B-cell lymphoma overview
|
B-cell lymphoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
B-cell lymphoma overview On the Web |
|
American Roentgen Ray Society Images of B-cell lymphoma overview |
|
Risk calculators and risk factors for B-cell lymphoma overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Shivali Marketkar, M.B.B.S. [2]
Overview
B-cell lymphomas make up most (about 85%) of the non-Hodgkin lymphomas (NHL) in the United States. It develops more frequently in immunocompromised individuals (such as those with AIDS.)
Classification
B-cell lymphomas include both Hodgkin's lymphomas and most Non-Hodgkins lymphomas. They are typically divided into low and high grade, typically corresponding to indolent (slow-growing) lymphomas and aggressive lymphomas, respectively. . The most commonly used classification system is the WHO classification, a convergence of more than one, older classification systems.
Most common
Five account for nearly three out of four patients with non-Hodgkin lymphoma:[1]
- Diffuse large B cell lymphoma
- Follicular lymphoma
- Mucosa-Associated Lymphatic Tissue lymphoma (MALT)
- Small cell lymphocytic lymphoma (overlaps with Chronic lymphocytic leukemia)
- Mantle cell lymphoma (MCL)
Rare
The remaining forms are much less common:[1]
- Burkitt lymphoma
- Mediastinal large B cell lymphoma
- Waldenström macroglobulinemia
- Nodal marginal zone B cell lymphoma (NMZL)
- Splenic marginal zone lymphoma (SMZL)
- Extranodal marginal zone B cell lymphoma
- Intravascular large B cell lymphoma
- Primary effusion lymphoma
- Lymphomatoid granulomatosis
- T cell/histiocyte-rich large B-cell lymphoma
- Primary central nervous system lymphoma
- Primary cutaneous diffuse large B-cell lymphoma, leg type (Primary cutaneous DLBCL, leg type)
- EBV positive diffuse large B-cell lymphoma of the elderly
- Diffuse large B-cell lymphoma associated with inflammation
- Intravascular large B-cell lymphoma
- ALK-positive large B-cell lymphoma
- Plasmablastic lymphoma
- Large B-cell lymphoma arising in HHV8-associated multicentric Castleman's disease
- B-cell lymphoma, unclassifiable with features intermediate between diffuse large B-cell lymphoma and Burkitt lymphoma
- B-cell lymphoma, unclassifiable with features intermediate between diffuse large B-cell lymphoma and classical Hodgkin lymphoma
Others
Additionally, some researchers separate out lymphomas that appear result from other immune system disorders, such as AIDS-related lymphoma. Classic Hodgkin's lymphoma and nodular lymphocyte predominant Hodgkin's lymphoma are now considered forms of B-cell lymphoma.[2]
Pathophysiology
Genetics
Chromosomal translocations involving the immunoglobulin heavy locus (IGH@) is a classic cytogenetic abnormality for many B-cell lymphomas, including follicular lymphoma, mantle cell lymphoma and Burkitt's lymphoma. In these cases, The immunoglobulin heavy locus forms a fusion protein with another protein that has pro-proliferative or anti-apoptotic abilities. The enhancer element of the immunoglobulin heavy locus, which normally functions to make B cells produce massive production of antibodies, now induces massive transcription of the fusion protein, resulting in excessive pro-proliferative or anti-apoptotic effects on the B cells containing the fusion protein. In Burkitt's lymphoma and mantle cell lymphoma, the other protein in the fusion is c-myc (on chromosome 8) and cyclin D1[3] (on chromosome 11), respectively, which gives the fusion protein pro-proliferative ability. In follicular lymphoma, the fused protein is Bcl-2 (on chromosome 18), which gives the fusion protein anti-apoptotic abilities.
Microscopic Pathology
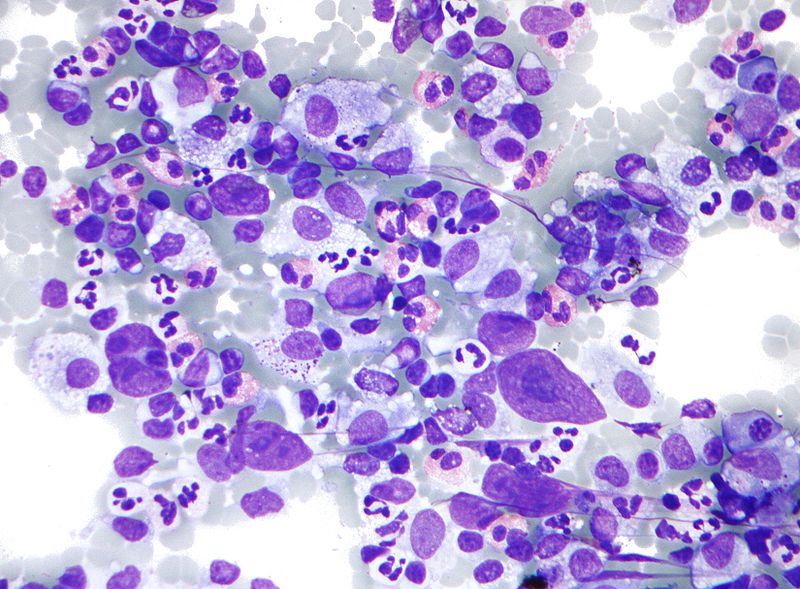
Shown below is a microscopic image of Hodgkins Lymphoma which is a type of B cell lymphoma.Lymph node FNA specimen(Field's stain) The micrograph shows a mixture of cells commonly seen in Hodgkins lymphoma:
- Eosinophils
- Reed Sternberg cells
- Plasma cells
- Histiocytes
Treatment
Medical Therapy
- Treatment includes radiation and chemotherapy.
- Early-stage indolent B-cell lymphomas can often be treated with radiation alone, with long-term non-recurrence.
- Early-stage aggressive disease is treated with chemotherapy and often radiation, with a 70-90% cure rate.[4]
- Late-stage indolent lymphomas are sometimes left untreated and monitored until they progress.
- Late-stage aggressive disease is treated with chemotherapy, with cure rates of over 70%.[4]
References
- ↑ 1.0 1.1 "The Lymphomas" (PDF). The Leukemia & Lymphoma Society. May 2006. pp. p. 12. Retrieved 2008-04-07.
- ↑ "HMDS: Hodgkin's Lymphoma". Archived from the original on 4 March 2009. Retrieved 2009-02-01.
- ↑ Li JY, Gaillard F, Moreau A; et al. (1999). "Detection of translocation t(11;14)(q13;q32) in mantle cell lymphoma by fluorescence in situ hybridization". Am. J. Pathol. 154 (5): 1449–52. doi:10.1016/S0002-9440(10)65399-0. PMC 1866594. PMID 10329598. Unknown parameter
|month=ignored (help) - ↑ 4.0 4.1 Merck Manual home edition, Non-Hodgkin Lymphomas