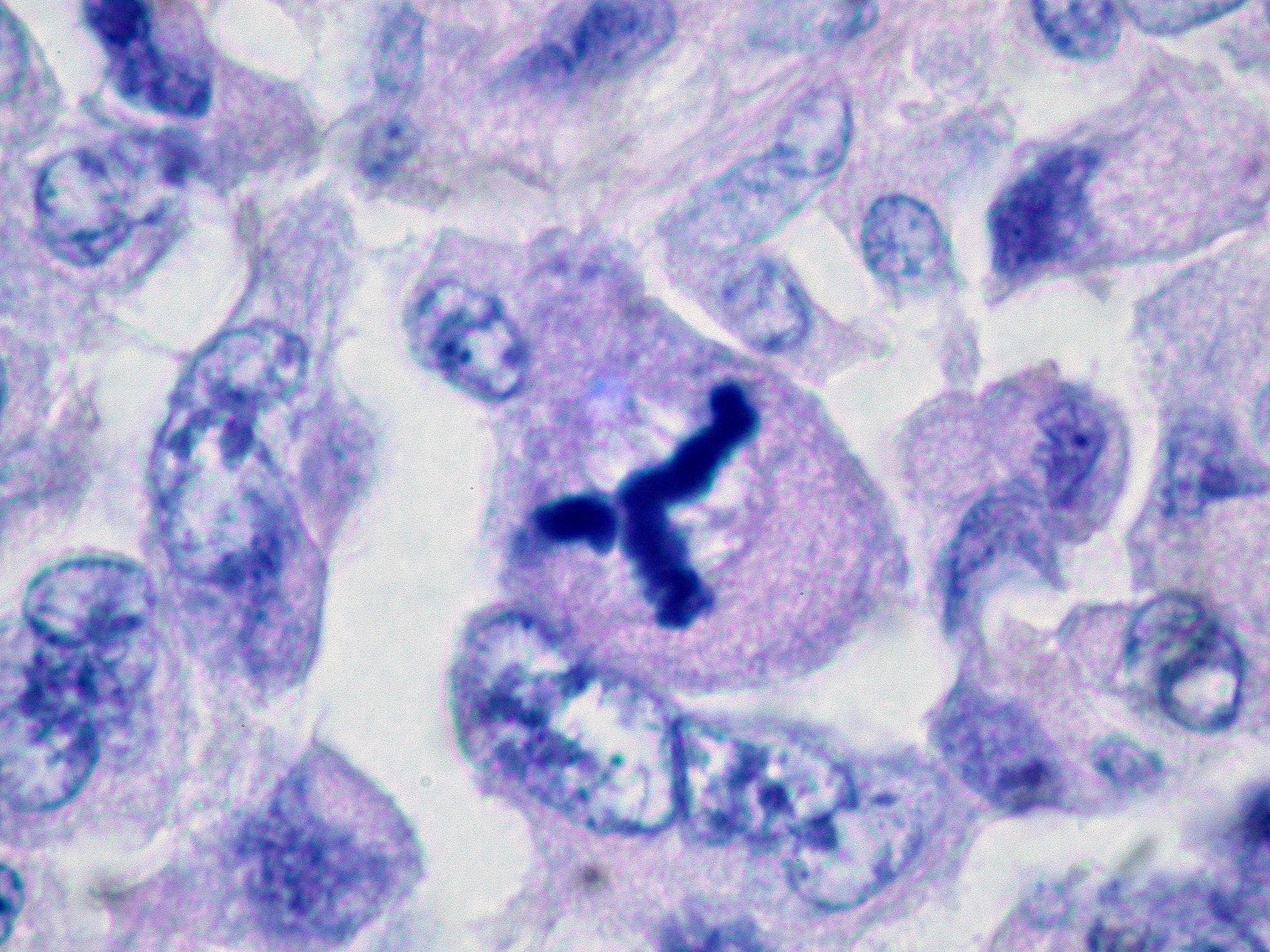
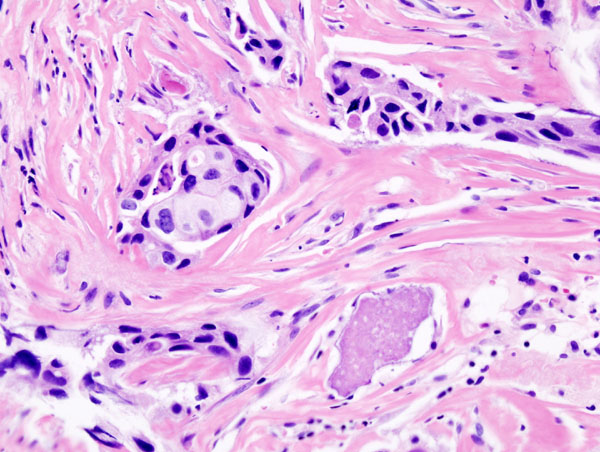
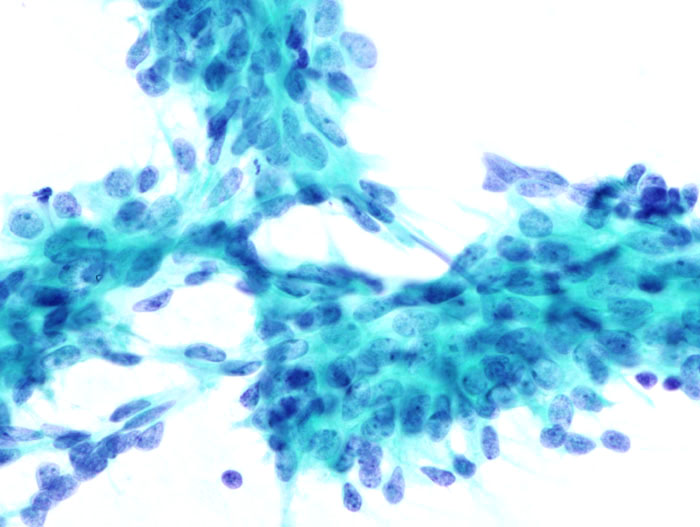
Metaplastic (sarcomatoid) carcinoma of the breast.
-
Histopathologic image from ductal cell carcinoma in situ (DCIS) of breast. Hematoxylin-eosin stain.
-
Histopathology of invasive ductal carcinoma of the breast representing a scirrhous growth. Core needle biopsy. Hematoxylin and eosin stain.
