|
|
| Line 1: |
Line 1: |
| | __NOTOC__ |
| | '''For patient information click [[{{PAGENAME}} (patient information)|here]]''' |
| | |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = {{PAGENAME}} | | | Name = {{PAGENAME}} | |
| Line 13: |
Line 16: |
| MeshID = | | | MeshID = | |
| }} | | }} |
| {{SI}}
| |
| {{CMG}} '''Associate Editor(s)-In-Chief:''' {{CZ}}
| |
|
| |
|
| |
|
| |
| '''Synonyms and Related Keywords''': Choledochal cysts
| |
|
| |
| ==Overview==
| |
|
| |
| '''Bile duct cysts''' are [[congenital]] conditions associated with [[benign]] [[cyst]]ic dilatation of [[bile ducts]]. They are uncommon in western countries<ref name="pmid17825168">{{cite journal |author=Liu YB, Wang JW, Devkota KR, ''et al'' |title=Congenital choledochal cysts in adults: twenty-five-year experience |journal=Chin. Med. J. |volume=120 |issue=16 |pages=1404–7 |year=2007 |pmid=17825168 |doi=}}</ref> <ref>Yu, Jinxing, Turner, Mary Ann, Fulcher, Ann S., Halvorsen, Robert A. [http://www.ajronline.org/cgi/content/abstract/187/6/1536 Congenital Anomalies and Normal Variants of the Pancreaticobiliary Tract and the Pancreas in Adults: Part 1, Biliary Tract.] Am. J. Roentgenol. 2006 187: 1536-1543</ref> but not as rare in East Asian nations like Japan and China.
| |
|
| |
| ==Historical Perspective==
| |
|
| |
| Vachel and Stevens were the first to describe a case of cystic dilatation of the intrahepatic bile ducts in 1906, but Jacques Caroli in 1958 gave a more thorough description of a syndrome of '''congenital malformation of the intrahepatic ducts''' with segmental '''cystic dilatation''', increased '''biliary lithiasis''', '''cholangitis''' and '''liver abscesses''', associated with '''renal''' cystic disease or tubular ectasia. The disease is uncommon, with about 180 cases reported in the literature.
| |
| ==Classification==
| |
|
| |
| According to the '''Todani system''', there are five types of bile duct cysts.<ref>{{cite journal |author=Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K |title=Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst |journal=Am. J. Surg. |volume=134 |issue=2 |pages=263-9 |year=1977 |pmid=889044}}</ref>. This classification was based on site of the cyst or dilatation. Type I to IV has been subtyped.
| |
|
| |
| [[Image:Choledochal_cysts.png|thumb|400px|left|Different types of bile duct cysts]]
| |
| <br clear="left"/>
| |
| ===Type 1: [[Choledochal cysts|Choledochal Cyst]]===
| |
|
| |
| Choledochal cysts are cystic dilatation of the common bile duct (CBD). Most common variety involving saccular or fusiform dilatation of a portion or entire [[common bile duct]] (CBD) with normal intrahepatic duct.
| |
|
| |
| * Account for 80% to 90% of all bile duct cysts
| |
| * Often presents during infancy with significant liver disease.
| |
| * Characterized by fusiform dilation of the extrahepatic bile duct
| |
| * Theorized that choledochal cysts form as the result of reflux of pancreatic secretions into the bile duct via [[anomalous pancreaticobiliary junction]].
| |
| * Cyst should be resected completely to prevent associated complications (i.e. [[ascending cholangitis]] and malignant transformation).
| |
|
| |
| ===Type 2: Diverticulum===
| |
|
| |
| Isolated diverticulum protruding from the CBD.
| |
|
| |
| * Accounts for 3% of all bile duct cysts
| |
| * Represents a true diverticulum.
| |
| * Saccular outpouchings arising from the supraduodenal extrahepatic bile duct or the [[intrahepatic bile ducts]].
| |
|
| |
|
| ===Type 3: Choledochocele<sup><small>[http://home.flash.net/~drrad/tf/112999.htm]</small></sup>===
| | {{Bile duct cyst}} |
| | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
| | {{SK}} Choledochal cysts |
|
| |
|
| Arise from dilatation of duodenal portion of CBD or where pancreatic duct meets.
| | ==[[Bile duct cyst overview|Overview]]== |
|
| |
|
| * Accounts for 5% of all bile duct cysts
| | ==[[Bile duct cyst historical perspective|Historical Perspective]]== |
| * Represents protrusion of a focally dilated, intramural segment of the distal common [[bile duct]] into the [[duodenum]].
| |
| * Choledochoceles may be successfully managed with endoscopic sphincterotomy, surgical excision, or both, in symptomatic patients.
| |
| * Often present with pain and obstructive jaundice; many have pancreatitis.
| |
|
| |
|
| ===Type 4: Multiple Communicating Intra and Extrahepatic Duct Cysts=== | | ==[[Bile duct cyst classification|Classification]]== |
|
| |
|
| Dilatation of both intrahepatic and extrahepatic biliary duct.
