| Classification of pain in the abdomen based on etiology
|
Disease
|
Clinical manifestations
|
Diagnosis
|
Comments
|
| Symptoms
|
Signs
|
| Abdominal Pain
|
Fever
|
Rigors and chills
|
Jaundice
|
Diarrhea
|
GI Bleed
|
Hypo-
tension
|
Guarding
|
Rebound Tenderness
|
Bowel sounds
|
Lab Findings
|
Imaging
|
| Abdominal causes
|
Inflammatory causes
|
Pancreato-biliary disorders
|
Acute suppurative cholangitis
|
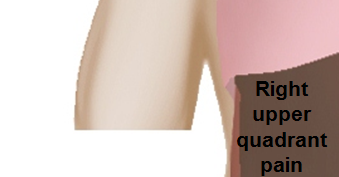
RUQ
|
+
|
+
|
+
|
−
|
−
|
+
|
+
|
+
|
N
|
|
Ultrasound shows biliary dilatation/stents/tumor
|
Septic shock occurs with features of SIRS
|
| Acute cholangitis
|
RUQ
|
+
|
−
|
+
|
−
|
−
|
−
|
−
|
−
|
N
|
|
Ultrasound shows biliary dilatation/stents/tumor
|
Biliary drainage (ERCP) + IV antibiotics
|
| Acute cholecystitis
|
RUQ
|
+
|
−
|
+
|
−
|
−
|
−
|
−
|
−
|
Hypoactive
|
|
Ultrasound shows gallstone and evidence of inflammation
|
Murphy’s sign
|
| Acute pancreatitis
|
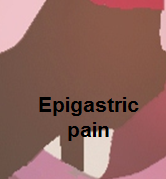
Epigastric
|
+
|
−
|
±
|
−
|
−
|
±
|
−
|
−
|
N
|
|
Ultrasound shows evidence of inflammation
|
Pain radiation to back
|
| Chronic pancreatitis
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Primary biliary cirrhosis
|
RUQ/Epigastric
|
−
|
−
|
+
|
−
|
+ in late presentation
|
−
|
−
|
−
|
N
|
- Increased AMA level, abnormal LFTs
|
|
|
| Primary sclerosing cholangitis
|
RUQ
|
+
|
−
|
+
|
−
|
−
|
−
|
−
|
−
|
N
|
|
ERCP and MRCP shows
- Multiple segmental strictures
- Mural irregularities
- Biliary dilatation and diverticula
- Distortion of biliary tree
|
The risk of cholangiocarcinoma in patients with primary sclerosing cholangitis is 400 times higher than the risk in the general population.
|
| Cholelithiasis
|
RUQ/Epigastric
|
±
|
−
|
±
|
−
|
−
|
−
|
−
|
−
|
N to hyperactive for dislodged stone
|
|
Ultrasound shows gallstone
|
Fatty food intolerance
|
| Gastric causes
|
Peptic ulcer disease
|
Diffuse
|
±
|
−
|
−
|
−
|
|
+ in perforated
|
+
|
+
|
N
|
- Ascitic fluid
- LDH > serum LDH
- Glucose < 50mg/dl
- Total protein > 1g/dl
|
Air under diaphragm in upright CXR
|
Upper GI endoscopy for diagnosis
|
| Gastritis
|
Epigastric
|
±
|
−
|
−
|
−
|
+ in chronic gastritis
|
−
|
−
|
−
|
N
|
H.pylori infection diagnostic tests
|
Endoscopy
|
H.pylori gastritis guideline recommendation
|
| Gastroesophageal reflux disease
|
Epigastric
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
N
|
Esophageal manometry
|
Gastric emptying studies
|
Endoscopy for alarm signs
|
| Gastric outlet obstruction
|
Epigastric
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
