Belinostat: Difference between revisions
No edit summary |
m (Protected "Belinostat": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 5: | Line 5: | ||
|drugClass=antineoplastic agent | |drugClass=antineoplastic agent | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication= | |indication=patients with relapsed or refractory peripheral [[T-cell lymphoma]] (PTCL). | ||
|adverseReactions=[[nausea]], [[fatigue]], [[pyrexia]], [[anemia]], and [[vomiting]], [[pneumonia]], [[pyrexia]], [[infection]], [[anemia]], [[increased creatinine]], [[thrombocytopenia]], and [[multi-organ failure]]. | |adverseReactions=[[nausea]], [[fatigue]], [[pyrexia]], [[anemia]], and [[vomiting]], [[pneumonia]], [[pyrexia]], [[infection]], [[anemia]], [[increased creatinine]], [[thrombocytopenia]], and [[multi-organ failure]]. | ||
<!--Black Box Warning--> | <!--Black Box Warning--> | ||
| Line 17: | Line 17: | ||
<!--FDA-Labeled Indications and Dosage (Adult)--> | <!--FDA-Labeled Indications and Dosage (Adult)--> | ||
|fdaLIADAdult======Peripheral T-cell lymphoma===== | |fdaLIADAdult======Peripheral T-cell lymphoma===== | ||
* | *Belinostat is indicated for the treatment of patients with relapsed or refractory peripheral [[T-cell lymphoma]] (PTCL). | ||
*This indication is approved under accelerated approval based on tumor response rate and duration of response . An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial. | *This indication is approved under accelerated approval based on tumor response rate and duration of response . An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial. | ||
====Dosing Information==== | ====Dosing Information==== | ||
*The recommended dosage of | *The recommended dosage of Belinostat is 1,000 mg/m2 administered over 30 minutes by intravenous infusion once daily on Days 1-5 of a 21-day cycle. Cycles can be repeated every 21 days until disease progression or unacceptable toxicity. | ||
=====Dosage Modification for Hematologic and Non-Hematologic Toxicities===== | =====Dosage Modification for Hematologic and Non-Hematologic Toxicities===== | ||
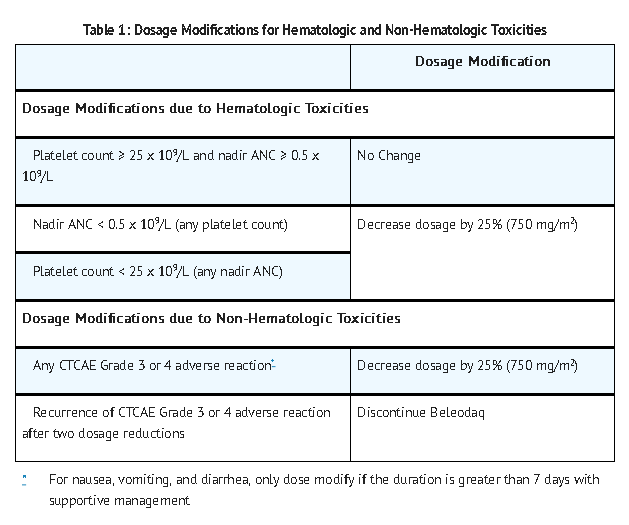
*Table 1 displays the recommended | *Table 1 displays the recommended Belinostat dosage modifications for hematologic and non-hematologic toxicities. Base dosage adjustments for [[thrombocytopenia]] and [[neutropenia]] on platelet and absolute neutrophil nadir (lowest value) counts in the preceding cycle of therapy. | ||
:*[[Absolute neutrophil count]] (ANC) should be greater than or equal to 1.0 x 10 9/L and the platelet count should be greater than or equal to 50 x 10 9/L prior to the start of each cycle and prior to resuming treatment following toxicity. Resume subsequent treatment with | :*[[Absolute neutrophil count]] (ANC) should be greater than or equal to 1.0 x 10 9/L and the platelet count should be greater than or equal to 50 x 10 9/L prior to the start of each cycle and prior to resuming treatment following toxicity. Resume subsequent treatment with Belinostat according to the guidelines described in Table 1 below. Discontinue Belinostat in patients who have recurrent [[ANC]] nadirs less than 0.5 x 10 9/L and/or recurrent [[platelet count]] nadirs less than 25 x 10 9/L after two dosage reductions. | ||
:*Other toxicities must be NCI-CTCAE Grade 2 or less prior to re-treatment. | :*Other toxicities must be NCI-CTCAE Grade 2 or less prior to re-treatment. | ||
*Monitor complete blood counts at baseline and weekly. Perform serum chemistry tests, including renal and hepatic functions prior to the start of the first dose of each cycle. | *Monitor complete blood counts at baseline and weekly. Perform serum chemistry tests, including renal and hepatic functions prior to the start of the first dose of each cycle. | ||
[[File: | [[File:Belinostat02.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
=====Patients with Reduced UGT1A1 Activity===== | =====Patients with Reduced UGT1A1 Activity===== | ||
*Reduce the starting dose of | *Reduce the starting dose of Belinostat to 750 mg/m2 in patients known to be homozygous for the UGT1A1*28 allele. | ||
=====Preparation and Administration Precautions===== | =====Preparation and Administration Precautions===== | ||
*As with other potentially cytotoxic anticancer agents, exercise care in the handling and preparation of solutions prepared with | *As with other potentially cytotoxic anticancer agents, exercise care in the handling and preparation of solutions prepared with Belinostat . | ||
=====Reconstitution and Infusion Instructions===== | =====Reconstitution and Infusion Instructions===== | ||
*Aseptically reconstitute each vial of | *Aseptically reconstitute each vial of Belinostat by adding 9 mL of Sterile Water for injection, USP, into the Belinostat vial with a suitable syringe to achieve a concentration of 50 mg of belinostat per mL. Swirl the contents of the vial until there are no visible particles in the resulting solution. The reconstituted product may be stored for up to 12 hours at ambient temperature (15-25°C; 59-77°F). | ||
*Aseptically withdraw the volume needed for the required dosage (based on the 50 mg/mL concentration and the patient’s [[BSA]] [m 2]) and transfer to an [[infusion bag]] containing 250 mL of 0.9 % [[Sodium Chloride injection]]. The infusion bag with drug solution may be stored at ambient room temperature (15-25°C; 59-77°F) for up to 36 hours including infusion time. | *Aseptically withdraw the volume needed for the required dosage (based on the 50 mg/mL concentration and the patient’s [[BSA]] [m 2]) and transfer to an [[infusion bag]] containing 250 mL of 0.9 % [[Sodium Chloride injection]]. The infusion bag with drug solution may be stored at ambient room temperature (15-25°C; 59-77°F) for up to 36 hours including infusion time. | ||
*Visually inspect the solution for particulate matter. Do not use if cloudiness or particulates are observed. | *Visually inspect the solution for particulate matter. Do not use if cloudiness or particulates are observed. | ||
| Line 59: | Line 59: | ||
* | *Belinostat can cause [[thrombocytopenia]], [[leukopenia]] ([[neutropenia]] and [[lymphopenia]]), and/or [[anemia]]; monitor [[blood counts]] weekly during treatment, and modify dosage as necessary . | ||
=====Infections===== | =====Infections===== | ||
*Serious and sometimes fatal infections, including [[pneumonia]] and [[sepsis]], have occurred with | *Serious and sometimes fatal infections, including [[pneumonia]] and [[sepsis]], have occurred with Belinostat . Do not administer Belinostat to patients with an active [[infection]]. Patients with a history of extensive or intensive [[chemotherapy]] may be at higher risk of [[life threatening infection]]s. | ||
=====Hepatotoxicity===== | =====Hepatotoxicity===== | ||
* | *Belinostat can cause fatal [[hepatotoxicity]] and [[liver function test]] abnormalities . Monitor [[liver function test]]s before treatment and before the start of each cycle. Interrupt or adjust dosage until recovery, or permanently discontinue Belinostat based on the severity of the hepatic toxicity | ||
=====Tumor Lysis Syndrome===== | =====Tumor Lysis Syndrome===== | ||
*[[Tumor lysis syndrome]] has occurred in | *[[Tumor lysis syndrome]] has occurred in Belinostat -treated patients in the clinical trial of patients with relapsed or refractory PTCL . Monitor patients with advanced stage disease and/or high tumor burden and take appropriate precautions . | ||
