Syncope resident survival guide: Difference between revisions
No edit summary |
|||
| Line 47: | Line 47: | ||
==Classification== | ==Classification== | ||
{| class="wikitable" width= 85% border="1" | |||
!width="250pt"|Cardiovascular syncope !!width="250pt"|Orthostatic hypotension !!width="250pt"|Reflex syncope | |||
|- | |||
| Arrhythmias (bradycardia or tachycardia) <br> *Structural heart disease <br> *Drug-induced arrhythmyas || *Primary autonomic failure <br> *Secondary autonomic failure <br> *Drug-induced <br> *Hypovolemia || *Vasovagal <br> *Situational <br> *Carotid sinus syncope | |||
|} | |||
==Diagnosis== | ==Diagnosis== | ||
Revision as of 18:28, 20 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Karol Gema Hernandez, M.D. [2]; Alejandro Lemor, M.D. [3]
| Syncope Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Classification |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Syncope is the transient loss of consciousness (LOC) due to cerebral hypoperfusion and it is characterized by a rapid onset, a short duration and a spontaneous complete recovery. It is important to identify the cause of the syncope and recognize high risk patients (those with structural heart disease or abnormal EKG). The initial management depends on the etiology of the syncope (reflex, orthostatic hypotension or cardiovascular).
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Aortic stenosis
- Arrhythmia
- Medications (vasodilators, diuretics, antiarrhythmics, antipsychotics)
- Orthostatic hypotension
- Vagal stimulation
- Vertebrobasilar insufficiency[2]
Classification
| Cardiovascular syncope | Orthostatic hypotension | Reflex syncope |
|---|---|---|
| Arrhythmias (bradycardia or tachycardia) *Structural heart disease *Drug-induced arrhythmyas |
*Primary autonomic failure *Secondary autonomic failure *Drug-induced *Hypovolemia |
*Vasovagal *Situational *Carotid sinus syncope |
Diagnosis
Shown below is an algorithm summarizing the diagnostic approach to syncope based on the 2009 ESC Guidelines for the Diagnosis and Management of Syncope.[3]
Abbreviations: TIA: Transient ischemic attack; EEG: Electroencephalography; HF: Heart failure; AF: Atrial fibrillation; SVT: Supraventricular tachycardia; VT: Ventricular tachycardia; MI: Myocardial infarction; BBB: Bundle branch block
Characterize symptoms ❑ Loss of consciousness (LOC)
❑ Prodrome:
❑ Chest pain (suggestive of cardiovascular syncope)
❑ Position prior to LOC:
Inquire about medications intake: Obtain a detailed past medical history:
❑ Neurological diseases: ❑ Recent trauma | |||||||||||||||||||||||||||||||
