Basal cell carcinoma medical therapy: Difference between revisions
| (8 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Basal cell carcinoma}} | {{Basal cell carcinoma}} | ||
{{CMG}} {{AE}} Saarah T. Alkhairy, M.D. | {{CMG}} {{AE}}{{M.N}},Saarah T. Alkhairy, M.D. | ||
==Overview== | ==Overview== | ||
After the suspicious lesion is evaluated, the medical therapy is divided | After the suspicious [[lesion]] is evaluated, the [[medical]] [[therapy]] is divided based on low-risk and high-risk basal cell carcinoma [[patients]]. [[Medical]] [[therapy]] consists of [[topical]] and [[systemic therapy]]. Among [[topical]] [[therapy]] [[imiquimod]], [[photodynamic therapy]], [[5-fluorouracil]] are included. [[Systemic therapy]] consists of [[Sonic hedgehog|sonic hedgehog pathway]] inhibitors like [[vismodegib]], [[sonidegib]]. | ||
==Basal Cell Carcinoma Medical Therapy== | ==Basal Cell Carcinoma Medical Therapy== | ||
Once the suspicious [[lesion]] is evaluated, the medical therapy is based upon the low-risk and high-risk basal cell carcinoma patients. | Once the suspicious [[lesion]] is evaluated, the [[medical]] [[therapy]] is based upon the low-risk and high-risk basal cell carcinoma [[patients]]. | ||
The table below summarizes the characteristics in low-risk and high-risk [[lesions]]<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | The table below summarizes the characteristics in low-risk and high-risk [[lesions]]<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | ||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | {| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | ||
| align="center" style="background:# | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''H&P'''}} | ||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Low risk'''}} | |||
| align="center" style="background:# | | align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''high risk'''}} | ||
| align="center" style="background:# | |||
|- | |- | ||
| Line 31: | Line 29: | ||
|- | |- | ||
| '''Immunosuppression'''||(-)||(+) | | '''[[Immunosuppression]]'''||(-)||(+) | ||
|- | |- | ||
| '''Site of prior radiation therapy'''||(-)||(+) | | '''Site of prior [[radiation therapy]]'''||(-)||(+) | ||
|- | |- | ||
| '''Subtype'''||[[Nodular]], [[superficial]]||Aggressive growth pattern | | '''Subtype'''||[[Nodular]], [[superficial]]||Aggressive [[growth]] pattern | ||
|- | |- | ||
| Line 51: | Line 49: | ||
'''Area M''' = [[cheeks]], [[forehead]], [[scalp]], [[neck]], and pre-[[tibial]] area | '''Area M''' = [[cheeks]], [[forehead]], [[scalp]], [[neck]], and pre-[[tibial]] area | ||
'''Area L''' = [[trunk]] and [[extremities]] (excluding pre-tibial area, [[hands]], [[feet]], [[nail]] units, and ankles) | '''Area L''' = [[trunk]] and [[extremities]] (excluding pre-[[tibial]] area, [[hands]], [[feet]], [[nail]] units, and ankles) | ||
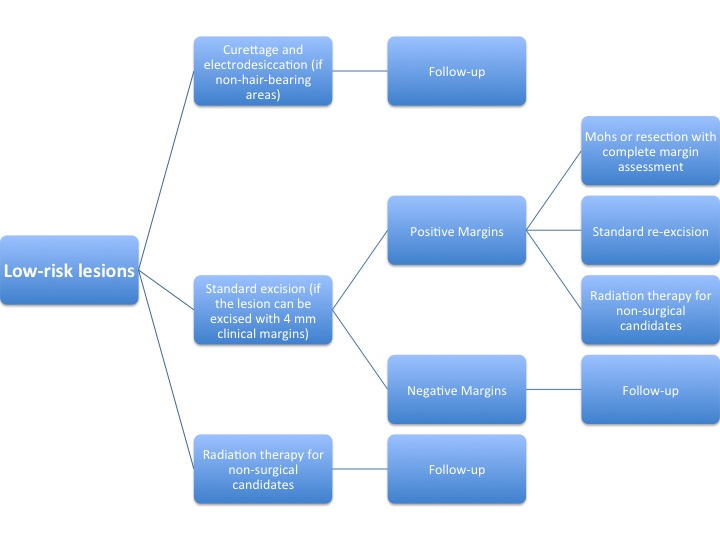