=====Gastrointestinal Toxicity===== | =====Gastrointestinal Toxicity===== | ||
*[[Nausea]], [[vomiting]] and [[diarrhea]] occur with | *[[Nausea]], [[vomiting]] and [[diarrhea]] occur with Belinostat and may require the use of [[antiemetic]] and [[antidiarrheal medication]]s. | ||
=====Embryo-fetal Toxicity===== | =====Embryo-fetal Toxicity===== | ||
* | *Belinostat can cause fetal harm when administered to a pregnant woman. Belinostat may cause [[teratogenicity]] and/or embryo-fetal lethality because it is [[genotoxic]] and targets actively dividing cells . Women of childbearing potential should be advised to avoid [[pregnancy]] while receiving Belinostat . If this drug is used during [[pregnancy]], or if the patient becomes pregnant while taking this drug, the patient should be apprised of potential hazard to the fetus | ||
| Line 87: | Line 87: | ||
:*[[Tumor Lysis Syndrome]] | :*[[Tumor Lysis Syndrome]] | ||
:*[[Gastrointestinal Toxicity]] | :*[[Gastrointestinal Toxicity]] | ||
:*The most common adverse reactions observed in the trial of patients with relapsed or refractory [[PTCL]] treated with | :*The most common adverse reactions observed in the trial of patients with relapsed or refractory [[PTCL]] treated with Belinostat were [[nausea]], [[fatigue]], [[pyrexia]], [[anemia]], and [[vomiting]] . | ||
=====Clinical Trials Experience===== | =====Clinical Trials Experience===== | ||
*Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of | *Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of Belinostat may not reflect the rates observed in practice. | ||
======Adverse Reactions in Patients with Peripheral T-Cell Lymphoma====== | ======Adverse Reactions in Patients with Peripheral T-Cell Lymphoma====== | ||
*The safety of | *The safety of Belinostat was evaluated in 129 patients with relapsed or refractory [[PTCL]] in the single arm clinical trial in which patients were administered Belinostat at a dosage of 1,000 mg/m2 administered over 30 minutes by IV infusion once daily on Days 1-5 of a 21-day cycle . The median duration of treatment was 2 cycles (range 1 – 33 cycles). | ||
Table 2 summarizes the adverse reactions regardless of causality from the trial in patients with relapsed or refractory [[PTCL]]. | Table 2 summarizes the adverse reactions regardless of causality from the trial in patients with relapsed or refractory [[PTCL]]. | ||
[[File: | [[File:Belinostat03.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
'''''Note: Adverse reactions are listed by order of incidence in the “All Grades” category first, then by incidence in “the Grade 3 or 4” category; MedDRA = Medical Dictionary for Regulatory Activities; Severity measured by National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 3.0''''' | '''''Note: Adverse reactions are listed by order of incidence in the “All Grades” category first, then by incidence in “the Grade 3 or 4” category; MedDRA = Medical Dictionary for Regulatory Activities; Severity measured by National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 3.0''''' | ||
======Serious Adverse Reactions====== | ======Serious Adverse Reactions====== | ||
*Sixty-one patients (47.3%) experienced serious adverse reactions while taking | *Sixty-one patients (47.3%) experienced serious adverse reactions while taking Belinostat or within 30 days after their last dose of Belinostat . The most common serious adverse reactions (> 2%) were [[pneumonia]], [[pyrexia]], [[infection]], [[anemia]], [[increased creatinine]], [[thrombocytopenia]], and [[multi-organ failure]]. One treatment-related death associated with [[hepatic failure]] was reported in the trial. | ||
*One patient with baseline [[hyperuricemia]] and bulky disease experienced Grade 4 [[tumor lysis syndrome]] during the first cycle of treatment and died due to [[multi-organ failure]]. A treatment-related death from [[ventricular fibrillation]] was reported in another monotherapy clinical trial with | *One patient with baseline [[hyperuricemia]] and bulky disease experienced Grade 4 [[tumor lysis syndrome]] during the first cycle of treatment and died due to [[multi-organ failure]]. A treatment-related death from [[ventricular fibrillation]] was reported in another monotherapy clinical trial with Belinostat . ECG analysis did not identify [[QT prolongation|QTc prolongation]]. | ||
======Discontinuations due to Adverse Reactions====== | ======Discontinuations due to Adverse Reactions====== | ||
*Twenty-five patients (19.4%) discontinued treatment with | *Twenty-five patients (19.4%) discontinued treatment with Belinostat due to adverse reactions. The adverse reactions reported most frequently as the reason for discontinuation of treatment included [[anemia]], [[febrile neutropenia]], [[fatigue]], and [[multi-organ failure]]. | ||
======Dosage Modifications due to Adverse Reactions====== | ======Dosage Modifications due to Adverse Reactions====== | ||
*In the trial, dosage adjustments due to adverse reactions occurred in 12% of | *In the trial, dosage adjustments due to adverse reactions occurred in 12% of Belinostat -treated patients. | ||
There is limited information regarding <i>Clinical Trial Experience</i> of | There is limited information regarding <i>Clinical Trial Experience</i> of Belinostat in the drug label. | ||
<!--Postmarketing Experience--> | <!--Postmarketing Experience--> | ||
|postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of | |postmarketing=There is limited information regarding <i>Postmarketing Experience</i> of Belinostat in the drug label. | ||
| Line 124: | Line 124: | ||
<!--Drug Interactions--> | <!--Drug Interactions--> | ||
|drugInteractions======UGT1A1 Inhibitors===== | |drugInteractions======UGT1A1 Inhibitors===== | ||
*Belinostat is primarily metabolized by UGT1A1. Avoid concomitant administration of | *Belinostat is primarily metabolized by UGT1A1. Avoid concomitant administration of Belinostat with strong inhibitors of UGT1A1 . | ||
=====Warfarin===== | =====Warfarin===== | ||
*Co-administration of | *Co-administration of Belinostat and [[warfarin]] resulted in no clinically relevant increase in plasma exposure of either R-[[warfarin]] or S-[[warfarin]] that would require a dose adjustment | ||
<!--Use in Specific Populations--> | <!--Use in Specific Populations--> | ||
|FDAPregCat=D | |FDAPregCat=D | ||
|useInPregnancyFDA= | |useInPregnancyFDA======Risk Summary===== | ||
=====Risk Summary===== | |||
* | *Belinostat may cause [[teratogenicity]] and/or embryo-fetal lethality because it is a [[genotoxic]] drug and targets actively dividing cells . Women should avoid [[pregnancy]] while receiving Belinostat . If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of potential hazard to the fetus. | ||
=====Animal Data===== | =====Animal Data===== | ||
*No reproductive and developmental animal toxicology studies have been conducted with belinostat. | *No reproductive and developmental animal toxicology studies have been conducted with belinostat. | ||
|useInPregnancyAUS=There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of | |useInPregnancyAUS=There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Belinostat in women who are pregnant. | ||