-
Histopathology of invasive ductal carcinoma of the breast representing a scirrhous growth. Core needle biopsy. HER-2/neu oncoprotein expression by Ventana immunostaining system.
-
Breast cancer (Infiltrating ductal carcinoma of the breast) dyed with H&E
-
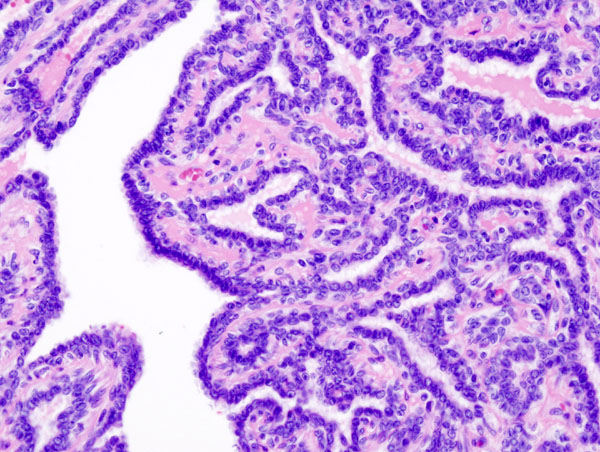
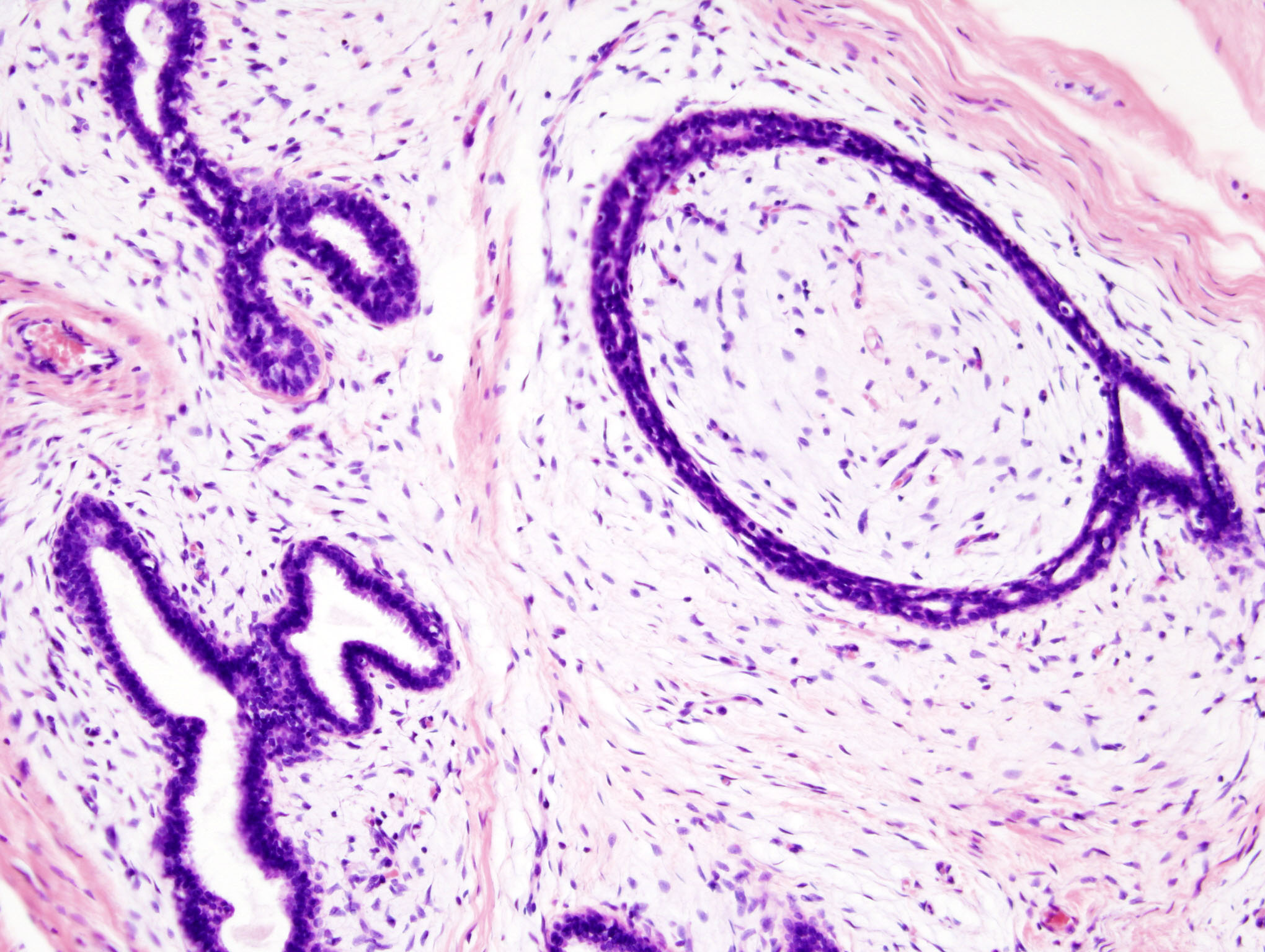
Histopathology of intraductal papilloma of the breast by excisional biopsy. Hematoxylin and eosin stain.
-
Histopathology of intraductal papilloma of the breast by excisional biopsy. Immunostaining for alpha-smooth muscle actin.
-
Histopathology of intraductal papilloma of the breast by excisional biopsy. Immunostaining for p63 protein.