The algorithm below demonstrates a treatment protocol for '''low-risk''' lesions<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | The [[Algorithm (medical)|algorithm]] below demonstrates a treatment [[Protocol (natural sciences)|protocol]] for '''low-risk''' [[lesions]]<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | ||
[[Image:Low Risk Basal Cell.jpg|800px]] | [[Image:Low Risk Basal Cell.jpg|800px]] | ||
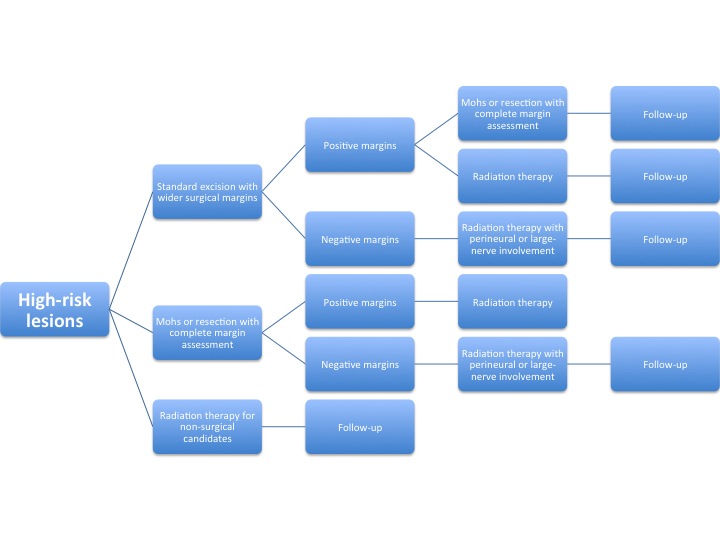
The algorithm below demonstrates a treatment protocol for '''high-risk''' lesions<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | The [[algorithm]] below demonstrates a treatment [[Protocol (natural sciences)|protocol]] for '''high-risk''' [[lesions]]<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | ||
[[Image:High Risk Basal Cell.jpg|800px]] | [[Image:High Risk Basal Cell.jpg|800px]] | ||
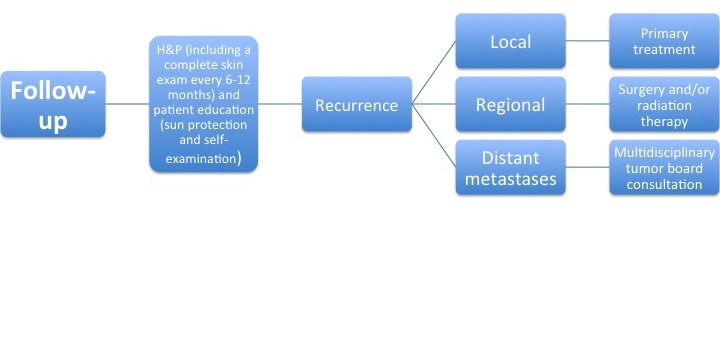
After the primary treatment, a follow-up is performed to evaluate for recurrence of the tumor. | After the primary treatment, a follow-up is performed to evaluate for recurrence of the [[tumor]]. | ||
The algorithm below demonstrates a follow-up protocol<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | The [[algorithm]] below demonstrates a follow-up [[Protocol (natural sciences)|protocol]]<ref>http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf</ref>. | ||
[[Image:Followup Basal Cell.jpg|800px]] | [[Image:Followup Basal Cell.jpg|800px]] | ||
| Line 72: | Line 70: | ||
*Systemic | *Systemic | ||
'''Topical therapy''' | '''Topical therapy''' | ||
* | *[[Imiquimod]] | ||
**It is an [[immunomodulatory]] agent that binds to [[Toll-like receptors|toll-like receptor]] 7 and induces the release of pro-inflammatory [[cytokines]] including [[IFN-α|IFN]]-alpha, [[TNF-alpha]] and [[IL-12]]. | **It is an [[immunomodulatory]] agent that binds to [[Toll-like receptors|toll-like receptor]] 7 and induces the release of pro-[[inflammatory]] [[cytokines]] including [[IFN-α|IFN]]-alpha, [[TNF-alpha]] and [[IL-12]]. | ||
**It is approved for treatment of small [[superficial]] | **It is approved for treatment of small [[superficial]] basal cell carcinoma and is applied nightly five times a week for six weeks. | ||
**The complete cure rate was around 80%. | **The complete [[cure]] rate was around 80%. | ||
*[[Photodynamic therapy]] | *[[Photodynamic therapy]] | ||
**The other available option for | **The other available option for basal cell carcinoma is [[photodynamic therapy]] (PDT) with [[Levulinic acid|5-amino levulinic acid]](MAL) or with its methyl [[Esters|ester]] plus red light. | ||
**The MAL cream is applied to the tumor and covered with an occlusive dressing for three hours. | **The MAL [[Cream (pharmaceutical)|cream]] is applied to the [[tumor]] and covered with an [[Occlusive dressing|occlusive]] [[Dressing (medical)|dressing]] for three hours. | ||
**The tumor cells then form increasing amounts