| | ==[[Bile duct cyst pathophysiology|Pathophysiology]]== |
|
| |
|
| * Second most common type of bile duct cysts (10%)
| | ==[[Bile duct cyst causes|Causes]]== |
| * Subdivided into subtypes A and B.
| |
| ** Type 4A: Fusiform dilation of the entire extrahepatic bile duct with extension of dilation of the intrahepatic bile ducts
| |
| ** Type 4B: Multiple cystic dilations involving only the extrahepatic bile duct.
| |
|
| |
|
| [http://www.radswiki.net Images courtesy of RadsWiki] | | ==[[Bile duct cyst differential diagnosis|Differentiating Bile duct cyst from other Diseases]]== |
|
| |
|
| <gallery>
| | ==[[Bile duct cyst epidemiology and demographics|Epidemiology and Demographics]]== |
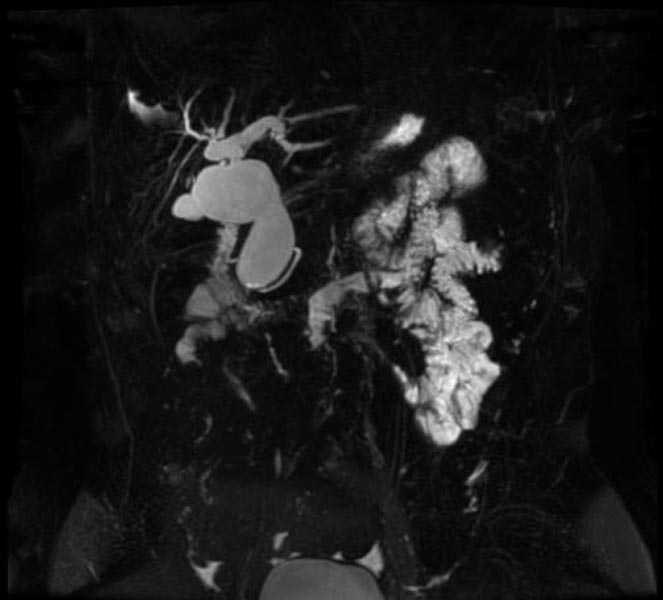
| Image:Bile duct cyst 001.jpg|MRI - T2: Type 4 bile duct cyst
| |
| Image:Bile duct cyst 002.jpg|MRI - T2: Type 4 bile duct cyst
| |
| Image:Bile duct cyst 003.jpg|MRI - T2: Type 4 bile duct cyst
| |
| Image:Bile duct cyst 004.jpg|MRCP: Type 4 bile duct cyst
| |
| </gallery>
| |
|
| |
|
| === Type 5: Caroli's Disease=== | | ==[[Bile duct cyst natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| Cystic dilatation of intra hepatic biliary ducts. <ref>Caroli, J, et al. La dilatation polykystique congenitale des voies biliaires intrahepatiques. Essai del classification. Sem Hop Paris 1958;34:488</ref> <ref>Lu, S.C. et al. Diseases of the biliary tree. Textbook of Gastroenterology 1995:2212.</ref> <ref>Tandon, RK, et al. Caroli’s disease: A heterogeneous entity. Amer J Gastroent 1990;85:170. PMID 2301339</ref> <ref>Chalasani, N, et al. Spontaneous rupture of a bile duct. Amer J Gastroent 1997;92:1062. PMID 9177539</ref> <ref>Miller, WJ, et al. Imaging findings in Caroli’s disease. Am J Roenth 1995;165:333. PMID 7618550</ref> <ref>Torra, R, et al. Autosomal dominant polycystic kidney disease and Caroli’s disease. Kidney Int 1997;52:33. PMID 9211343</ref> <ref>Ros, E, et al. Ursodeoxycholic acid treatment of primary hepatolithiasis in Caroli’s syndrome. Lancet 1993;342:404. PMID 8101905</ref>
| |
|
| |
| * [[Caroli's disease]] is a rare form of congenital biliary cystic disease manifested by cystic dilations of intrahepatic bile ducts
| |
| * Association with benign renal tubular ectasia and other forms of renal cystic disease.
| |
|
| |
| ==Pathophysiology==
| |
| ===Bile Duct Anatomy===
| |
| The path is as follows: [[Bile canaliculi]] '''→''' [[Canals of Hering]] '''→''' [[interlobular bile ducts]] '''→''' [[intrahepatic bile ducts]] '''→''' left and right [[hepatic ducts]] ''merge to form'' '''→''' [[common hepatic duct]] ''exits liver and joins'' '''→''' [[cystic duct]] (from [[gall bladder]]) ''forming'' '''→''' [[common bile duct]] '''→''' ''joins with'' [[pancreatic duct]] '''→''' ''forming'' [[ampulla of Vater]] '''→''' ''enters'' [[duodenum]]
| |
|
| |
| <gallery perRow="3">
| |
| Image:Illu pancrease.jpg|Region of pancreas
| |
| Image:Gray848.png|The celiac ganglia with the sympathetic plexuses of the abdominal viscera radiating from the ganglia.
