Atrial septal defect
| Atrial septal defect | ||
 | ||
|---|---|---|
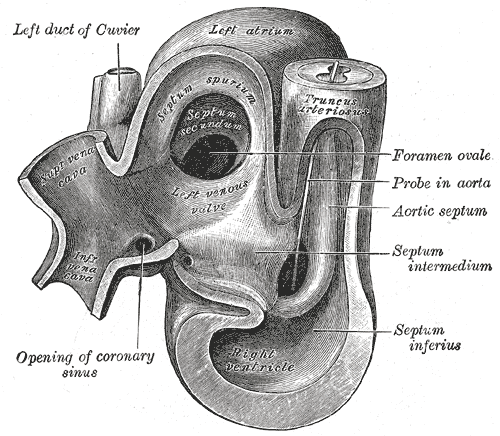
| Heart of human embryo of about thirty-five days | ||
| ICD-10 | Q21.1 | |
| ICD-9 | 745.5-745.6 | |
| OMIM | 108800 | |
| DiseasesDB | 1089 | |
| eMedicine | med/3519 | |
| MeSH | C14.240.400.560.375 | |
| Cardiology Network |
 Discuss Atrial septal defect further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editors-In-Chief: Claudia Hochberg, M.D.; C. Michael Gibson, M.S., M.D. [1] Phone:617-525-6884
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Keri Shafer, M.D. [3]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Embryology
Pathophysiology
Epidemiology
Genetic
Types of atrial septal defects
Ostium primum atrial septal defect | Ostum secundum atrial septal defect | Patent foramen ovale | Sinus venosus atrial septal defect | Common or single atrium
Diagnosis
Physical examination | Auscultation of the heart | Chest X-ray | Electrocardiography | Echocardiography | Trans-cranial doppler ultrasound | MRI
Treatment
Evaluation prior to correction
Prior to correction of an ASD, an evaluation to determine if pulmonary hypertension is present and whether it is reversible. Closure of an ASD may be recommended for prevention purposes, to avoid such a complication in the first place. Pulmonary Hypertension is not always present in adults that are diagnosed with an ASD in adulthood.
If there is a suspicion that pulmonary hypertension is present, the evaluation may include a right heart catheterization. This involves placing a catheter in the venous system of the heart and measuring pressures and oxygen saturations in the SVC, IVC, right atrium, right ventricle, pulmonary artery, and in the wedge position. Individuals with a pulmonary vascular resistance (PVR) of less than 7 wood units show regression of symptoms (including NYHA functional class). On the other hand, individuals with a PVR of greater than 15 wood units have increased mortality associated with closure of the ASD.
If the pulmonary arterial pressure is more than 2/3 the systemic systolic pressure, there should be a net left-to-right shunt of at least 1.5:1 or evidence of reversibility of the shunt when given pulmonary artery vasodilators prior to surgery. If Eisenmenger's physiology has developed, it must be demonstrated that the right-to-left shunt is reversible with pulmonary artery vasodilators prior to surgery.
Surgical ASD closure
Surgical closure of an ASD involves opening up at least one atrium and closing the defect with a patch under direct visualization.
Percutaneous ASD closure
Percutaneous closure of an ASD is currently only indicated for the closure of ostium secundum ASDs with a sufficient rim of tissue around the septal defect so that the closure device does not impinge upon the SVC, IVC, or the tricuspid or mitral valves. The Amplatzer Septal Occluder is commonly used to close ASD's. The ASO consists of two self-expandable round discs connected to each other with a 4-mm waist, made up of 0.004–0.005´´ nitinol wire mesh filled with Dacron fabric. Implantation of the device is relatively easy. The prevalence of residual defect is low. The disadvantages are a thick profile of the device and concern related to a large amount of nitinol (a nickel-titanium compound) in the device and consequent potential for nickel toxicity.
Percutaneous closure is the method of choice in most centers.[1]
Associated conditions
Due to the communication between the atria that occurs in ASD's, disease entities or complications from the condition, are possible.
Decompression sickness
ASDs, and particularly PFOs, are a predisposing risk factor for decompression sickness in divers because a proportion of venous blood carrying inert gases, such as helium or nitrogen does not pass through the lungs.[2][3] The only way to release the excess inert gases from the body is to pass the blood carrying the inert gases through the lungs to be exhaled. If some of the inert gas-laden blood passes through the PFO, it avoids the lungs and the inert gas is more likely to form large bubbles in the arterial blood stream causing decompression sickness.
Paradoxical emboli
Venous thrombi (clots in the veins) are quite common. Embolization (dislodgement of thrombi) normally go to the lung and cause pulmonary emboli. In an individual with ASD, these emboli can potentially enter the arterial system. This can cause any phenomenon that is attributed to acute loss of blood to a portion of the body, including cerebrovascular accident (stroke), infarction of the spleen or intestines, or even a distal extremity (i.e.: finger or toe).
This is known as a paradoxical embolus because the clot material paradoxically enters the arterial system instead of going to the lungs.
Migraine
Some recent research has suggested that a proportion of cases of migraine may be caused by patent foramen ovale. While the exact mechanism remains unclear, closure of a PFO can reduce symptoms in certain cases.[4][5] This remains controversial. 20% of the general population have a PFO, which for the most part, is asymptomatic. 20% of the female population have migraines. And, the placebo effect in migraine typically averages around 40%. The high frequency of these facts makes statistically significant relationships between PFO and migraine difficult (i.e., the relationship may just be chance or coincidence).
See also
- Atrioventricular septal defect
- Cardiac output
- Congenital heart disease
- Heart sounds
- Pulmonary hypertension
- Vascular resistance
- Ventricular septal defect
References
- ↑ Bjørnstad P (2006). "Is interventional closure the current treatment of choice for selected patients with deficient atrial septation?". Cardiol Young. 16 (1): 3–10. PMID 16454871.
- ↑ Lier H, Schroeder S, Hering R (2004). "[Patent foramen ovale: an underrated risk for divers?]". Dtsch Med Wochenschr. 129 (1–2): 27–30. PMID 14703578.
- ↑ Saary M, Gray G (2001). "A review of the relationship between patent foramen ovale and type II decompression sickness". Aviat Space Environ Med. 72 (12): 1113–20. PMID 11763113.
- ↑ Adams H (2004). "Patent foramen ovale: paradoxical embolism and paradoxical data". Mayo Clin Proc. 79 (1): 15–20. PMID 14708944.
- ↑ Azarbal B, Tobis J, Suh W, Chan V, Dao C, Gaster R (2005). "Association of interatrial shunts and migraine headaches: impact of transcatheter closure". J Am Coll Cardiol. 45 (4): 489–92. PMID 15708691.
External links
- Atrial Septal Defect information from Seattle Children's Hospital Heart Center
- Pediatric Heart Surgery
- The Congenital Heart Surgery Video Project
- Pediatric Cardiac Surgery: Atrial Septal Defect Repair