of protoporphyrin IX, which is stimulated by irradiation with red light to form reactive oxygen species which are in turn cytotoxic. | **The [[Tumor cell|tumor cells]] then form increasing amounts of [[protoporphyrin IX]], which is stimulated by [[irradiation]] with red [[light]] to form [[reactive oxygen species]] which are in turn [[cytotoxic.]] | ||
**It should be repeated after 1–4 weeks. | **It should be repeated after 1–4 weeks. | ||
**The achieved complete remission is expected to be 92%. | **The achieved complete [[remission]] is expected to be 92%. | ||
**The main disadvantages of | **The main disadvantages of [[photodynamic therapy]] are the [[pain]] during the [[irradiation]] and the local [[inflammatory]] [[reaction]] ([[erythema]], erosions, [[pustules]], and crusts). | ||
*5- | *[[Fluorouracil (topical)|5-fluorouracil]] | ||
**It is a cytostatic agent which is available as a 5% prescription cream that is designed to be applied twice daily for 3–12 weeks until erosions develop. | **It is a [[cytostatic]] agent which is available as a 5% [[prescription]] [[Cream (pharmaceutical)|cream]] that is designed to be applied twice daily for 3–12 weeks until erosions develop. | ||
'''Systemic therapy''' | '''Systemic therapy''' | ||
* | *[[Sonic hedgehog|Sonic hedgehog pathway]] inhibitors([[vismodegib]], [[sonidegib]]) | ||
**They are markedly teratogenic and embryotoxic. | **They are markedly [[teratogenic]] and embryotoxic. | ||
**The commonest adverse effects of vismodegib include muscle cramps, hair loss, taste disturbances and weight loss. | **The commonest [[adverse effects]] of [[vismodegib]] include [[muscle cramps]], [[hair loss]], [[Taste alteration|taste disturbances]] and [[weight loss]]. | ||
'''Cryotherapy''' | '''Cryotherapy''' | ||
*Small and superficial | *Small and [[superficial]] basal cell carcinoma is occasionally still treated with [[liquid nitrogen]] (–196°C) either with direct contact or using a [[Spray-on skin|spray]]. | ||
*The wounds may heal with either hypopigmentation or scarring so making it a major disadvantage. | *The [[wounds]] may [[Healing|heal]] with either [[hypopigmentation]] or [[scarring]] so making it a major disadvantage. | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[Category:Up-To-Date]] | |||
[[Category:Oncology]] | [[Category:Oncology]] | ||
[[Category:Medicine]] | [[Category:Medicine]] | ||
[[Category:Dermatology]] | [[Category:Dermatology]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
Latest revision as of 17:09, 4 April 2019
|
Basal cell carcinoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Basal cell carcinoma medical therapy On the Web |
|
American Roentgen Ray Society Images of Basal cell carcinoma medical therapy |
|
Risk calculators and risk factors for Basal cell carcinoma medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maneesha Nandimandalam, M.B.B.S.[2],Saarah T. Alkhairy, M.D.