|useInLaborDelivery=There is no FDA guidance on use of | |useInLaborDelivery=There is no FDA guidance on use of Belinostat during labor and delivery. | ||
|useInNursing=*It is not known whether belinostat is excreted in human milk. Because many drugs are excreted in [[Breast milk |human milk]] and because of the potential for serious adverse reactions in nursing infants from | |useInNursing=*It is not known whether belinostat is excreted in human milk. Because many drugs are excreted in [[Breast milk |human milk]] and because of the potential for serious adverse reactions in nursing infants from Belinostat , a decision should be made whether to discontinue nursing or discontinue drug, taking into account the importance of the drug to the mother. | ||
|useInPed=*Pediatric patients were not included in clinical trials. The safety and effectiveness of | |useInPed=*Pediatric patients were not included in clinical trials. The safety and effectiveness of Belinostat in pediatric patients have not been established. | ||
|useInGeri=*In the single-arm trial, 48% of patients (n = 62) were ≥ 65 years of age and 10% of patients (n=13) were ≥ 75 years of age . The median age of the trial population was 63 years. Patients ≥ 65 years of age had a higher response rate to | |useInGeri=*In the single-arm trial, 48% of patients (n = 62) were ≥ 65 years of age and 10% of patients (n=13) were ≥ 75 years of age . The median age of the trial population was 63 years. Patients ≥ 65 years of age had a higher response rate to Belinostat treatment than patients < 65 years of age (36% versus 16%) while no meaningful differences in response rate were observed between patients ≥ 75 years of age and those < 75 years of age. No clinically meaningful differences in serious adverse reactions were observed in patients based on age (< 65 years compared with ≥ 65 years or < 75 years of age compared with ≥ 75 years of age). | ||
|useInGender=There is no FDA guidance on the use of | |useInGender=There is no FDA guidance on the use of Belinostat with respect to specific gender populations. | ||
|useInRace=There is no FDA guidance on the use of | |useInRace=There is no FDA guidance on the use of Belinostat with respect to specific racial populations. | ||
|useInRenalImpair=*Approximately 40% of the belinostat dose is excreted renally, primarily as metabolites. Belinostat exposure is not altered in patients with [[Creatinine Clearance]] ([[CLcr]]) > 39 mL/min. There is insufficient data to recommend a dose of | |useInRenalImpair=*Approximately 40% of the belinostat dose is excreted renally, primarily as metabolites. Belinostat exposure is not altered in patients with [[Creatinine Clearance]] ([[CLcr]]) > 39 mL/min. There is insufficient data to recommend a dose of Belinostat in patients with [[CLcr]] ≤ 39 mL/min. | ||
|useInHepaticImpair=*Belinostat is metabolized in the liver and hepatic impairment is expected to increase exposure to belinostat. Patients with moderate and severe hepatic impairment ([[total bilirubin]] >1.5 x upper limit of normal (ULN)) were excluded from clinical trials. | |useInHepaticImpair=*Belinostat is metabolized in the liver and hepatic impairment is expected to increase exposure to belinostat. Patients with moderate and severe hepatic impairment ([[total bilirubin]] >1.5 x upper limit of normal (ULN)) were excluded from clinical trials. | ||
There is insufficient data to recommend a dose of | There is insufficient data to recommend a dose of Belinostat in patients with moderate and severe hepatic impairment | ||
|useInReproPotential=There is no FDA guidance on the use of | |useInReproPotential=There is no FDA guidance on the use of Belinostat in women of reproductive potentials and males. | ||
|useInImmunocomp=There is no FDA guidance one the use of | |useInImmunocomp=There is no FDA guidance one the use of Belinostat in patients who are [[immunocompromised]]. | ||
<!--Administration and Monitoring--> | <!--Administration and Monitoring--> | ||
|administration=* Intravenous | |administration=* Intravenous | ||
|monitoring=* | |monitoring=*Belinostat can cause [[thrombocytopenia]], [[leukopenia]] ([[neutropenia]] and [[lymphopenia]]), and/or anemia; monitor blood counts weekly during treatment, and modify dosage as necessary. | ||
<!--IV Compatibility--> | <!--IV Compatibility--> | ||
|IVCompat=There is limited information regarding <i>IV Compatibility</i> of | |IVCompat=There is limited information regarding <i>IV Compatibility</i> of Belinostat in the drug label. | ||
<!--Overdosage--> | <!--Overdosage--> | ||
|overdose=*No specific information is available on the treatment of overdosage of | |overdose=*No specific information is available on the treatment of overdosage of Belinostat . There is no antidote for Belinostat and it is not known if Belinostat is dialyzable. If an overdose occurs, general supportive measures should be instituted as deemed necessary by the treating physician. The elimination half-life of belinostat is 1.1 hours | ||
<!--Pharmacology--> | <!--Pharmacology--> | ||
<!--Drug box 2--> | <!--Drug box 2--> | ||
|drugBox=[[File: | |drugBox=[[File:Belinostat00.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
<!--Mechanism of Action--> | <!--Mechanism of Action--> | ||
|mechAction=* | |mechAction=*Belinostat is a [[histone deacetylase]] (HDAC) inhibitor. HDACs catalyze the removal of acetyl groups from the lysine residues of [[histone]]s and some [[non-histone proteins]]. In vitro, belinostat caused the accumulation of acetylated histones and other proteins, inducing cell cycle arrest and/or apoptosis of some transformed cells. Belinostat shows preferential [[cytotoxicity]] towards [[tumor cells]] compared to normal cells. Belinostat inhibited the enzymatic activity of [[histone deacetylase]]s at nanomolar concentrations (<250 nM). | ||
<!--Structure--> | <!--Structure--> | ||
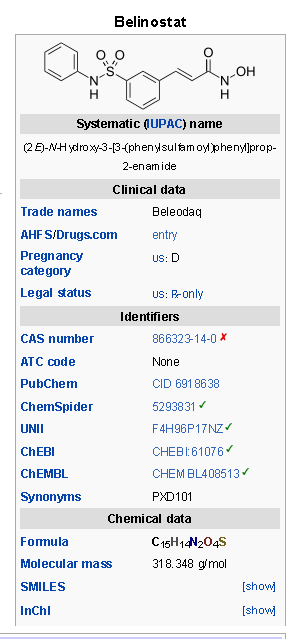
|structure=* | |structure=*Belinostat is a [[histone deacetylase]] inhibitor with a [[sulfonamide]]-hydroxamide structure. The chemical name of belinostat is (2E)-N-hydroxy-3-[3-(phenylsulfamoyl)phenyl]prop-2-enamide. The structural formula is as follows: | ||
[[File: | [[File:Belinostat01.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
The molecular formula is C15H14N2O4S and the molecular weight is 318.35 g/mol. | The molecular formula is C15H14N2O4S and the molecular weight is 318.35 g/mol. | ||
*Belinostat is a white to off-white powder. It is slightly soluble in distilled water (0.14 mg/mL) and polyethylene glycol 400 (about 1.5 mg/mL), and is freely soluble in [[ethanol]] (> 200 mg/mL). The pKa values are 7.87 and 8.71 by [[potentiometry]] and 7.86 and 8.59 by UV. | *Belinostat is a white to off-white powder. It is slightly soluble in distilled water (0.14 mg/mL) and polyethylene glycol 400 (about 1.5 mg/mL), and is freely soluble in [[ethanol]] (> 200 mg/mL). The pKa values are 7.87 and 8.71 by [[potentiometry]] and 7.86 and 8.59 by UV. | ||
* | *Belinostat (belinostat) for injection is supplied as a sterile lyophilized yellow powder containing 500 mg belinostat as the active ingredient. Each vial also contains 1000 mg L-[[Arginine]], USP as an inactive ingredient. The drug product is supplied in a single-use 30 mL clear glass vial with a coated stopper and [[aluminum]] crimp seal with “flip-off” cap. Belinostat is intended for [[intravenous]] administration after reconstitution with 9 mL Sterile Water for injection, and the reconstituted solution is further diluted with 250 mL of sterile 0.9% [[Sodium Chloride]] injection prior to infusion | ||
