B-cell lymphoma pathophysiology
|
B-cell lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
B-cell lymphoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of B-cell lymphoma pathophysiology |
|
Risk calculators and risk factors for B-cell lymphoma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Overview
Pathophysiology
Physiology
The normal physiology of B-cells can be understood as follows:
- Development of mature B-cells include:
- B-cells develop from hematopoietic stem cells originating from bone marrow. B-cell development occurs in the bone marrow through several steps including the ordered rearrangement of [[IGH@|Ig H] and L chain loci (i.e., VDJ recombination), positive selection, and negative selection.[1]
- B-cell surface consists of membrane-bound Ig, complement component receptors, Fc receptors, and B cell-specific cell surface molecules representing by CDs (i.e., CD19, CD20, CD21, etc.).
- Immature (transitional) B-cells migrate from the bone marrow to secondary lymphoid organs (i.e., lymph nodes, spleen) for activation. Activation begins with either T-cell dependent or T-cell independent. T-cell-dependent B-cell activation begins with the binding of the B-cell receptor (BCR) to the T-cell-dependent antigen. T-cell independent B-cell activation begins with BCR crosslinking through polysaccharides or via BCR and toll-like receptor (TLR) costimulation. Following the activation, further maturation steps including germinal center reaction (i.e., clonal expansion, class switch recombination, somatic hypermutation, affinity maturation) occur.[2][1]
- B-cells can be divided into 3 main types include: B1 B-lymphoctes (originates from fetal liver), marginal zone (MZ) B2 B-lymphocyes, and follicular (FO) B2 B-lymphocytes.[3]
- B-cells complete their maturation by differention into memory B cells or antibody-secreting plasma cells.
- Functions of B-cells include:[1]
- Antibody production
- Production of cytokines (i.e. IFN-γ, IL-6, IL-10)
- Lymphoid tissue organogenesis
- Wound healing
- Tumor immunity
- Transplant rejection
- Dentritic cell regulation
- TH1/TH2 cytokine balance
- Antigen presentation
- Co-stimulation
Pathogenesis
It is understood that there are different factors that have important roles in the pathogenesis of B-cell lymphomas including:[4]
- Reciprocal translocations that occur between one of the immunoglobulin loci and proto-oncogene
- Increased expression of B-cell receptor (BCR)
- Increased survival and proliferation of B-cells mediated by antigen binding
- Malignant interaction between B-cells and other cells in tumor microenviroment
Genetics
Chromosomal translocations involving the immunoglobulin heavy locus (IGH@) is a classic cytogenetic abnormality for many B-cell lymphomas, including follicular lymphoma, mantle cell lymphoma, diffuse large B cell lymphoma, MALT lymphoma, lymphoplasmacytoid lymphoma, multiple myeloma, and Burkitt's lymphoma. In these cases, The immunoglobulin heavy locus forms a fusion protein with another protein that has pro-proliferative or anti-apoptotic abilities. The enhancer element of the immunoglobulin heavy locus, which normally functions to make B cells produce massive production of antibodies, now induces massive transcription of the fusion protein, resulting in excessive pro-proliferative or anti-apoptotic effects on the B cells containing the fusion protein. Chromosomal translocations and mutations of tumor suppressor genes that are associated with B-cell lymphomas include:[4]
- Burkitt's lymphoma is characterized by the chromosomal translocations between MYC and either IGH@ or IGL@. Mutations of tumor suppressor genes causing Burkitt lymphoma include TP53 and retinoblastoma-like protein 2.
- Mantle-cell lymphoma is characterized by the chromosomal translocation between cyclin D1 and IGH@. Mutations of tumor suppressor gene ATM, is also associated with mantle-cell lymphoma.
- Follicular lymphoma is characterized by the chromosomal translocation between Bcl-2 and IGH@.
- Diffuse large B cell lymphoma is characterized by the chromosomal translocations of Bcl-2–IGH@, MYC-IGH@, MYC-IGL@, or the chromosomal translocations involving BCL6. Mutations of tumor suppressor genes causing diffuse large B cell lymphoma include CD95, ATM, and TP53.
- The mutation of tumor suppressor gene SOCS1 is associated with primary mediastinal B-cell lymphoma.
- Classical Hodgkin's lymphoma is associated with mutations of tumor suppressor genes including IκBα, IκBe, and CD95.