-
Breast fibroadenoma
-
Breast fibroadenoma
-
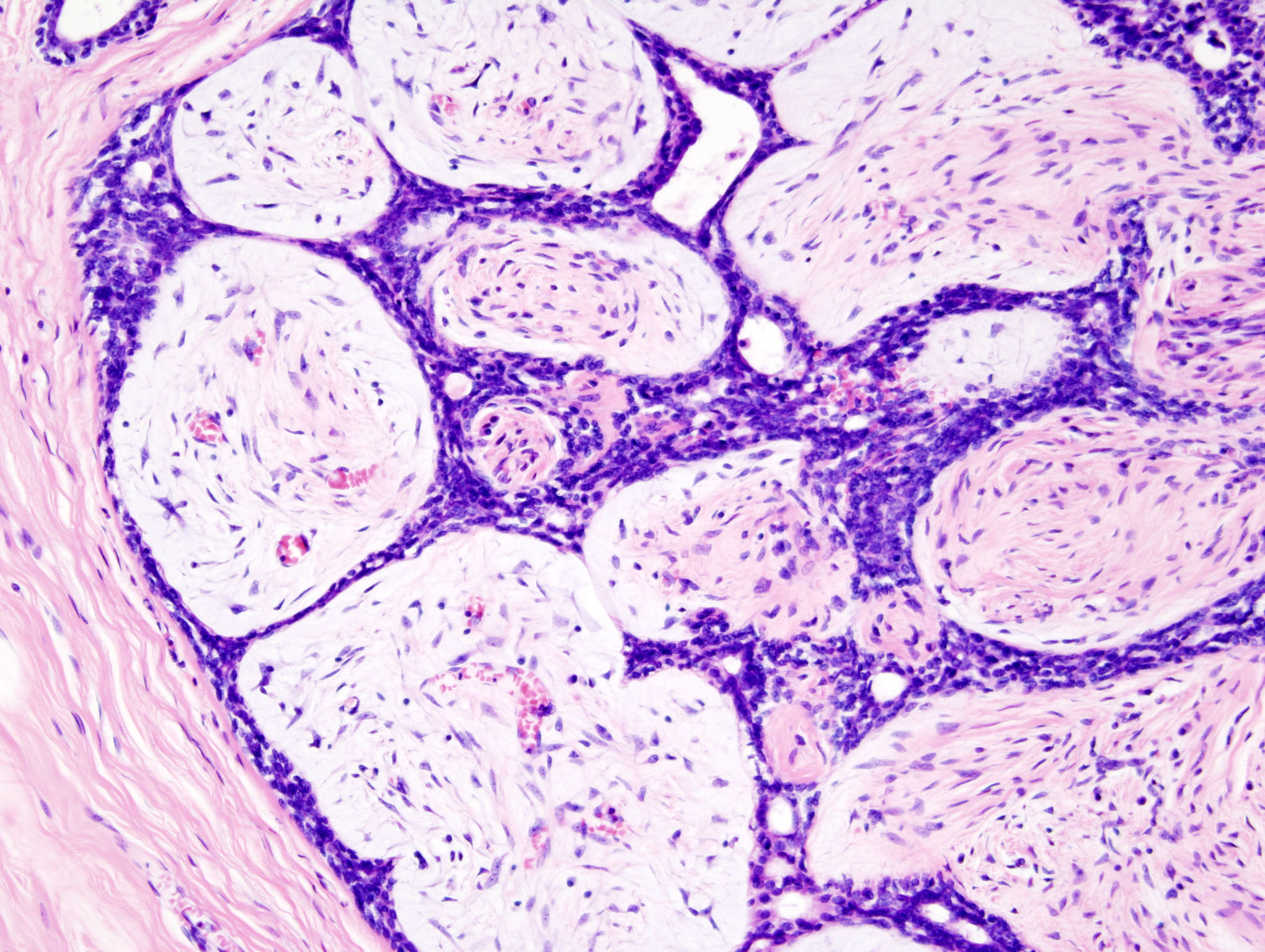
Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain.
-
Histopathologic image of breast fibroadenoma. Core needle biopsy. Hematoxylin & eosin stain.
References
- ↑ Giordano SH, Hortobagyi GN (2003). "Inflammatory breast cancer: clinical progress and the main problems that must be addressed". Breast Cancer Res. 5 (6): 284–8. doi:10.1186/bcr608. PMID 14580242. Free Full Text.
- ↑ http://cordis.europa.eu/fetch?CALLER=EN_NEWS&ACTION=D&SESSION=&RCN=30093
- ↑ Tumours of the breast and female genital organs, WHO classification of tumours, 2003, ISBN 9283224124