<!--Pharmacodynamics--> | <!--Pharmacodynamics--> | ||
|PD======Cardiac Electrophysiology===== | |PD======Cardiac Electrophysiology===== | ||
*Multiple clinical trials have been conducted with | *Multiple clinical trials have been conducted with Belinostat , in many of which ECG data were collected and analyzed by a central laboratory. Analysis of clinical ECG and belinostat [[plasma concentration]] data demonstrated no meaningful effect of Belinostat on [[cardiac repolarization]]. None of the trials showed any clinically relevant changes caused by Belinostat on heart rate, PR duration or [[QRS duration]] as measures of autonomic state, [[atrio-ventricular conduction]] or depolarization; there were no cases of [[Torsades de Pointes]]. | ||
|PK=*The pharmacokinetic characteristics of belinostat were analyzed from pooled data from phase 1/2 clinical studies that used doses of belinostat ranging from 150 to 1200 mg/m2. The total mean [[plasma clearance]] and elimination [[half-life]] were 1240 mL/min and 1.1 hours, respectively. The total clearance approximates average hepatic blood flow (1500 mL/min), suggesting high hepatic extraction (clearance being flow dependent). | |PK=*The pharmacokinetic characteristics of belinostat were analyzed from pooled data from phase 1/2 clinical studies that used doses of belinostat ranging from 150 to 1200 mg/m2. The total mean [[plasma clearance]] and elimination [[half-life]] were 1240 mL/min and 1.1 hours, respectively. The total clearance approximates average hepatic blood flow (1500 mL/min), suggesting high hepatic extraction (clearance being flow dependent). | ||
| Line 199: | Line 198: | ||
*In vitro studies showed belinostat and its metabolites (including belinostat glucuronide, belinostat amide, methyl belinostat) inhibited metabolic activities of CYP2C8 and CYP2C9. Other metabolites (3-ASBA and belinostat acid) inhibited CYP2C8. | *In vitro studies showed belinostat and its metabolites (including belinostat glucuronide, belinostat amide, methyl belinostat) inhibited metabolic activities of CYP2C8 and CYP2C9. Other metabolites (3-ASBA and belinostat acid) inhibited CYP2C8. | ||
*In cancer patients, co-administration of | *In cancer patients, co-administration of Belinostat (1,000 mg/m2) and [[warfarin]] (5 mg), a known [[CYP2C9]] substrate, did not increase the AUC or Cmax of either R- or S-[[warfarin]]. | ||
*Belinostat is likely a [[glycoprotein]] (P-gp) substrate but is unlikely to inhibit [[P-gp]]. | *Belinostat is likely a [[glycoprotein]] (P-gp) substrate but is unlikely to inhibit [[P-gp]]. | ||
| Line 206: | Line 205: | ||
*UGT1A1 activity is reduced in individuals with genetic polymorphisms that lead to reduced enzyme activity such as the [[UGT1A1*28 polymorphism]]. Approximately 20% of the black population, 10% of the white population, and 2% of the Asian population are [[homozygous]] for the [[UGT1A1*28 allele]]. Additional reduced function [[allele]]s may be more prevalent in specific populations. | *UGT1A1 activity is reduced in individuals with genetic polymorphisms that lead to reduced enzyme activity such as the [[UGT1A1*28 polymorphism]]. Approximately 20% of the black population, 10% of the white population, and 2% of the Asian population are [[homozygous]] for the [[UGT1A1*28 allele]]. Additional reduced function [[allele]]s may be more prevalent in specific populations. | ||
*Because belinostat is primarily (80 -90%) metabolized by UGT1A1, the clearance of belinostat could be decreased in patients with reduced [[UGT1A1 activity]] (e.g., patients with [[UGT1A1*28 allele]]). Reduce the starting dose of | *Because belinostat is primarily (80 -90%) metabolized by UGT1A1, the clearance of belinostat could be decreased in patients with reduced [[UGT1A1 activity]] (e.g., patients with [[UGT1A1*28 allele]]). Reduce the starting dose of Belinostat to 750 mg/m2 in patients known to be homozygous for the UGT1A1*28 allele to minimize dose limiting toxicities. | ||
<!--Nonclinical Toxicology--> | <!--Nonclinical Toxicology--> | ||
|nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | |nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility===== | ||
| Line 213: | Line 212: | ||
*Belinostat was [[genotoxic]] in a bacterial reverse mutation test ([[Ames assay]]), an in vitro mouse [[lymphoma cell]] mutagenesis assay, and an in vivo rat [[micronucleus assay]]. | *Belinostat was [[genotoxic]] in a bacterial reverse mutation test ([[Ames assay]]), an in vitro mouse [[lymphoma cell]] mutagenesis assay, and an in vivo rat [[micronucleus assay]]. | ||
* | *Belinostat may impair male [[fertility]]. [[Fertility]] studies using belinostat were not conducted. However, belinostat effects on male reproductive organs observed during the 24-week repeat-dose dog toxicology study included reduced organ weights of the [[testes]]/[[epididymides]] that correlated with a delay in testicular maturation | ||
<!--Clinical Studies--> | <!--Clinical Studies--> | ||
|clinicalStudies=======Relapsed or Refractory Peripheral T-cell Lymphoma (PTCL)====== | |clinicalStudies=======Relapsed or Refractory Peripheral T-cell Lymphoma (PTCL)====== | ||
*In an open-label, single-arm, non-randomized international trial conducted at 62 centers, 129 patients with relapsed or refractory PTCL were treated with | *In an open-label, single-arm, non-randomized international trial conducted at 62 centers, 129 patients with relapsed or refractory PTCL were treated with Belinostat 1,000 mg/m2 administered over 30 minutes via IV infusion once daily on Days 1-5 of a 21-day cycle. There were 120 patients who had histologically confirmed [[PTCL]] by central review evaluable for efficacy. Patients were treated with repeat cycles every three weeks until disease progression or unacceptable toxicity. | ||
*The primary efficacy endpoint was response rate (complete response and partial response) as assessed by an independent review committee (IRC) using the International Workshop Criteria (IWC) (Cheson 2007). The key secondary efficacy endpoint was duration of response. Response assessments were evaluated every 6 weeks for the first 12 months and then every 12 weeks until 2 years from the start of study treatment. Duration of response was measured from the first day of documented response to disease progression or death. Response and progression of disease were evaluated by the IRC using the IWC. | *The primary efficacy endpoint was response rate (complete response and partial response) as assessed by an independent review committee (IRC) using the International Workshop Criteria (IWC) (Cheson 2007). The key secondary efficacy endpoint was duration of response. Response assessments were evaluated every 6 weeks for the first 12 months and then every 12 weeks until 2 years from the start of study treatment. Duration of response was measured from the first day of documented response to disease progression or death. Response and progression of disease were evaluated by the IRC using the IWC. | ||
| Line 223: | Line 222: | ||