Hyperactive
|
|
|
Succussion splash
|
| Gastrointestinal perforation
|
Diffuse
|
+
|
±
|
±
|
−
|
+, depends on site
|
+
|
+
|
±
|
Hyperactive/hypoactive
|
|
Air under diaphragm in upright CXR
|
Hamman's sign
|
| Dumping syndrome
|
Lower and then diffuse
|
−
|
−
|
|
|
|
|
|
|
|
|
|
|
| Intestinal causes
|
Acute appendicitis
|
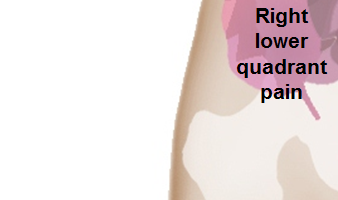
Starts in epigastrium, migrates to RLQ
|
+
|
+in pyogenic appendicitis
|
−
|
−
|
−
|
+ in perforated appendicitis
|
+
|
+
|
Hypoactive
|
|
Ultrasound shows evidence of inflammation
|
Nausea & vomiting, decreased appetite
|
| Acute diverticulitis
|
LLQ
|
+
|
±
|
−
|
±
|
Hematochezia
|
+ in perforated diverticulitis
|
+
|
+
|
Hypoactive
|
|
CT scan and ultrasound shows evidence of inflammation
|
History of constipation
|
| Inflammatory bowel disease
|
Diffuse
|
±
|
−
|
±
|
±
|
Hematochezia
|
−
|
−
|
−
|
N/ Hyperactive
|
|
String sign on abdominal x-ray in Crohn's disease
|
Extra intestinal findings:
|
| Irritable bowel syndrome
|
Diffuse
|
±
|
−
|
−
|
+
|
−
|
−
|
−
|
−
|
N
|
Tests done to exclude other diseases as it diagnosis of exclusion
|
Tests done to exclude other diseases as it diagnosis of exclusion
|
Symptomatic treatment
|
| Whipple's disease
|
Diffuse
|
±
|
−
|
±
|
+
|
−
|
±
|
−
|
−
|
N
|
|
Endoscopy is used to confirm diagnosis.
Images used to find complications
|
Extra intestinal findings:
|
| Toxic megacolon
|
Diffuse
|
+
|
−
|
−
|
+
|
−
|
+
|
±
|
−
|
Hypoactive
|
|
CT scan shows:
Ultrasound shows:
- Loss of haustra coli of the colon
- Hypoechoic and thickened bowel walls with irregular internal margins in the sigmoid and descending colon
- Prominent dilation of the transverse colon (>6 cm)
- Insignificant dilation of ileal bowel loops (diameter >18 mm) with increased intraluminal gas and fluid
|
|
| Tropical sprue
|
Diffuse
|
+
|
−
|
−
|
+
|
−
|
−
|
−
|
−
|
N
|
|
Barium studies show dilation and edema of mucosal folds
|
Steatorrhea- 10-40 g/day (Normal=5 g/day)
|
| Celiac disease
|
Diffuse
|
−
|
−
|
−
|
+
|
−
|
−
|
−
|
−
|
Hyperactive
|
|
USG
- Bull’s eye or target pattern
- Pseudokidney sign
|
Gluten allergy
|
| Infective colitis
|
Diffuse
|
+
|
−
|
−
|
+
|
Hematochezia
|
+ in fulminant colitis
|
±
|
±
|
Hyperactive
|
|
CT scan
- Bowel wall thickening
- Edema
|
|
| Hepatic causes
|
Viral hepatitis
|
RUQ
|
+
|
−
|
+
|
+ in Hep A and E
|
−
|
+ in fulminant hepatitis
|
+in acute
|
+
|
N
|
- Abnormal LFTs
- Viral serology
|
USG
|
Hep A and E have fecoral route of transmission and Hep B and C transmits via blood transfusion and sexual contact.