Identify possible triggers: (suggestive of vasovagal syncope) ❑ Emotional stress | |||||||||||||||||||||||||||||||
Examine the patient
❑ Vitals
❑ Lungs ❑ Heart
❑ Neurologic
| |||||||||||||||||||||||||||||||
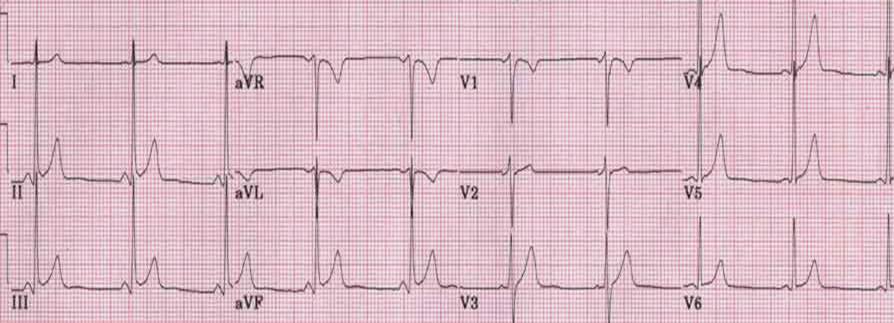
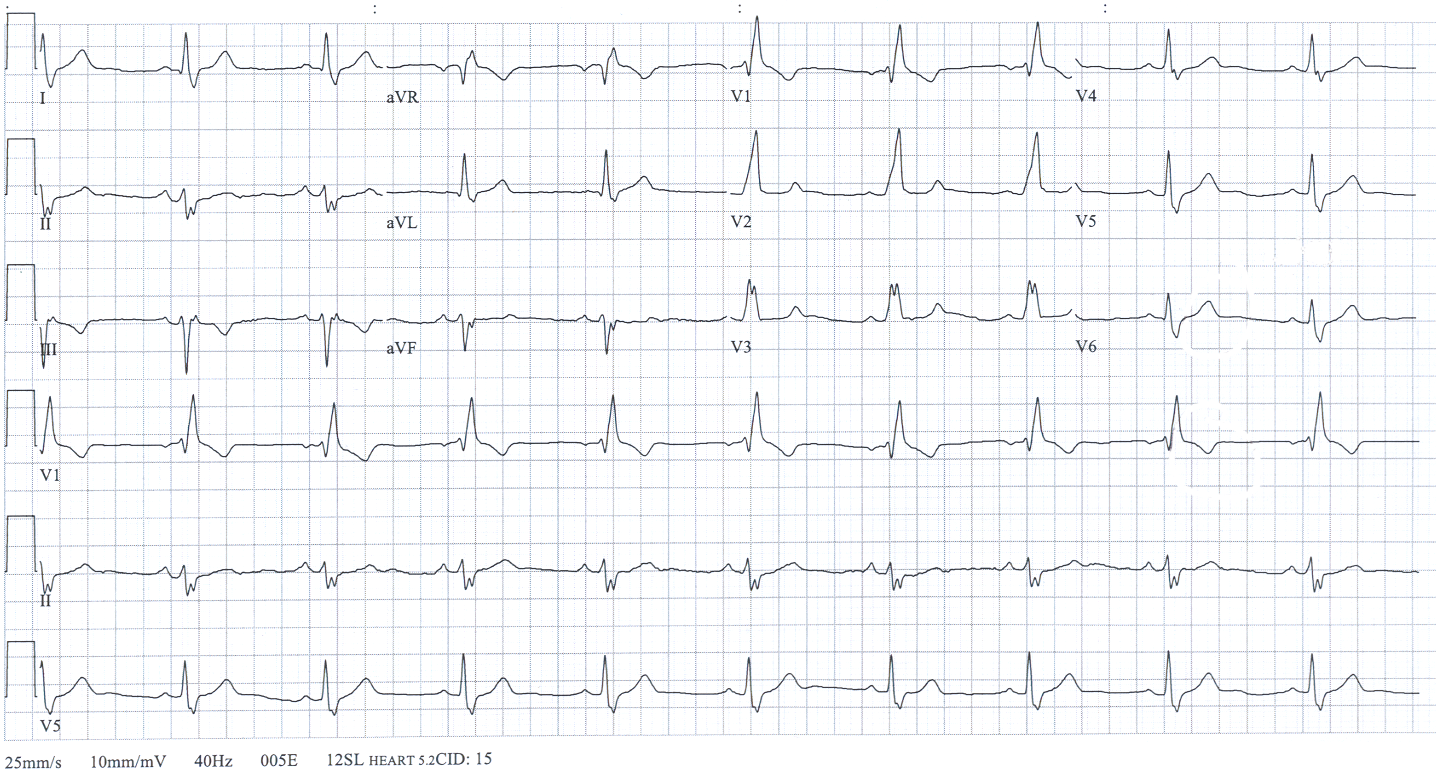
Order labs and tests ❑ EKG (most important initial test) ❑ Glucose (rule out hypoglycemia)
| |||||||||||||||||||||||||||||||
Order imaging studies
To rule out structural heart disease or valvular disease: ❑ Head CT | |||||||||||||||||||||||||||||||
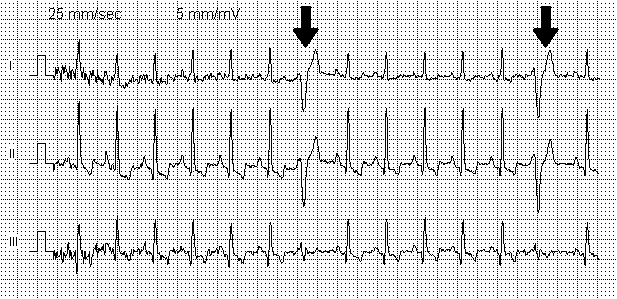
Abnormal EKG
| Normal EKG
Rule out other possible diagnoses:
| ||||||||||||||||||||||||||||||
Cardiovascular syncope
Additional findings:
❑ Cardiac evaluation:
❑ Presence of structural hearth disease
❑ Occurred during exertion | Orthostatic hypotension
Additional findings:
❑ Cardiac evaluation: palpitations ❑ After standing up or prolonged standing ❑ Start of new antihypertensive drug ❑ Presence of autonomic neuropathy | Reflex Syncope Additional findings:
❑ If present, order a head CT or MRI ❑ EKG findings: tachycardia, normal or bradycardia | |||||||||||||||||||||||||||||||||
Treatment
Shown below is an algorithm summarizing the therapeutic approach to syncope based on the 2009 ESC Guidelines for the Diagnosis and Management of Syncope. [3]
Abbreviations: AF: Atrial fibrillation: SVT: Supraventricular tachycardia ; VT:Ventricular tachycardia: MI: Myocardial infarction; BBB: Bundle branch block
| ❑ Determine the etiology of the syncope | |||||||||||||||||||||||||||
Cardiovascular | Reflex | ||||||||||||||||||||||||||
Depends on the cause of the arrhythmia: ❑ Schedule for cardiac pacing surgery in patients with sinus node disease, Mobitz II AV block, BBB with positive electrophysiological study ❑ Schedule for catheter ablation in patients with SVT and VT in absence of structural hearth disease ❑ Administer antiarrhythmic drug therapy in patients with AF, failed catheter ablation ❑ Schedule for implantable cardioverter defibrillator surgery in patients with VT with heart disease, electrophysiological study induced VT in patients with previous MI, VT and inherited cardiomyopathy | ❑ Adequate hydration and salt intake ❑ Adjunctive therapy if needed:
Contraindicated in severe heart disease, acute renal failure, pheochromocytoma, severe hypertension or thyrotoxicosis
| ❑ Explain diagnosis, provide reassurance ❑ Explain risk of recurrence and avoidance of triggers ❑ Isometric physical counterpressure maneuvers (PCM) in patients with prodrome:
