Amaurosis fugax
| Amaurosis fugax | |
 | |
|---|---|
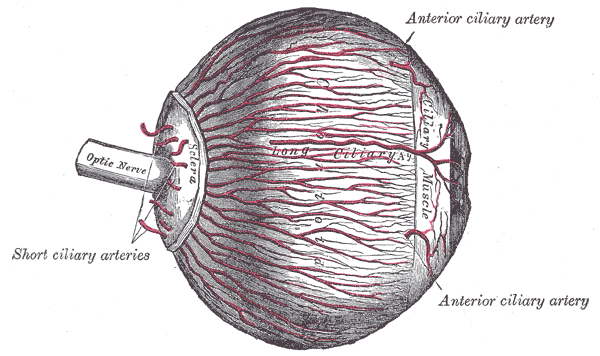
| The arteries of the choroid and iris. The greater part of the sclera has been removed. | |
| ICD-10 | G45.3 |
| ICD-9 | 362.34 |
| DiseasesDB | 501 |
| MedlinePlus | 000784 |
| MeSH | D020757 |
|
Amaurosis fugax Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Amaurosis fugax On the Web |
|
American Roentgen Ray Society Images of Amaurosis fugax |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Diagnostic Evaluation
Despite the temporary nature of the vision loss, those experiencing amaurosis fugax are usually advised to consult a physician immediately as it is a symptom that usually heralds serious vascular events, including stroke.[1][2] Restated, “because of the brief interval between the transient event and a stroke or blindness from temporal arteritis, the workup for transient monocular blindness should be undertaken without delay.” If the patient has no history of giant cell arteritis, the probability of vision preservation is high; however, the chance of a stroke reaches that for a hemispheric TIA. Therefore, investigation of cardiac disease is justified.[3]
A diagnostic evaluation should begin with the patient's history, followed by a physical exam, with particular importance being paid to the ophthalmic examination with regards to signs of ocular ischemia. When investigating amaurosis fugax, an ophthalmologic consult is absolutely warranted if available. Several concomitant laboratory tests should also be ordered to investigate some of the more common, systemic causes listed above, including a complete blood count, erythrocyte sedimentation rate, lipid panel, and blood glucose level. If a particular etiology is suspected based on the history and physical, additional relevant labs should be ordered.[3]
If laboratory tests are abnormal, a systemic disease process is likely, and, if the ophthalmologic examinaton is abnormal, ocular disease is likely. However, in the event that both of these routes of investigation yield normal findings, or an inadequate explanation, noninvasive duplex ultrasound studies are recommended to identify carotid artery disease. Most episodes of amaurosis fugax are the result of stenosis of the ipsilateral carotid artery.[4] With that being the case, researchers investigated how best to evaluate these episodes of vision loss, and concluded that for patients ranging from 36-74 years old, "...carotid artery duplex scanning should be performed...as this investigation is more likely to provide useful information than an extensive cardiac screening (ECG, Holler 24-hour monitoring and precordial echocardiography)."[4] Additionally, concomitant head CT or MRI imaging is also recommended to investigate the presence of a “clinically silent cerebral embolism.”[3]
If the results of the ultrasound and intracranial imaging are normal, “renewed diagnostic efforts may be made,” during which fluorescein angiography is an appropriate consideration. However, carotid angiography is not advisable in the presence of a normal ultrasound and CT.[5]
Treatment
If the diagnostic workup reveals a systemic disease process, directed therapies to treat that underlying etiology should be initiated. If the amaurosis fugax is caused by an atherosclerotic lesion, aspirin is indicated, and a carotid endarterectomy if the stenosis is surgically accessible. Generally, if the carotid artery is still patent, the greater the stenosis, the greater the indication for endarterectomy. "Amaurosis fugax appears to be a particularly favorable indication for carotid endarterectomy. Left untreated, this event carries a high risk of stroke; after carotid endarterectomy, which has a low operative risk, there is a very low postoperative stroke rate."[6] If the full diagnostic workup is completely normal, patient observation is recommended.[3]
Related Chapters
References
- ↑ Rothwell, Warlow. "Timing of TIA's preceding stroke: time window for prevention is very short." Neurology. 2005;64:817.
- ↑ 3.0 3.1 3.2 3.3
- ↑ 4.0 4.1 Smit, Ronald; G. Seerp Baarsma and Peter J. Koudstaal "The source of embolism in amaurosis fugax and retinal artery occlusion." International Ophthalmology. 1994 March;18(2):83-86. ISSN 0165-5701.
- ↑ Walsh J, Markowitz I, Kerstein MD. "Carotid endarterectomy for amaurosis fugax without angiography." Am J Surg. 1986 Aug;152(2):172-4. PMID 3526933.
- ↑ Bernstein EF, Dilley RB. "Late results after carotid endarterectomy for amaurosis fugax." J Vasc Surg. 1987 Oct;6(4):333-40. PMID 3656582.
Template:Diseases of the nervous system de:Retinaler Arterienverschluss