|
| Liver masses
|
RUQ
|
+
|
+ in Liver abscess
|
±
|
−
|
+ in Hepatocellular carcinoma
|
+ in sepsis
|
+ in Liver abscess
|
+ in Liver abscess
|
N
|
|
USG
|
|
| Budd-Chiari syndrome
|
RUQ
|
±
|
−
|
±
|
−
|
+ in liver failure leading to varices
|
−
|
−
|
−
|
N
|
|
| Findings on CT scan suggestive of Budd-Chiari syndrome include:
|
|
Ascitic fluid examination shows:
|
| Hemochromatosis
|
RUQ
|
−
|
−
|
−
|
−
|
+ in cirrhotic patients
|
−
|
−
|
−
|
N
|
- >60% TS
- >240 μg/L SF
- Raised LFT
Hyperglycemia
|
Ultrasound shows evidence of cirrhosis
|
Extra intestinal findings:
- Hyperpigmentation
- Diabetes mellitus
- Arthralgia
- Impotence in males
- Cardiomyopathy
- Atherosclerosis
- Hypopituitarism
- Hypothyroidism
- Extrahepatic cancer
- Prone to specific infections
|
| Cirrhosis
|
RUQ
|
−
|
−
|
+
|
−
|
varices
|
+
|
−
|
−
|
N
|
|
USG
|
- Stigmata of liver disease
- Cruveilhier- Baumgarten murmur
|
| Peritoneal causes
|
Spontaneous bacterial peritonitis
|
Diffuse
|
+
|
+
|
+ in cirrhotic patients
|
+
|
−
|
±
|
+
|
+
|
Hypoactive
|
- Ascitic fluid PMN>250 cells/mm³
- Culture: Positive for single organism
|
Ultrasound for evaluation of liver cirrhosis
|
|
| Hollow Viscous Obstruction
|
Small intestine obstruction
|
Diffuse
|
−
|
−
|
−
|
−
|
−
|
−
|
+
|
±
|
Hyperactive then absent
|
Leukocytosis
|
Abdominal X ray
|
Nausea & vomiting associated with constipation, abdominal distention
|
| Volvulus
|
Diffuse
|
−
|
−
|
−
|
−
|
−
|
−
|
+
|
−
|
Hypoactive
|
Leukocytosis
|
CT scan and abdominal X ray
|
Nausea & vomiting associated with constipation, abdominal distention
|
| Biliary colic
|
RUQ
|
−
|
−
|
+
|
−
|
−
|
−
|
−
|
−
|
N
|
Increased bilirubin and alkaline phosphatase
|
Ultrasound
|
Nausea & vomiting
|
| Renal colic
|
Flank pain
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
−
|
N
|
Hematuria
|
CT scan and ultrasound
|
Colicky abdominal pain associated with nausea & vomiting
|
| Vascular Disorders
|
Ischemic causes
|
Mesenteric ischemia
|
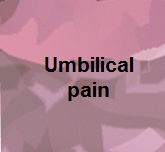
Periumbilical
|
±
|
−
|
−
|
+
|
Hematochezia
|
±
|
−
|
−
|
Hyperactive
|
Leukocytosis and lactic acidosis
|
CT scan
|
Nausea & vomiting, normal physical examination
|
| Acute ischemic colitis
|
Diffuse
|
±
|
±
|
−
|
+
|
Massive
|
|
+
|
+
|
Hyperactive then absent
|
Leukocytosis
|
CT scan
|
Nausea & vomiting
|
| Hemorrhagic causes
|
Ruptured abdominal aortic aneurysm
|
Diffuse
|
−
|
−
|
−
|
−
|
Massive
|
+
|
−
|
−
|
N
|
Normal
|
CT scan
|
Unstable hemodynamics
|
| Intra-abdominal or retroperitoneal hemorrhage
|
Diffuse
|
−
|
−
|
−
|
−
|
Massive
|
+
|
−
|
−
|
N
|
Anemia
|
CT scan
|
History of trauma
|
| Gynaecological Causes
|
Tubal causes
|
Torsion of the cyst
|
RLQ / LLQ
|
−
|
−
|
−
|
−
|
−
|
|
±
|
±
|
N
|
Increased ESR and CRP
|
Ultrasound
|
Sudden onset sever pain with nausea and vomiting
|
| Acute salpingitis
|
RLQ / LLQ
|
+
|
±
|
−
|
−
|
−
|
−
|
±
|
±
|
N
|
Leukocytosis
|
Pelvic ultrasound
|
Vaginal discharge
|
| Cyst rupture
|
RLQ / LLQ
|
−
|
−
|
−
|
−
|
−
|
+
|
±
|
±
|
N
|
Increased ESR and CRP
|
Ultrasound
|
Sudden onset sever pain with nausea and vomiting
|
| Pregnancy
|
Ruptured ectopic pregnancy
|
RLQ / LLQ
|
−
|
−
|
−
|
−
|
−
|
+
|
−
|
−
|
N
|
Positive pregnancy test
|
Ultrasound
|
History of missed period and vaginal bleeding
|
| Extra-abdominal causes
|
Pulmonary disorders
|
Pleural empyema
|
RUQ/Epigastric
|
+
|
±
|
−
|
−
|
−
|
−
|
−
|
−
|
N
|
|
|
|
| Cardiovascular disorders
|
Myocardial Infarction
|
Epigastric
|
−
|
−
|
−
|
−
|
−
|
+ in cardiogenic shock
|
−
|
−
|
N
|
|
|
|