| |||||||||||||||||||||||||
Do's
- Tilt testing is indicated to demonstrate susceptibility to reflex syncope.
- Tilt testing should be considered to discriminate between reflex and OH syncope.
- Perform tilt testing if the cause of syncope is a psychiatric disease.
- Tilt testing may be considered for differentiating syncope with jerking movements from epilepsy.
- If syncope happened after standing up position, there should be documentation with active standing or tilt testing in order to diagnose orthostatic hypotension.
- Perform carotid sinus massage if patient >40 years with syncope of unknown etiology after initial evaluation.
- If multiple unexplained falls; perform tilt testing.
- Consider implantable loop recorder before embarking on cardiac pacing in patients with suspected or confirmed reflex syncope presenting with frequent or traumatic syncopal episodes.
- Evaluate neurologically if syncope is due to autonomic failure, to evaluate underlying disease.
Don'ts
- Don't perform carotid sinus massage in patients with previous TIA or stroke within the past 3 months and in patients with carotid sinus bruits (except if carotid sinus Doppler studies excluded significant stenosis).
- Don't use tilt testing for assessment of treatment.
- Don't perform isoproterenol tilt test in patients with ischemic heart disease.
- Don't use adenosine stress test as a diagnostic test to select patients for cardiac pacing, owing to lack of correlation with spontaneous syncope.
- Don't perform electrophysiologic study if there is already indication for implantable cardioverter defibrillator in patients with ischemic heart with suspected arrhythmic cause.
- Don't perform electrophysiologic study in patients with normal EKG, no heart disease, and no palpitations.
References
- ↑ Khoo, C.; Chakrabarti, S.; Arbour, L.; Krahn, AD. (2013). "Recognizing life-threatening causes of syncope". Cardiol Clin. 31 (1): 51–66. doi:10.1016/j.ccl.2012.10.005. PMID 23217687. Unknown parameter
|month=ignored (help) - ↑ Kapoor, WN. (2000). "Syncope". N Engl J Med. 343 (25): 1856–62. doi:10.1056/NEJM200012213432507. PMID 11117979. Unknown parameter
|month=ignored (help) - ↑ 3.0 3.1 Task Force for the Diagnosis and Management of Syncope. European Society of Cardiology (ESC). European Heart Rhythm Association (EHRA). Heart Failure Association (HFA). Heart Rhythm Society (HRS). Moya A; et al. (2009). "Guidelines for the diagnosis and management of syncope (version 2009)". Eur Heart J. 30 (21): 2631–71. doi:10.1093/eurheartj/ehp298. PMC 3295536. PMID 19713422 Check
|pmid=value (help).