Wernicke-Korsakoff syndrome
For patient information, click here
| Wernicke-Korsakoff syndrome | |
 | |
|---|---|
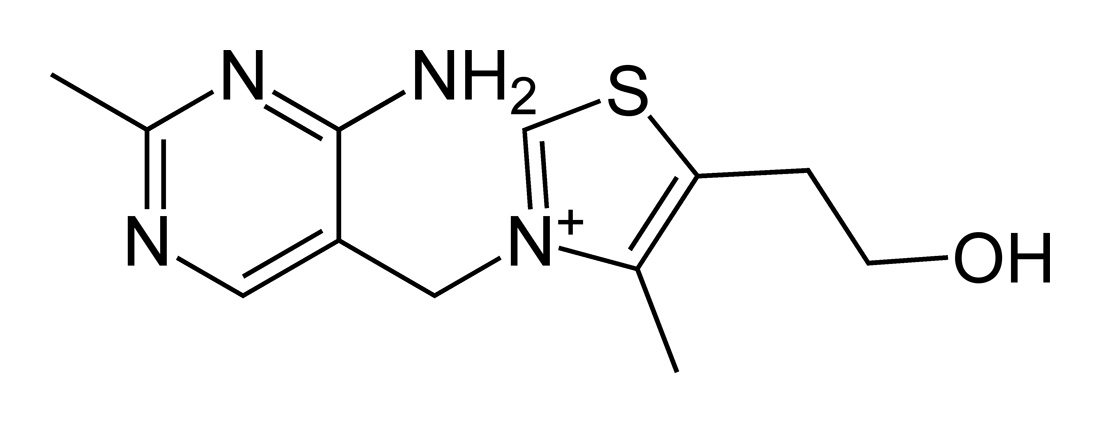
| Thiamine |
|
Wernicke-Korsakoff Syndrome Microchapters |
|
Differentiating Wernicke-Korsakoff Syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Wernicke-Korsakoff syndrome On the Web |
|
American Roentgen Ray Society Images of Wernicke-Korsakoff syndrome |
|
Directions to Hospitals Treating Wernicke-Korsakoff syndrome |
|
Risk calculators and risk factors for Wernicke-Korsakoff syndrome |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Aditya Govindavarjhulla, M.B.B.S. [3]
Synonyms and keywords: Alcohol induced encephalopathy; transketolase defect; Korsakoff psychosis; alcoholic encephalopathy
Overview
Wernicke-Korsakoff syndrome is a is a degenerative brain disorder cause by thiamine deficiency. This is usually secondary to alcohol abuse. Although Wernicke's and Korsakoff's may appear to be two different disorders, they are generally considered to be different stages of the same disorder, which is called Wernicke-Korsakoff syndrome(WKS). Wernicke's encephalopathy represents the "acute" phase of the disorder, and Korsakoff's amnesic syndrome represents the "chronic" phase.
Historical Perspective
The syndrome is a combined manifestation of two eponymous disorders, Korsakoff's Psychosis and Wernicke's encephalopathy, named for Drs. Sergei Korsakoff and Carl Wernicke.
Pathophysiology
Wernicke-Korsakoff syndrome results from thiamin deficiency. It is generally agreed that Wernicke's encephalpathy results from severe acute deficiency of thiamine (Vitamin B1), whilst Korsakoff's psychosis results from chronic deficiency of thiamin. The metabolically active form of thiamine is thiamine diphosphate which plays a major role as a cofactor in glucose metabolism. The enzymes which are dependent on thiamin diphosphate are associated with the TCA Cycle and catalyse the oxidation of pyruvate,alphaketoglutarate and branched chain amino acids. Thus, anything that encourages glucose metabolism will exacerbate an existing clinical or sub-clinical thiamine deficiency. When Wernicke's encephalopathy accompanies Korsakoff's syndrome, the combination is called the Wernicke-Korsakoff syndrome. Korsakoff's is a continuum of Wernicke's encephalopathy, though a recognised episode of Wernicke's is not always obvious.
There is an unreplicated study that has associated susceptiblity to this syndrome with a hereditary deficiency of transketolase, an enzyme involved in thiamine metabolism.[1]
Pathology
Wernicke-Korsakoff syndrome in alcoholics especially is associated with atrophy[2] of specific regions of the brain, especially the mamillary bodies. Other regions include the anterior region of the thalamus (accounting for amnesic symptoms), the medial dorsal thalamus, the basal forebrain, and median and dorsal raphe nuclei.[3] Korsakoff's involves neuronal loss, that is, damage to neurons; gliosis which is a result of damage to supporting cells of the central nervous system; and hemorrhage or bleeding in mammillary bodies. Damage to the dorsomedial nucleus of the thalamus is also associated with this disorder. Frequently, for unknown reasons, patients with Korsakoff's psychosis will exhibit marked degeneration of the mamillary bodies. The mechanism of this degeneration is unknown, but it supports current neurological theory that the mamillary bodies play a role in various "memory circuits" within the brain. An example of a memory circuit is the Papez circuit.
