Barrett's esophagus differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Amresh Kumar (talk | contribs) |
Amresh Kumar (talk | contribs) No edit summary |
||
| Line 18: | Line 18: | ||
===Preferred Table=== | ===Preferred Table=== | ||
{| class="wikitable" | {| class="wikitable" | ||
! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Disease | ! rowspan="3" align="center" style="background:#4479BA; color: #FFFFFF;" |Disease | ||
| Line 62: | Line 63: | ||
| | | | ||
* [[Biopsy]] | * [[Biopsy]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Systemic sclerosis]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Systemic sclerosis]] | ||
| Line 216: | Line 97: | ||
| | | | ||
* [[Skin biopsy]] | * [[Skin biopsy]] | ||
|- | |- | ||
| style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Stroke]] | | style="padding: 5px 5px; background: #DCDCDC;" align="center" |[[Stroke]] | ||
| Line 326: | Line 177: | ||
| | | | ||
* 24 hour [[esophageal]] pH monitoring | * 24 hour [[esophageal]] pH monitoring | ||
|} | |} | ||
Revision as of 16:12, 31 January 2018
|
Barrett's Esophagus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Barrett's esophagus differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Barrett's esophagus differential diagnosis |
|
Risk calculators and risk factors for Barrett's esophagus differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amresh Kumar MD [2]
Overview
Barrett's Oesophagus must be differentiated from Esophagitis, Peptic ulcer disease and Esophageal motor disorders.
Differentiating Barrett's Esophagus from other Diseases
- Pills esophagitis
- Eosinophilic esophagitis
- Infectious esophagitis[1]
- GERD[2]
- Peptic ulcer disease
- Esophageal motor disorders
Preferred Table
| Disease | Signs and Symptoms | Barium esophagogram | Endoscopy | Other imaging and laboratory findings | Gold Standard | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Onset | Dysphagia | Weight loss | Heartburn | Other findings | Mental status | |||||||
| Solids | Liquids | Type | ||||||||||
| Esophageal carcinoma |
|
+ | + | Progressive | + | +/- | Normal |
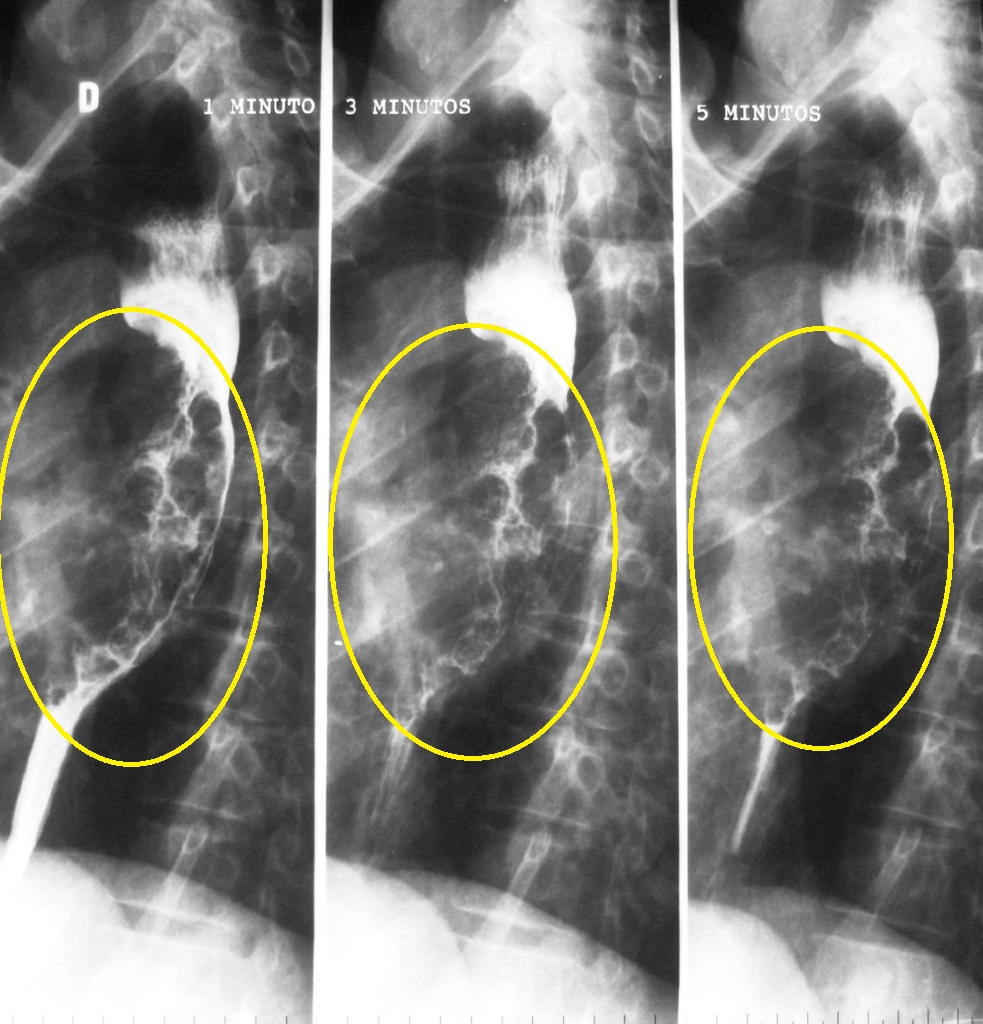 |
{{#ev:youtube|5ucSlgqGAno}}
|
|||
| Systemic sclerosis |
|
+ | + | Progressive | +/- | + |
|
Normal |
|
|
Positive serology for | |
| Stroke |
|
+ | + | Progressive | + | +/- |
|
Impaired |
|
|
||
| Motor disorders |
|
+ | + | Progressive | +/- | Normal |
|
|
|
| ||
| GERD |
|
+ | - | Progressive | +/- | + | Normal |
|
|
| ||
Use if the above table can not be made
| Differential Diagnosis | Similar Features | Differentiating Features |
|---|---|---|
| Differential 1 |
|
|
| Differential 2 |
|
|
| Differential 3 |
|
|
| Differential 4 |
|
|
| Differential 5 |
|
|
References
- ↑ Moayyedi P, Talley NJ (2006). "Gastro-oesophageal reflux disease". Lancet. 367 (9528): 2086–100. doi:10.1016/S0140-6736(06)68932-0. PMID 16798392. Unknown parameter
|month=ignored (help) - ↑ http://www.wrongdiagnosis.com/b/barretts_esophagus/misdiag.htm