*Table 3 summarizes the baseline demographic and disease characteristics of the study population, who were evaluable for efficacy. | *Table 3 summarizes the baseline demographic and disease characteristics of the study population, who were evaluable for efficacy. | ||
[[File: | [[File:Belinostat04.png|thumb|none|600px|This image is provided by the National Library of Medicine.]] | ||
*The median duration of response based on the first date of response to disease progression or death was 8.4 months (95% CI: 4.5 – 29.4). Of the responders, the median time to response was 5.6 weeks (range 4.3 - 50.4 weeks). Nine patients (7.5%) were able to proceed to a stem cell transplant after treatment with | *The median duration of response based on the first date of response to disease progression or death was 8.4 months (95% CI: 4.5 – 29.4). Of the responders, the median time to response was 5.6 weeks (range 4.3 - 50.4 weeks). Nine patients (7.5%) were able to proceed to a stem cell transplant after treatment with Belinostat . | ||
<!--How Supplied--> | <!--How Supplied--> | ||
|howSupplied======How Supplied===== | |howSupplied======How Supplied===== | ||
* | *Belinostat (belinostat) for injection is supplied in single vial cartons; each 30 mL clear vial contains sterile, lyophilized powder equivalent to 500 mg belinostat. | ||
*NDC 68152-108-09: Individual carton of | *NDC 68152-108-09: Individual carton of Belinostat 30 mL single-use vial containing 500 mg belinostat. | ||
<!--Patient Counseling Information--> | <!--Patient Counseling Information--> | ||
|storage=*Store | |storage=*Store Belinostat (belinostat) for injection at room temperature 20°C to 25°C (68°C to 77°F). Excursions are permitted between 15°C and 30°C (59°F and 86°F). Retain in original package until use. . | ||
* | *Belinostat is a [[cytotoxic]] drug. Follow special handling and disposal procedures | ||
|fdaPatientInfo=*Physicians should discuss the FDA approved Patient Information Leaflet with patients prior to treatment with | |fdaPatientInfo=*Physicians should discuss the FDA approved Patient Information Leaflet with patients prior to treatment with Belinostat . Instruct patients to read the Patient Information Leaflet carefully. | ||
*Advise the patient or the caregiver to read the FDA-approved patient labeling (Patient Information). | *Advise the patient or the caregiver to read the FDA-approved patient labeling (Patient Information). | ||
| Line 247: | Line 246: | ||
:*To report any symptoms of [[thrombocytopenia]], [[leukopenia]] ([[neutropenia]] and [[lymphopenia]]), and [[anemia]] . | :*To report any symptoms of [[thrombocytopenia]], [[leukopenia]] ([[neutropenia]] and [[lymphopenia]]), and [[anemia]] . | ||
:*To immediately report symptoms of infection (e.g., [[pyrexia]]) . | :*To immediately report symptoms of infection (e.g., [[pyrexia]]) . | ||
:*Of the potential risk to the fetus and for women to avoid [[pregnancy]] while receiving | :*Of the potential risk to the fetus and for women to avoid [[pregnancy]] while receiving Belinostat . | ||
:*To understand the importance of monitoring [[liver function test]] abnormalities and to immediately report potential symptoms of liver injury | :*To understand the importance of monitoring [[liver function test]] abnormalities and to immediately report potential symptoms of liver injury | ||
<!--Precautions with Alcohol--> | <!--Precautions with Alcohol--> | ||
|alcohol=* Alcohol- | |alcohol=* Alcohol-Belinostat interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
<!--Brand Names--> | <!--Brand Names--> | ||
|brandNames=* | |brandNames=* Belinostat ® | ||
<!--Look-Alike Drug Names--> | <!--Look-Alike Drug Names--> | ||
| Line 266: | Line 265: | ||
}} | }} | ||
{{LabelImage | {{LabelImage | ||
|fileName= | |fileName=Belinostat05.png | ||
}} | }} | ||
{{LabelImage | {{LabelImage | ||
|fileName= | |fileName=Belinostat06.png | ||
}} | }} | ||
<!--Pill Image--> | <!--Pill Image--> | ||
Latest revision as of 17:57, 18 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Aparna Vuppala, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Belinostat is an antineoplastic agent that is FDA approved for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (PTCL).. Common adverse reactions include nausea, fatigue, pyrexia, anemia, and vomiting, pneumonia, pyrexia, infection, anemia, increased creatinine, thrombocytopenia, and multi-organ failure..
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Peripheral T-cell lymphoma
- Belinostat is indicated for the treatment of patients with relapsed or refractory peripheral T-cell lymphoma (PTCL).
- This indication is approved under accelerated approval based on tumor response rate and duration of response . An improvement in survival or disease-related symptoms has not been established. Continued approval for this indication may be contingent upon verification and description of clinical benefit in the confirmatory trial.
Dosing Information
- The recommended dosage of Belinostat is 1,000 mg/m2 administered over 30 minutes by intravenous infusion once daily on Days 1-5 of a 21-day cycle. Cycles can be repeated every 21 days until disease progression or unacceptable toxicity.
Dosage Modification for Hematologic and Non-Hematologic Toxicities
- Table 1 displays the recommended Belinostat dosage modifications for hematologic and non-hematologic toxicities. Base dosage adjustments for thrombocytopenia and neutropenia on platelet and absolute neutrophil nadir (lowest value) counts in the preceding cycle of therapy.
- Absolute neutrophil count (ANC) should be greater than or equal to 1.0 x 10 9/L and the platelet count should be greater than or equal to 50 x 10 9/L prior to the start of each cycle and prior to resuming treatment following toxicity. Resume subsequent treatment with Belinostat according to the guidelines described in Table 1 below. Discontinue Belinostat in patients who have recurrent ANC nadirs less than 0.5 x 10 9/L and/or recurrent platelet count nadirs less than 25 x 10 9/L after two dosage reductions.
- Other toxicities must be NCI-CTCAE Grade 2 or less prior to re-treatment.
- Monitor complete blood counts at baseline and weekly. Perform serum chemistry tests, including renal and hepatic functions prior to the start of the first dose of each cycle.
Patients with Reduced UGT1A1 Activity
- Reduce the starting dose of Belinostat to 750 mg/m2 in patients known to be homozygous for the UGT1A1*28 allele.
Preparation and Administration Precautions
- As with other potentially cytotoxic anticancer agents, exercise care in the handling and preparation of solutions prepared with Belinostat .
Reconstitution and Infusion Instructions
- Aseptically reconstitute each vial of Belinostat by adding 9 mL of Sterile Water for injection, USP, into the Belinostat vial with a suitable syringe to achieve a concentration of 50 mg of belinostat per mL. Swirl the contents of the vial until there are no visible particles in the resulting solution. The reconstituted product may be stored for up to 12 hours at ambient temperature (15-25°C; 59-77°F).
- Aseptically withdraw the volume needed for the required dosage (based on the 50 mg/mL concentration and the patient’s BSA [m 2]) and transfer to an infusion bag containing 250 mL of 0.9 % Sodium Chloride injection. The infusion bag with drug solution may be stored at ambient room temperature (15-25°C; 59-77°F) for up to 36 hours including infusion time.