Overview
After the suspicious lesion is evaluated, the medical therapy is divided based on low-risk and high-risk basal cell carcinoma patients. Medical therapy consists of topical and systemic therapy. Among topical therapy imiquimod, photodynamic therapy, 5-fluorouracil are included. Systemic therapy consists of sonic hedgehog pathway inhibitors like vismodegib, sonidegib.
Basal Cell Carcinoma Medical Therapy
Once the suspicious lesion is evaluated, the medical therapy is based upon the low-risk and high-risk basal cell carcinoma patients.
The table below summarizes the characteristics in low-risk and high-risk lesions[1].
| H&P | Low risk | high risk |
| Location/size | Area L < 20 mm; Area M < 10 mm; Area H < 6 mm | Area L ≥ 20 mm; Area M ≥ 10 mm; Area H ≥ 6 mm |
| Borders | Well defined | Poorly defined |
| Primary vs. recurrent | Primary | Recurrent |
| Immunosuppression | (-) | (+) |
| Site of prior radiation therapy | (-) | (+) |
| Subtype | Nodular, superficial | Aggressive growth pattern |
| Perineural involvement | (-) | (+) |
Area H = “mask areas” of face (central face, eyelids, eyebrows, periorbital, nose, lips [cutaneous and vermilion], chin, mandible, preauricular and postauricular skin/sulci, temple, ear), genitalia, hands, and feet
Area M = cheeks, forehead, scalp, neck, and pre-tibial area
Area L = trunk and extremities (excluding pre-tibial area, hands, feet, nail units, and ankles)
The algorithm below demonstrates a treatment protocol for low-risk lesions[2].
The algorithm below demonstrates a treatment protocol for high-risk lesions[3].
After the primary treatment, a follow-up is performed to evaluate for recurrence of the tumor.
The algorithm below demonstrates a follow-up protocol[4].
The medical therapy for basal cell carcinoma is divided into[5][6]:
- Toipcal
- Systemic
Topical therapy
- Imiquimod
- It is an immunomodulatory agent that binds to toll-like receptor 7 and induces the release of pro-inflammatory cytokines including IFN-alpha, TNF-alpha and IL-12.
- It is approved for treatment of small superficial basal cell carcinoma and is applied nightly five times a week for six weeks.
- The complete cure rate was around 80%.
- Photodynamic therapy
- The other available option for basal cell carcinoma is photodynamic therapy (PDT) with 5-amino levulinic acid(MAL) or with its methyl ester plus red light.
- The MAL cream is applied to the tumor and covered with an occlusive dressing for three hours.
- The tumor cells then form increasing amounts of protoporphyrin IX, which is stimulated by irradiation with red light to form reactive oxygen species which are in turn cytotoxic.
- It should be repeated after 1–4 weeks.
- The achieved complete remission is expected to be 92%.
- The main disadvantages of photodynamic therapy are the pain during the irradiation and the local inflammatory reaction (erythema, erosions, pustules, and crusts).
- 5-fluorouracil
- It is a cytostatic agent which is available as a 5% prescription cream that is designed to be applied twice daily for 3–12 weeks until erosions develop.
Systemic therapy
- Sonic hedgehog pathway inhibitors(vismodegib, sonidegib)
- They are markedly teratogenic and embryotoxic.
- The commonest adverse effects of vismodegib include muscle cramps, hair loss, taste disturbances and weight loss.
Cryotherapy
- Small and superficial basal cell carcinoma is occasionally still treated with liquid nitrogen (–196°C) either with direct contact or using a spray.
- The wounds may heal with either hypopigmentation or scarring so making it a major disadvantage.
References
- ↑ http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf
- ↑ http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf
- ↑ http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf
- ↑ http://www.nccn.org/professionals/physician_gls/PDF/nmsc.pdf
- ↑ Berking C, Hauschild A, Kölbl O, Mast G, Gutzmer R (May 2014). "Basal cell carcinoma-treatments for the commonest skin cancer". Dtsch Arztebl Int. 111 (22): 389–95. doi:10.3238/arztebl.2014.0389. PMID 24980564.
- ↑ Wong CS, Strange RC, Lear JT (October 2003). "Basal cell carcinoma". BMJ. 327 (7418): 794–8. doi:10.1136/bmj.327.7418.794. PMC 214105. PMID 14525881.