- Lymphocyte-predominant Hodgkin's lymphoma is characterized by the chromosomal translocations involving BCL6.
- MALT lymphoma is characterized by the chromosomal translocations of API2–MALT1, BCL10–IGH@, MALT1–IGH@, or FOXP1–IGH@. The mutation of tumor suppressor gene CD95 is associated with MALT lymphoma.
- Lymphoplasmacytoid lymphoma is characterized by the chromosomal translocation between PAX5 and IGH@.
- Multiple myeloma is characterized by the chromosomal translocations of cyclin D1–IGH@, FGFR3–IGH@, or MAF–IGH@. The mutation of tumor suppressor gene CD95 is associated with multiple myeloma.
Associated Conditions
Conditions associated with B-cell lymphoma include:[4]
- Viral infections:
- Bacterial infections:
- Autoimmune diseases:
Gross Pathology
There is no gross pathologic finding characteristic of B-cell lymphoma.
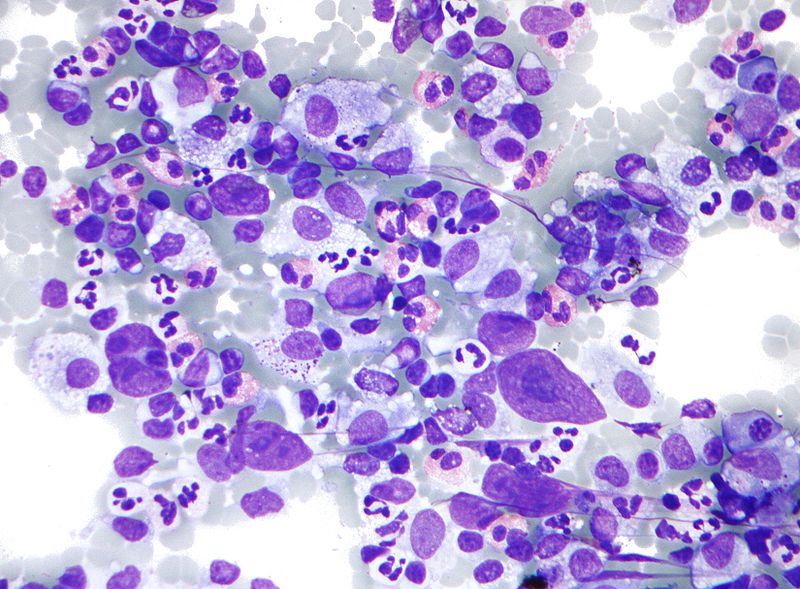
Microscopic Pathology
Below is a microscopic image of a lymph node FNA specimen (Field's stain) of a patient with Hodgkin's lymphoma, a type of B cell lymphoma. The micrograph shows a mixture of cells commonly seen in Hodgkin's lymphoma:
- Eosinophils
- Reed Sternberg cells
- Plasma cells
- Histiocytes
Video
Shown below is a video of diffuse large B cell lymphoma {{#ev:youtube|9gEo7si6jtc}}
References
- ↑ 1.0 1.1 1.2 LeBien TW, Tedder TF (September 2008). "B lymphocytes: how they develop and function". Blood. 112 (5): 1570–80. doi:10.1182/blood-2008-02-078071. PMC 2518873. PMID 18725575.
- ↑ Hess C, Winkler A, Lorenz AK, Holecska V, Blanchard V, Eiglmeier S, Schoen AL, Bitterling J, Stoehr AD, Petzold D, Schommartz T, Mertes MM, Schoen CT, Tiburzy B, Herrmann A, Köhl J, Manz RA, Madaio MP, Berger M, Wardemann H, Ehlers M (September 2013). "T cell-independent B cell activation induces immunosuppressive sialylated IgG antibodies". J Clin Invest. 123 (9): 3788–96. doi:10.1172/JCI65938. PMC 3754242. PMID 23979161.
- ↑ Hoffman W, Lakkis FG, Chalasani G (January 2016). "B Cells, Antibodies, and More". Clin J Am Soc Nephrol. 11 (1): 137–54. doi:10.2215/CJN.09430915. PMC 4702236. PMID 26700440.
- ↑ 4.0 4.1 4.2 Küppers R (April 2005). "Mechanisms of B-cell lymphoma pathogenesis". Nat Rev Cancer. 5 (4): 251–62. doi:10.1038/nrc1589. PMID 15803153.