- Visually inspect the solution for particulate matter. Do not use if cloudiness or particulates are observed.
- Connect the infusion bag containing drug solution to an infusion set with a 0.22 µm in-line filter for administration.
- Infuse intravenously over 30 minutes. If infusion site pain or other symptoms potentially attributable to the infusion occur, the infusion time may be extended to 45 minutes.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Belinostat in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Belinostat in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Belinostat FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Belinostat in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Belinostat in pediatric patients.
Contraindications
- None.
Warnings
Hematologic Toxicity
- Belinostat can cause thrombocytopenia, leukopenia (neutropenia and lymphopenia), and/or anemia; monitor blood counts weekly during treatment, and modify dosage as necessary .
Infections
- Serious and sometimes fatal infections, including pneumonia and sepsis, have occurred with Belinostat . Do not administer Belinostat to patients with an active infection. Patients with a history of extensive or intensive chemotherapy may be at higher risk of life threatening infections.
Hepatotoxicity
- Belinostat can cause fatal hepatotoxicity and liver function test abnormalities . Monitor liver function tests before treatment and before the start of each cycle. Interrupt or adjust dosage until recovery, or permanently discontinue Belinostat based on the severity of the hepatic toxicity
Tumor Lysis Syndrome
- Tumor lysis syndrome has occurred in Belinostat -treated patients in the clinical trial of patients with relapsed or refractory PTCL . Monitor patients with advanced stage disease and/or high tumor burden and take appropriate precautions .
Gastrointestinal Toxicity
- Nausea, vomiting and diarrhea occur with Belinostat and may require the use of antiemetic and antidiarrheal medications.
Embryo-fetal Toxicity
- Belinostat can cause fetal harm when administered to a pregnant woman. Belinostat may cause teratogenicity and/or embryo-fetal lethality because it is genotoxic and targets actively dividing cells . Women of childbearing potential should be advised to avoid pregnancy while receiving Belinostat . If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of potential hazard to the fetus
Adverse Reactions
Clinical Trials Experience
- The following serious adverse reactions are described in more detail in other sections of the prescribing information.
- Hematologic Toxicity
- Infection
- Hepatotoxicity
- Tumor Lysis Syndrome
- Gastrointestinal Toxicity
- The most common adverse reactions observed in the trial of patients with relapsed or refractory PTCL treated with Belinostat were nausea, fatigue, pyrexia, anemia, and vomiting .
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of Belinostat may not reflect the rates observed in practice.
Adverse Reactions in Patients with Peripheral T-Cell Lymphoma
- The safety of Belinostat was evaluated in 129 patients with relapsed or refractory PTCL in the single arm clinical trial in which patients were administered Belinostat at a dosage of 1,000 mg/m2 administered over 30 minutes by IV infusion once daily on Days 1-5 of a 21-day cycle . The median duration of treatment was 2 cycles (range 1 – 33 cycles).
Table 2 summarizes the adverse reactions regardless of causality from the trial in patients with relapsed or refractory PTCL.
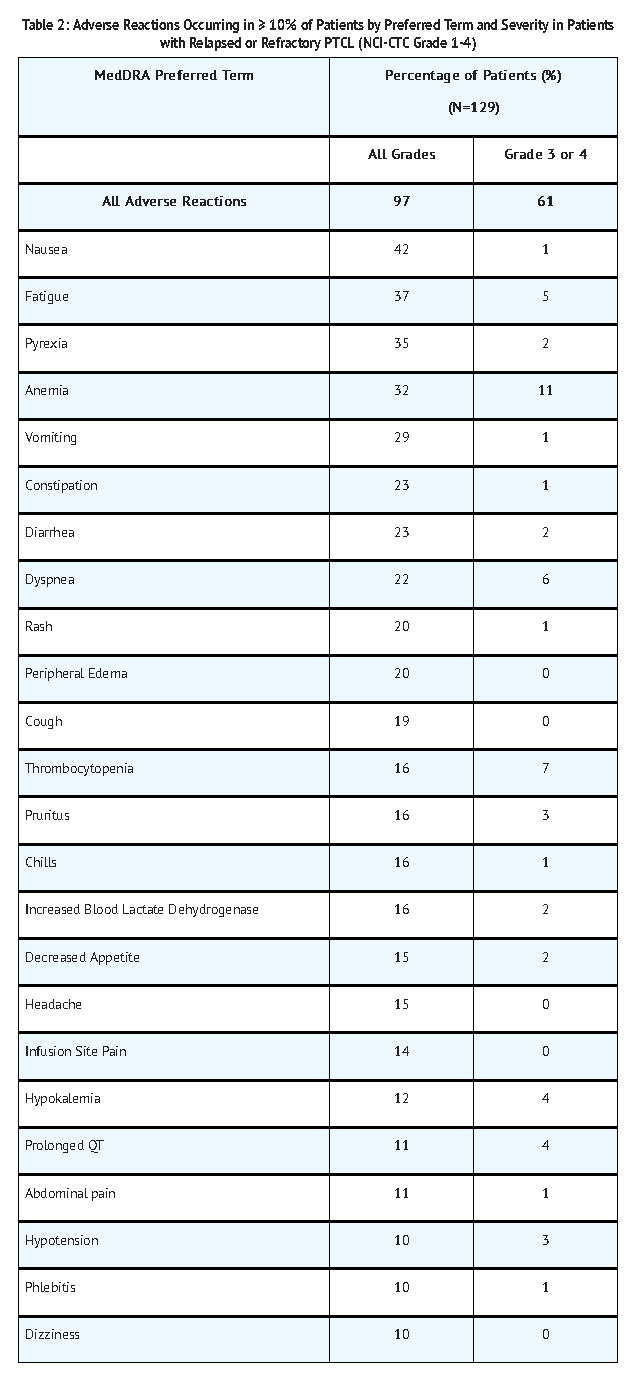
Note: Adverse reactions are listed by order of incidence in the “All Grades” category first, then by incidence in “the Grade 3 or 4” category; MedDRA = Medical Dictionary for Regulatory Activities; Severity measured by National Cancer Institute Common Terminology Criteria for Adverse Events (NCI-CTCAE) version 3.0
Serious Adverse Reactions
- Sixty-one patients (47.3%) experienced serious adverse reactions while taking Belinostat or within 30 days after their last dose of Belinostat . The most common serious adverse reactions (> 2%) were pneumonia, pyrexia, infection, anemia, increased creatinine, thrombocytopenia, and multi-organ failure. One treatment-related death associated with hepatic failure was reported in the trial.
- One patient with baseline hyperuricemia and bulky disease experienced Grade 4 tumor lysis syndrome during the first cycle of treatment and died due to multi-organ failure. A treatment-related death from ventricular fibrillation was reported in another monotherapy clinical trial with Belinostat . ECG analysis did not identify QTc prolongation.
Discontinuations due to Adverse Reactions
- Twenty-five patients (19.4%) discontinued treatment with Belinostat due to adverse reactions. The adverse reactions reported most frequently as the reason for discontinuation of treatment included anemia, febrile neutropenia, fatigue, and multi-organ failure.
Dosage Modifications due to Adverse Reactions
- In the trial, dosage adjustments due to adverse reactions occurred in 12% of Belinostat -treated patients.
There is limited information regarding Clinical Trial Experience of Belinostat in the drug label.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Belinostat in the drug label.
