Bile duct cyst
For patient information click here
| Bile duct cyst | |
 | |
|---|---|
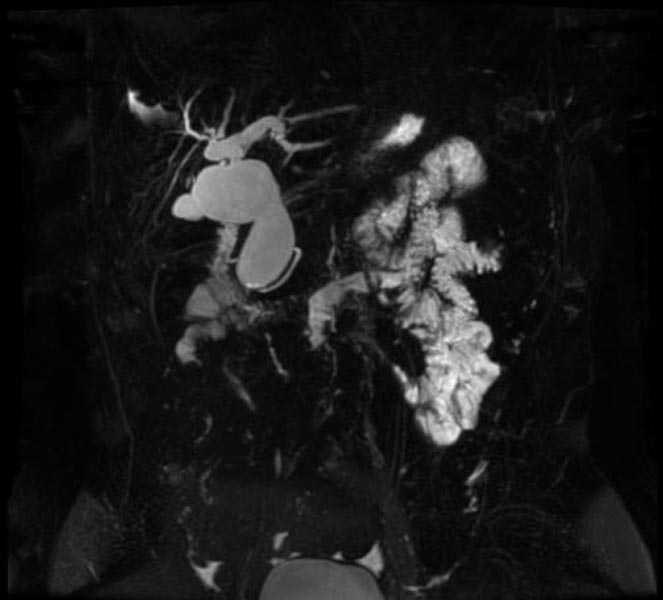
| MRCP: Type 4 bile duct cyst. Image courtesy of RadsWiki |
|
Bile duct cyst Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Bile duct cyst On the Web |
|
American Roentgen Ray Society Images of Bile duct cyst |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: Choledochal cysts
Overview
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Bile Duct Cyst from other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications and Prognosis
Diagnosis
History, and Symptoms | Physical Examination |
Laboratory Findings
The laboratory tests are not specific and may show slightly abnormal liver function and cholestasis tests (serum bilirubin, alanine aminotransferase, aspartate aminotransferase, alkaline phosphatase, γ-glutamyltranspeptidase) and amylase values.[1][2]
| X Ray |
CT |
CT scan of the abdominal cavity shows the relationship of the cyst with surrounding tissues, its continuity with the biliary tree, and the existence and staging of any accompanying malignancy. It is helpful to explain the intrahepatic dilations and the severity of the disease in people with Caroli’s disease (diffuse hepatic or localized segmental involvement) and type IVA cysts. Before doing an operation, a surgeon must consider certain factors since segmental lobectomy is a treatment option for localized type-IVA BC or Caroli's disease.
Though MRCP is superior to CTC cholangiography (Computerized tomography cholangiography (CTC) following infusion of meglumine iodoxamate), in the visualization of the intrahepatic duct and the pancreatic system according to research by Fumino et al., The greatest benefit of CTC, however, is its capacity to generate clear pictures free of respiratory aberrations in infants, in whom conducting an accurate MRCP is particularly challenging.[1][3]
MRI |
Echocardiography or Ultrasound |
Treatment
Medical Therapy | Surgery | Primary Prevention | Secondary Prevention | Cost-Effectiveness of Therapy | Future or Investigational Therapies
Case Studies
- ↑ 1.0 1.1 Singham J, Yoshida EM, Scudamore CH (December 2009). "Choledochal cysts: part 2 of 3: Diagnosis". Can J Surg. 52 (6): 506–11. PMC 2792398. PMID 20011188.
- ↑ Kim OH, Chung HJ, Choi BG (January 1995). "Imaging of the choledochal cyst". Radiographics. 15 (1): 69–88. doi:10.1148/radiographics.15.1.7899614. PMID 7899614.
- ↑ Fumino S, Ono S, Kimura O, Deguchi E, Iwai N (July 2011). "Diagnostic impact of computed tomography cholangiography and magnetic resonance cholangiopancreatography on pancreaticobiliary maljunction". J Pediatr Surg. 46 (7): 1373–8. doi:10.1016/j.jpedsurg.2011.01.026. PMID 21763837.