Bradycardia resident survival guide
| Bradycardia Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]: Associate Editor(s)-in-Chief: Ogheneochuko Ajari, MB.BS, MS [2]; Vidit Bhargava, M.B.B.S [3]
Overview
Bradycardia is defined as a sinus rhythm with a rate <60 beats per minute. A heart rate of <50 beats per minute is used as a working definition of bradycardia causing symptoms.[1]. The evaluation of bradycardia includes assessment of heart rhythm, symptoms and associated medical conditions. Symptomatic bradycardias are treated by removal of underlying causes, medications (e.g. the use of atropine) or insertion of temporary or permanent pacemaker. Nevertheless, some asymtomatic bradycardias may require treatment to prevent complications.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
Diagnosis
Shown below is an algorithm depicting the diagnosis of bradycardia
Characterize the symptoms: ❑ Palpitations Obtain a detailed history:
❑ Medication use ❑ Past medical history | |||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: ❑ Heart rate < 50/min
❑ Signs of poor perfusion
| |||||||||||||||||||||||||||||||||||||||||||||||||
Consider alternative diagnosis: ❑ Ventricular bigeminy ❑ Frequent premature ventricular contractions (PVCs) ❑ Atrial fibrillation ❑ Blocked premature atrial contractions (PACs) ❑ Cardiac tamponade | |||||||||||||||||||||||||||||||||||||||||||||||||
Order tests: First initial test 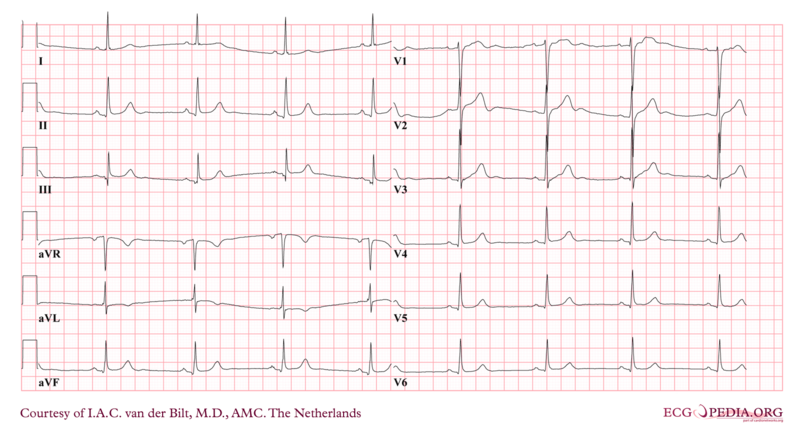 Other initial tests
❑ Exercise stress testing - For diagnoses of sick sinus syndrome and ischemic heart disease Laboratory tests Other Investigations | |||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Shown below is an algorithm depicting the treatment of bradycardia based on the 2010 AHA guidelines for cardiopulmonary resuscitation and emergency cardiovascular care.[1]
| Bradycardia confirmed Bradyarrhythmia seen with heart rate < 50/min | |||||||||||||||||||
Identify and treat underlying cause:
❑ Maintain patent airway; assist breathing as necessary | |||||||||||||||||||
Bradyarrhythmia causing symptoms? ❑ Hypotension? ❑ Acutely altered mental status? ❑ Signs of shock? ❑ Ischemic chest discomfort? ❑ Acute heart failure? | |||||||||||||||||||
| Yes | No | ||||||||||||||||||
| Primary treatment option Atropine
❑ Administer a first dose 0.5 mg IV bolus ❑ Repeat every 3-5 minutes ❑ Administer a maximum dose of 3 mg | ❑ Monitor and observe | ||||||||||||||||||
| Secondary treatment options If atropine ineffective: ❑ Administer dopamine infusion (2-10 mcg/kg/min) OR ❑ Administer epinephrine infusion (2-10 mcg/min) OR ❑ Proceed with transcutaneous pacing | |||||||||||||||||||
❑ Consult to Cardiologist ❑ Consider transvenous pacing | |||||||||||||||||||
Do's
- Prepare for transcutaneous pacing if perfusion is poor.
- Consider using sodium bicarbonate for severe metabolic acidosis.
- Use atropine with caution in the presence of myocardial ischemia because it increases oxygen demand and could worsen the ischemia.
Don'ts
- Do not delay pacing if the rhythm is Mobitz type II second degree block or third-degree AV block even if the patient is asymptomatic.
- Avoid using atropine in hypothermic patients with either bradycardia or Mobitz type II second degree AV block.
- Do not use atropine to treat bradycardia in cardiac transplant patients.
- Do not use atropine to treat Type II second degree and third degree heart blocks since their management requires transcutaneous/transvenous pacing.
References
- ↑ 1.0 1.1 Neumar, RW.; Otto, CW.; Link, MS.; Kronick, SL.; Shuster, M.; Callaway, CW.; Kudenchuk, PJ.; Ornato, JP.; McNally, B. (2010). "Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S729–67. doi:10.1161/CIRCULATIONAHA.110.970988. PMID 20956224. Unknown parameter
|month=ignored (help)