Drug Interactions
UGT1A1 Inhibitors
- Belinostat is primarily metabolized by UGT1A1. Avoid concomitant administration of Belinostat with strong inhibitors of UGT1A1 .
Warfarin
- Co-administration of Belinostat and warfarin resulted in no clinically relevant increase in plasma exposure of either R-warfarin or S-warfarin that would require a dose adjustment
Use in Specific Populations
Pregnancy
Risk Summary
- Belinostat may cause teratogenicity and/or embryo-fetal lethality because it is a genotoxic drug and targets actively dividing cells . Women should avoid pregnancy while receiving Belinostat . If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of potential hazard to the fetus.
Animal Data
- No reproductive and developmental animal toxicology studies have been conducted with belinostat.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Belinostat in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Belinostat during labor and delivery.
Nursing Mothers
- It is not known whether belinostat is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Belinostat , a decision should be made whether to discontinue nursing or discontinue drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Pediatric patients were not included in clinical trials. The safety and effectiveness of Belinostat in pediatric patients have not been established.
Geriatic Use
- In the single-arm trial, 48% of patients (n = 62) were ≥ 65 years of age and 10% of patients (n=13) were ≥ 75 years of age . The median age of the trial population was 63 years. Patients ≥ 65 years of age had a higher response rate to Belinostat treatment than patients < 65 years of age (36% versus 16%) while no meaningful differences in response rate were observed between patients ≥ 75 years of age and those < 75 years of age. No clinically meaningful differences in serious adverse reactions were observed in patients based on age (< 65 years compared with ≥ 65 years or < 75 years of age compared with ≥ 75 years of age).
Gender
There is no FDA guidance on the use of Belinostat with respect to specific gender populations.
Race
There is no FDA guidance on the use of Belinostat with respect to specific racial populations.
Renal Impairment
- Approximately 40% of the belinostat dose is excreted renally, primarily as metabolites. Belinostat exposure is not altered in patients with Creatinine Clearance (CLcr) > 39 mL/min. There is insufficient data to recommend a dose of Belinostat in patients with CLcr ≤ 39 mL/min.
Hepatic Impairment
- Belinostat is metabolized in the liver and hepatic impairment is expected to increase exposure to belinostat. Patients with moderate and severe hepatic impairment (total bilirubin >1.5 x upper limit of normal (ULN)) were excluded from clinical trials.
There is insufficient data to recommend a dose of Belinostat in patients with moderate and severe hepatic impairment
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Belinostat in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Belinostat in patients who are immunocompromised.
Administration and Monitoring
Administration
- Intravenous
Monitoring
- Belinostat can cause thrombocytopenia, leukopenia (neutropenia and lymphopenia), and/or anemia; monitor blood counts weekly during treatment, and modify dosage as necessary.
IV Compatibility
There is limited information regarding IV Compatibility of Belinostat in the drug label.
Overdosage
- No specific information is available on the treatment of overdosage of Belinostat . There is no antidote for Belinostat and it is not known if Belinostat is dialyzable. If an overdose occurs, general supportive measures should be instituted as deemed necessary by the treating physician. The elimination half-life of belinostat is 1.1 hours
Pharmacology
Mechanism of Action
- Belinostat is a histone deacetylase (HDAC) inhibitor. HDACs catalyze the removal of acetyl groups from the lysine residues of histones and some non-histone proteins. In vitro, belinostat caused the accumulation of acetylated histones and other proteins, inducing cell cycle arrest and/or apoptosis of some transformed cells. Belinostat shows preferential cytotoxicity towards tumor cells compared to normal cells. Belinostat inhibited the enzymatic activity of histone deacetylases at nanomolar concentrations (<250 nM).
Structure
- Belinostat is a histone deacetylase inhibitor with a sulfonamide-hydroxamide structure. The chemical name of belinostat is (2E)-N-hydroxy-3-[3-(phenylsulfamoyl)phenyl]prop-2-enamide. The structural formula is as follows:

The molecular formula is C15H14N2O4S and the molecular weight is 318.35 g/mol.
- Belinostat is a white to off-white powder. It is slightly soluble in distilled water (0.14 mg/mL) and polyethylene glycol 400 (about 1.5 mg/mL), and is freely soluble in ethanol (> 200 mg/mL). The pKa values are 7.87 and 8.71 by potentiometry and 7.86 and 8.59 by UV.
- Belinostat (belinostat) for injection is supplied as a sterile lyophilized yellow powder containing 500 mg belinostat as the active ingredient. Each vial also contains 1000 mg L-Arginine, USP as an inactive ingredient. The drug product is supplied in a single-use 30 mL clear glass vial with a coated stopper and aluminum crimp seal with “flip-off” cap. Belinostat is intended for intravenous administration after reconstitution with 9 mL Sterile Water for injection, and the reconstituted solution is further diluted with 250 mL of sterile 0.9% Sodium Chloride injection prior to infusion
Pharmacodynamics
Cardiac Electrophysiology
- Multiple clinical trials have been conducted with Belinostat , in many of which ECG data were collected and analyzed by a central laboratory. Analysis of clinical ECG and belinostat plasma concentration data demonstrated no meaningful effect of Belinostat on cardiac repolarization. None of the trials showed any clinically relevant changes caused by Belinostat on heart rate, PR duration or QRS duration as measures of autonomic state, atrio-ventricular conduction or depolarization; there were no cases of Torsades de Pointes.
Pharmacokinetics
- The pharmacokinetic characteristics of belinostat were analyzed from pooled data from phase 1/2 clinical studies that used doses of belinostat ranging from 150 to 1200 mg/m2. The total mean plasma clearance and elimination half-life were 1240 mL/min and 1.1 hours, respectively. The total clearance approximates average hepatic blood flow (1500 mL/min), suggesting high hepatic extraction (clearance being flow dependent).
Distribution
- The mean belinostat volume of distribution approaches total body water, indicating that belinostat has limited body tissue distribution. In vitro plasma studies have shown that between 92.9% and 95.8% of belinostat is bound to protein in an equilibrium dialysis assay, and was independent of belinostat plasma concentrations from 500 to 25,000 ng/mL.
Metabolism
- Belinostat is primarily metabolized by hepatic UGT1A1. Strong UGT1A1 inhibitors are expected to increase exposure to belinostat. Belinostat also undergoes hepatic metabolism by CYP2A6, CYP2C9, and CYP3A4 enzymes to form belinostat amide and belinostat acid. The enzymes responsible for the formation of methyl belinostat and 3-(anilinosulfonyl)-benzenecarboxylic acid, (3-ASBA) are not known.
Excretion
- Belinostat is eliminated predominantly through metabolism with less than 2% of the dose recovered unchanged in urine. All major human metabolites (methyl belinostat, belinostat amide, belinostat acid, belinostat glucuronide, and 3-ASBA) are generally excreted in urine within the first 24 hours after dose administration. Metabolites 3-ASBA and belinostat glucuronide represented the highest fractions of the belinostat dose excreted in urine (4.61% and 30.5%, respectively).
Drug-Drug Interactions
- In vitro studies showed belinostat and its metabolites (including belinostat glucuronide, belinostat amide, methyl belinostat) inhibited metabolic activities of CYP2C8 and CYP2C9. Other metabolites (3-ASBA and belinostat acid) inhibited CYP2C8.
- In cancer patients, co-administration of Belinostat (1,000 mg/m2) and warfarin (5 mg), a known CYP2C9 substrate, did not increase the AUC or Cmax of either R- or S-warfarin.