Causes
- Malnourishment
- Chronic alcoholism
- Prolonged intravenous therapy
- Gastric stapling
- ICU stays
- Chronic intake of polished rice
- Large dose of glucose in thiamine deficient individuals [4]
Epidemiology and Demography
- In France, a country with one of the highest per capita consumptions of alcohol, the prevalence of the WKS was found to be only 0.4% in a small retrospective autopsy study.[5]
- Prevalence rates in Australia are highest 2.8%.[6]
- Per capita consumption of alcohol is not corelating with the prevalence of the syndrome in many countries.[7]
Age
- It is more common in middle aged persons.
Gender
- It is more common in men.
Natural History, Complications and Prognosis
Complications
- Alcohol withdrawal
- Difficulty with personal or social interaction
- Injury caused by falls
- Permanent alcoholic neuropathy
- Permanent loss of thinking skills
- Permanent loss of memory
- Shortened life span
Prognosis
- Without treatment, Wernicke-Korsakoff syndrome gets steadily worse and can be life threatening.
- With treatment, symptoms can be controlled (such as uncoordinated movement and vision difficulties) from getting worse.
- Some symptoms, especially the loss of memory and thinking skills, may be permanent. Other disorders related to alcohol abuse may also occur.
Diagnosis
Symptoms
- Lethargy
- Confusion
- Anterograde amnesia
- Retrograde amnesia
- Confabulation
- Meager content in conversation
- Lack of insight
- Apathy - the patients lose interest in things quickly and generally appear indifferent to change
- Weakness
Physical Examination
Appearance of the Patient
- Lethargic and disturbed consciousness
Vital Signs
- Fast pulse (heart rate)
- Low blood pressure
- Low body temperature
Eyes
Abdomen
- Organomegaly may be noticed
Neurologic
Laboratory Findings
Electrolyte and Biomarker Studies
- Serum electrolytes
- Serum albumin (relates to person's general nutrition)
- Serum vitamin B1 levels
- Transketolase activity in red blood cells (reduced in people with thiamine deficiency)
MRI
- MRI may show changes in the brain tissue - atrophy of mammilary body
Diagnosis of Wernicke-Korsakoff syndrome is by clinical impression and can sometimes be confirmed with formal neuropsychological assessment. Wernicke's encephalopathy typically presents with ataxia and nystagmus, and Korsakoff's psychosis with anterograde and retrograde amnesia and confabulation upon relevant lines of questioning.
Treatment
Treatment consists of reversing the thiamine deficiency by giving supplemental thiamine, usually by starting with an initial intravenous or intramuscular dose followed by supplemental oral doses. It is important to start the thiamine treatment before giving any glucose as the encephalopathy will be worsened by the glucose. (Glucose administration promotes dehydrogenation of pyruvate, a biochemical reaction which consumes thiamine.) By the time amnesia and psychosis have occurred, complete recovery is unlikely.
Prevention
- Not drinking alcohol or drinking in moderation and getting enough nutrition reduce the risk of developing Wernicke-Korsakoff syndrome.
- Thiamine supplements and a good diet may reduce the chance of getting this condition, but do not eliminate the risk.
References
- ↑ Nixon P, Kaczmarek M, Tate J, Kerr R, Price J (1984). "An erythrocyte transketolase isoenzyme pattern associated with the Wernicke-Korsakoff syndrome". Eur J Clin Invest. 14 (4): 278–81. PMID 6434322.
- ↑ Kolb & Whishaw: Fundamentals of Human Neuropsychology, 2003, pages 473-473
- ↑ Mann K, Agartz I, Harper C, Shoaf S; et al. (2001). "Neuroimaging in alcoholism: ethanol and brain damage". Alcohol Clin Exp Res. 25 (5 Suppl ISBRA): 104S–109S. PMID 11391058.
- ↑ Zimitat C, Nixon P, (2000). "Glucose loading precipitates encephalopathy in thiamine-deficient rats". Metabolic Brain Disease. 14 (1): 1–10.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/7596325
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/7596325
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/7596325
de:Wernicke-Korsakow-Syndrom is:Wernicke-Korsakoff heilkenni nl:Syndroom van Wernicke sq:Sindroma Wernicke-Korsakoff