| |
| Image:Gray1039.png|Horizontal disposition of the peritoneum in the upper part of the abdomen.
| |
| Image:Gray1057.png|Interior of the descending portion of the duodenum, showing bile papilla.
| |
| Image:Gray1086-liver.PNG|Inferior surface of the liver.
| |
| Image:Gray1099.png|The pancreas and duodenum from behind.
| |
| Image:Gray1100.png|The pancreatic duct.
| |
| Image:Bilebladder.png|The portal vein and its tributaries.
| |
| Image:Illu liver gallbladder.jpg|Liver and gallbladder
| |
| </gallery>
| |
|
| |
| ==Causes==
| |
| Many biliary cysts are congenitally acquired, perhaps as a consequence of unequal proliferation of epithelial cells during embryonic biliary duct development. Some biliary cysts are acquired, and some may develop in association with anatomic variations that lead to abnormally high ductal pressures in association with other predisposing factors.
| |
| ==Natural history, Complications and Prognosis==
| |
| Future complications include [[cholangitis]] and a 2% risk of malignancy, which may develop in any part of the biliary tree.
| |
| ==Diagnosis== | | ==Diagnosis== |
| ===History and Symptoms===
| |
|
| |
|
| Most of them present in 1st year of life; adult presentation is rare and usually at this stage is associated with complication.
| | [[Bile duct cyst history and symptoms|History and Symptoms]] | [[Bile duct cyst physical examination|Physical Examination]] | [[Bile duct cyst laboratory findings|Laboratory Findings]] | [[Bile duct cyst CT|CT]] | [[Bile duct cyst echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Bile duct cyst other imaging findings|Other Imaging Findings]] |
| | |
| Classic triad (listed below) is found only in minority of patients:
| |
| * [[abdominal pain|intermittent abdominal pain]]
| |
| * [[jaundice]],
| |
| * [[abdominal mass|right upper quadrant abdominal mass]]
| |
| | |
| A hepatic cyst may be present, as may short stature. A fever of unknown origin may be observed. [[Pancreatitis]] may be present.
| |
| === MRI and CT ===
| |
| * Abdominal CT scans are also often diagnostic.
| |
| === Ultrasonography ===
| |
| * Ultrasound is often adequate for the diagnosis of biliary cysts, except for Type III choledochoceles. Biliary cysts can often even be picked up in utero.
| |
| === Other Imaging Findings ===
| |
| * [[Cholescintigraphy]] ([[HIDA scan]]s) is also quite useful for all but Type III choledochoceles. Findings include biliary tract dilatation and tracer retention after 24 hours. It gives data on excretory function, which is also useful post surgical repair.
| |
| * Endoscopic Retrograde Cholangio-Pancreatography (ERCP) provides excellent visualization.
| |
| * ERCP is particularly useful for type III choledochoceles, demonstrating a clubbed distal [[common bile duct]] (CBD) and a round, cyst-like, contrast-filled structure in the terminal CBD often extending into the duodenal lumen.
| |
| * Magnetic resonance cholangiopancreatography (MRCP) is also a available for evaluation.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| Biliary duct cysts are treated by surgical excision of the cyst with the formation of a [[roux-en-Y]] anastamosis to the [[biliary duct]].
| |
|
| |
| * '''Intrahepatic biliary''' cyst treatment depends on degree of involvement.
| |
| *:* Segmental disease can be potentially cured with '''lobectomy'''. The risks and benefits of undergoing this surgery, versus the associated risks of future cholangitis, stone disease, pancreatitis, and liver abscess if not treated surgically have to be weighed in individual patients.
| |
| *:* If both lobes are involved, surgical resection may not be an option.
| |
| *:*:* If patients have recurrent cholangitis, a trial of prophylactic antibiotics could be considered.
| |
| *:*:* '''Liver transplant''' is a final option.
| |
| *:* '''Cholecystectomy''' is indicated because it reduces the likelihood of cholangitis, and because the gallbladder is at increased risk of malignancy in patients with biliary cysts.
| |
| *:* A report in the Lancet describes a significant improvement in stone disease in Caroli’s disease patients treated with ursodeoxycholic acid (Actigall) 10-20 mg/kg/d.
| |
| * '''Extrahepatic biliary cysts''' are often treated with surgical repair due to risks of cyst rupture with secondary peritonitis, cholangitis and liver cirrhosis.
| |
| *:* Surgical options include primary cyst excision, and internal drainage procedures, such as choledochoduodenostomy and Roun-en-Y choledochojejunostomy. The down sides of internal drainage include a high complication rate and risk of malignancy in the abnormal region (2.5%).
| |
|
| |
|
| | [[Bile duct cyst surgery|Surgery]] | [[Bile duct cyst primary prevention|Primary Prevention]] | [[Bile duct cyst secondary prevention|Secondary Prevention]] | [[Bile duct cyst cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Bile duct cyst future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| ==References== | | ==Case Studies== |
| {{Reflist|2}}
| | [[Bile duct cyst case study one|Case #1]] |
|
| |
|
| [[Category:Gastroenterology]] | | [[Category:Gastroenterology]] |