- Belinostat is likely a glycoprotein (P-gp) substrate but is unlikely to inhibit P-gp.
Pharmacogenomics
- UGT1A1 activity is reduced in individuals with genetic polymorphisms that lead to reduced enzyme activity such as the UGT1A1*28 polymorphism. Approximately 20% of the black population, 10% of the white population, and 2% of the Asian population are homozygous for the UGT1A1*28 allele. Additional reduced function alleles may be more prevalent in specific populations.
- Because belinostat is primarily (80 -90%) metabolized by UGT1A1, the clearance of belinostat could be decreased in patients with reduced UGT1A1 activity (e.g., patients with UGT1A1*28 allele). Reduce the starting dose of Belinostat to 750 mg/m2 in patients known to be homozygous for the UGT1A1*28 allele to minimize dose limiting toxicities.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Carcinogenicity studies have not been performed with belinostat.
- Belinostat was genotoxic in a bacterial reverse mutation test (Ames assay), an in vitro mouse lymphoma cell mutagenesis assay, and an in vivo rat micronucleus assay.
- Belinostat may impair male fertility. Fertility studies using belinostat were not conducted. However, belinostat effects on male reproductive organs observed during the 24-week repeat-dose dog toxicology study included reduced organ weights of the testes/epididymides that correlated with a delay in testicular maturation
Clinical Studies
Relapsed or Refractory Peripheral T-cell Lymphoma (PTCL)
- In an open-label, single-arm, non-randomized international trial conducted at 62 centers, 129 patients with relapsed or refractory PTCL were treated with Belinostat 1,000 mg/m2 administered over 30 minutes via IV infusion once daily on Days 1-5 of a 21-day cycle. There were 120 patients who had histologically confirmed PTCL by central review evaluable for efficacy. Patients were treated with repeat cycles every three weeks until disease progression or unacceptable toxicity.
- The primary efficacy endpoint was response rate (complete response and partial response) as assessed by an independent review committee (IRC) using the International Workshop Criteria (IWC) (Cheson 2007). The key secondary efficacy endpoint was duration of response. Response assessments were evaluated every 6 weeks for the first 12 months and then every 12 weeks until 2 years from the start of study treatment. Duration of response was measured from the first day of documented response to disease progression or death. Response and progression of disease were evaluated by the IRC using the IWC.
- Table 3 summarizes the baseline demographic and disease characteristics of the study population, who were evaluable for efficacy.
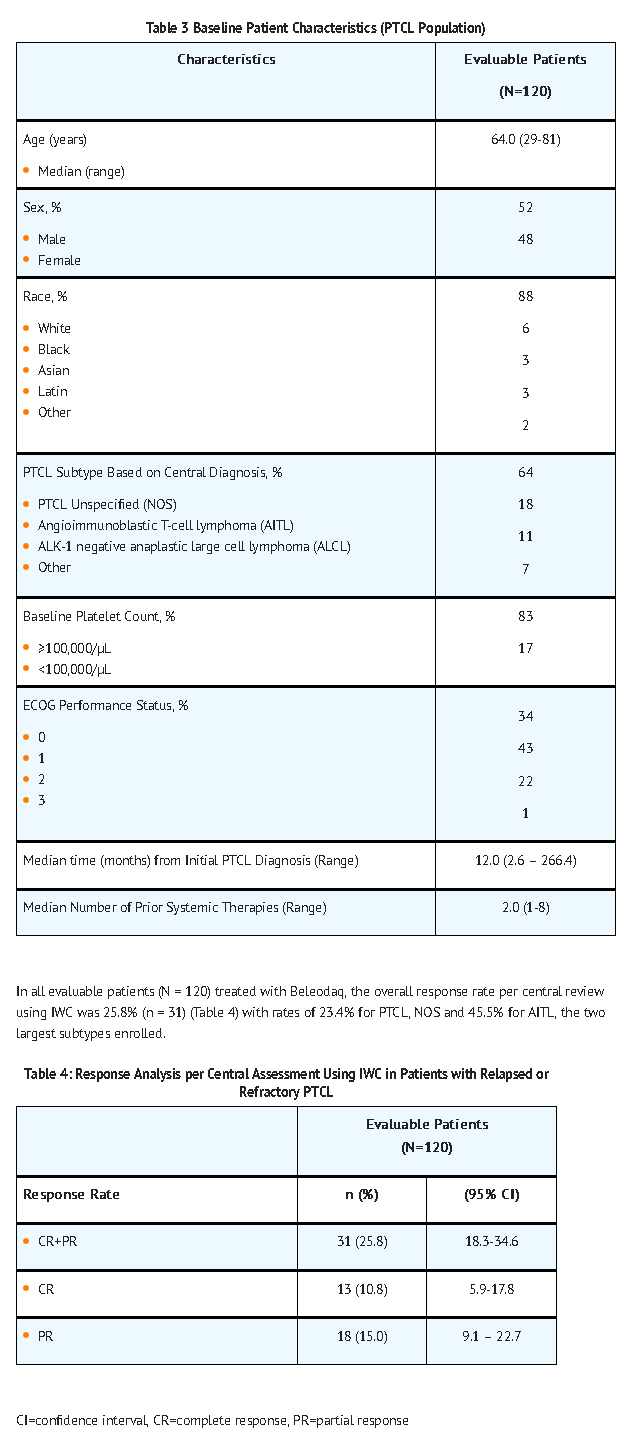
- The median duration of response based on the first date of response to disease progression or death was 8.4 months (95% CI: 4.5 – 29.4). Of the responders, the median time to response was 5.6 weeks (range 4.3 - 50.4 weeks). Nine patients (7.5%) were able to proceed to a stem cell transplant after treatment with Belinostat .
How Supplied
How Supplied
- Belinostat (belinostat) for injection is supplied in single vial cartons; each 30 mL clear vial contains sterile, lyophilized powder equivalent to 500 mg belinostat.
- NDC 68152-108-09: Individual carton of Belinostat 30 mL single-use vial containing 500 mg belinostat.
Storage
- Store Belinostat (belinostat) for injection at room temperature 20°C to 25°C (68°C to 77°F). Excursions are permitted between 15°C and 30°C (59°F and 86°F). Retain in original package until use. .
- Belinostat is a cytotoxic drug. Follow special handling and disposal procedures
Images
Drug Images
{{#ask: Page Name::Belinostat |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Belinostat |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Physicians should discuss the FDA approved Patient Information Leaflet with patients prior to treatment with Belinostat . Instruct patients to read the Patient Information Leaflet carefully.
- Advise the patient or the caregiver to read the FDA-approved patient labeling (Patient Information).
- Advise patients or their caregivers:
- To report symptoms of nausea, vomiting and diarrhea so that appropriate antiemetic and antidiarrheal medications can be administered
- To report any symptoms of thrombocytopenia, leukopenia (neutropenia and lymphopenia), and anemia .
- To immediately report symptoms of infection (e.g., pyrexia) .
- Of the potential risk to the fetus and for women to avoid pregnancy while receiving Belinostat .
- To understand the importance of monitoring liver function test abnormalities and to immediately report potential symptoms of liver injury
Precautions with Alcohol
- Alcohol-Belinostat interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Belinostat ®
Look-Alike Drug Names
- A® — B®
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Belinostat
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Belinostat |Label Name=Belinostat05.png
}}
{{#subobject:
|Label Page=Belinostat |Label Name=Belinostat06.png
}}